Medication Safety: Protect Yourself from Dangerous Interactions and Errors
When you take a pill, you expect it to help—not hurt. But medication safety, the practice of using drugs correctly to avoid harm while achieving therapeutic benefit. Also known as drug safety, it’s not just about following labels—it’s about understanding what’s hidden in your medicine cabinet. Every year, hundreds of thousands of people end up in emergency rooms because of preventable mistakes. Some mix painkillers with blood thinners. Others take antihistamines after a drink. A few don’t realize their calcium-fortified orange juice is blocking their thyroid medicine. These aren’t rare accidents. They’re common, predictable, and often avoidable.
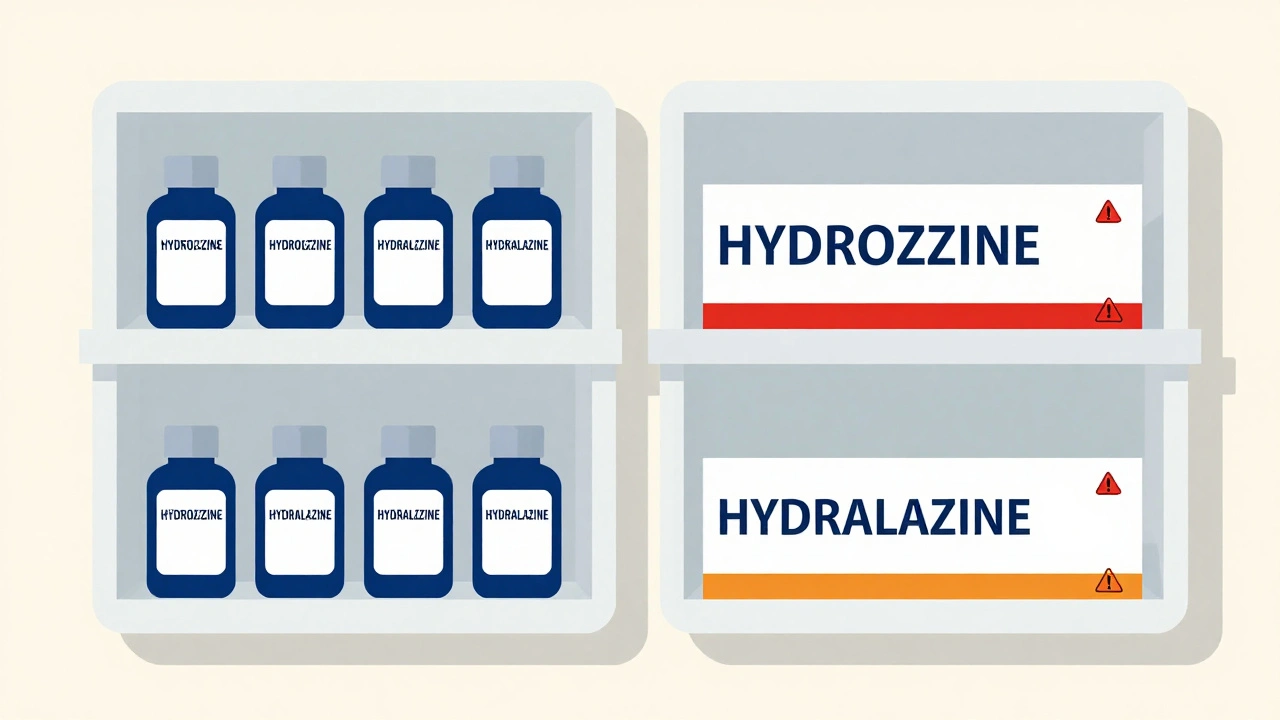
True medication safety, the practice of using drugs correctly to avoid harm while achieving therapeutic benefit. Also known as drug safety, it’s not just about following labels—it’s about understanding what’s hidden in your medicine cabinet. isn’t just about pills. It’s about knowing how your body reacts to combinations you didn’t even think mattered. drug interactions, when two or more medications affect each other’s strength, timing, or effect in the body. Also known as medication interactions, it’s why taking ibuprofen with warfarin can cause internal bleeding, or why garlic supplements increase bleeding risk even if you’re not on a blood thinner. medication errors, mistakes in prescribing, dispensing, or taking drugs that lead to harm. Also known as drug mistakes, it’s why people accidentally overdose on acetaminophen by taking three different cold medicines at once—each with the same active ingredient. And then there’s adverse drug reactions, unintended, harmful effects from medications that occur at normal doses. Also known as side effects, these aren’t always listed on the label. Some are rare, like tendon rupture from antibiotics, or liver failure from herbal supplements. Others are subtle—like your thyroid levels creeping up after you start a new stomach acid pill.
Generic drugs aren’t cheap imitations—they’re FDA-approved copies with the same active ingredients. But switching to them without checking your labs? That’s where safety breaks down. People on thyroid meds, seizure drugs, or blood thinners need to track their symptoms and lab results after a switch. The same goes for new biosimilars or when a drug shortage forces a change. Medication safety isn’t a one-time task. It’s an ongoing habit: reading labels, asking questions, keeping a list of everything you take, and knowing when to call your doctor. You don’t need to be a pharmacist. You just need to pay attention.
Below, you’ll find real-world guides that cut through the noise. No fluff. No theory. Just what you need to know to avoid the most common—and dangerous—mistakes people make every day with their meds.