Proton Pump Inhibitors: What They Are, How They Work, and What You Need to Know
When you hear proton pump inhibitors, a class of drugs that block acid production in the stomach to treat heartburn and ulcers. Also known as PPIs, they’re among the most prescribed medications in the world—used by millions daily for conditions like GERD, peptic ulcers, and acid reflux. But they’re not harmless. While they work well short-term, long-term use can lead to side effects like nutrient deficiencies, bone loss, and even kidney problems. Many people take them without knowing why—or how long they should.
These drugs target the proton pumps in stomach lining cells, the final step in acid production. By shutting those pumps down, they reduce acid more effectively than older meds like H2 blockers. Common ones include omeprazole (Prilosec), esomeprazole (Nexium), lansoprazole (Prevacid), and pantoprazole (Protonix). You can get some over the counter, but that doesn’t mean they’re safe for daily, long-term use without medical guidance. The FDA has warned about risks like low magnesium, Clostridium difficile infections, and rebound acid hypersecretion when people stop suddenly.
People often reach for PPIs because heartburn feels unbearable, but not all stomach discomfort is caused by excess acid. Some cases are linked to diet, stress, or even a weak lower esophageal sphincter. And while PPIs help with symptoms, they don’t fix the root cause. That’s why doctors recommend using the lowest dose for the shortest time possible. If you’ve been on one for over a year, it’s worth asking if you still need it—or if lifestyle changes, antacids, or H2 blockers could work better.
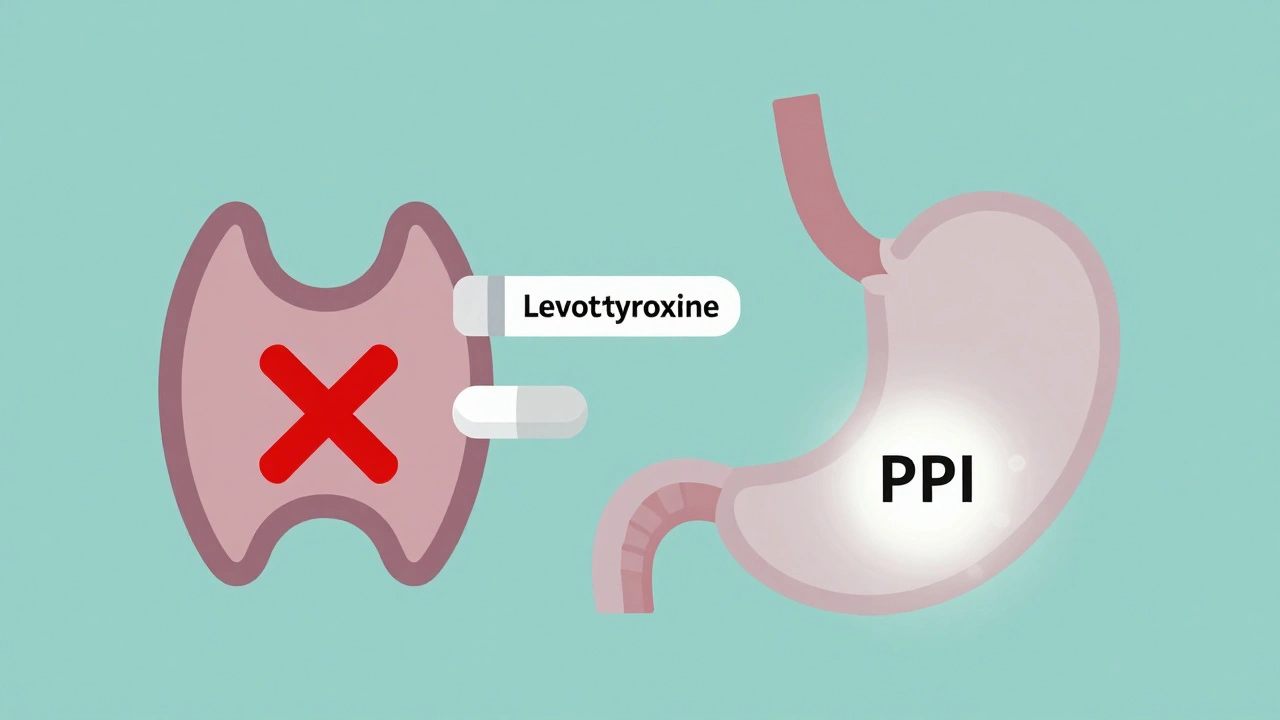
What’s interesting is how these drugs connect to other common concerns. For example, calcium-fortified juices can interfere with how well some PPIs work, and mixing them with blood thinners or certain antibiotics can raise bleeding or infection risks. Even something as simple as taking them at the wrong time of day—like after a meal instead of before—can cut their effectiveness. And while they’re not directly linked to mood stabilizers or liver toxins like kava, the way your body handles multiple medications at once matters. If you’re on other prescriptions, especially ones with narrow therapeutic windows, PPIs can change how those drugs behave in your system.
There’s also growing awareness that many people are prescribed PPIs unnecessarily—sometimes for mild symptoms that would resolve on their own, or as a preventive measure after surgery or during hospital stays. Studies show up to 70% of long-term users could safely stop with proper guidance. The key isn’t to avoid them entirely, but to use them wisely. Know why you’re taking them. Track how long you’ve been on them. Talk to your doctor before quitting cold turkey.
Below, you’ll find real-world insights from people who’ve used these drugs, warnings about hidden risks, and practical advice on managing acid-related conditions without relying on daily pills. Whether you’re just starting out or have been taking PPIs for years, there’s something here that can help you make smarter choices about your stomach—and your health.