Levothyroxine and Proton Pump Inhibitors: What You Need to Know About Absorption Interactions
 Dec, 4 2025
Dec, 4 2025
Levothyroxine-PPI Dose Adjustment Calculator
Calculate Your Levothyroxine Adjustment
Based on 2023 clinical data showing PPIs reduce levothyroxine absorption by 15-20% in hypothyroid patients.
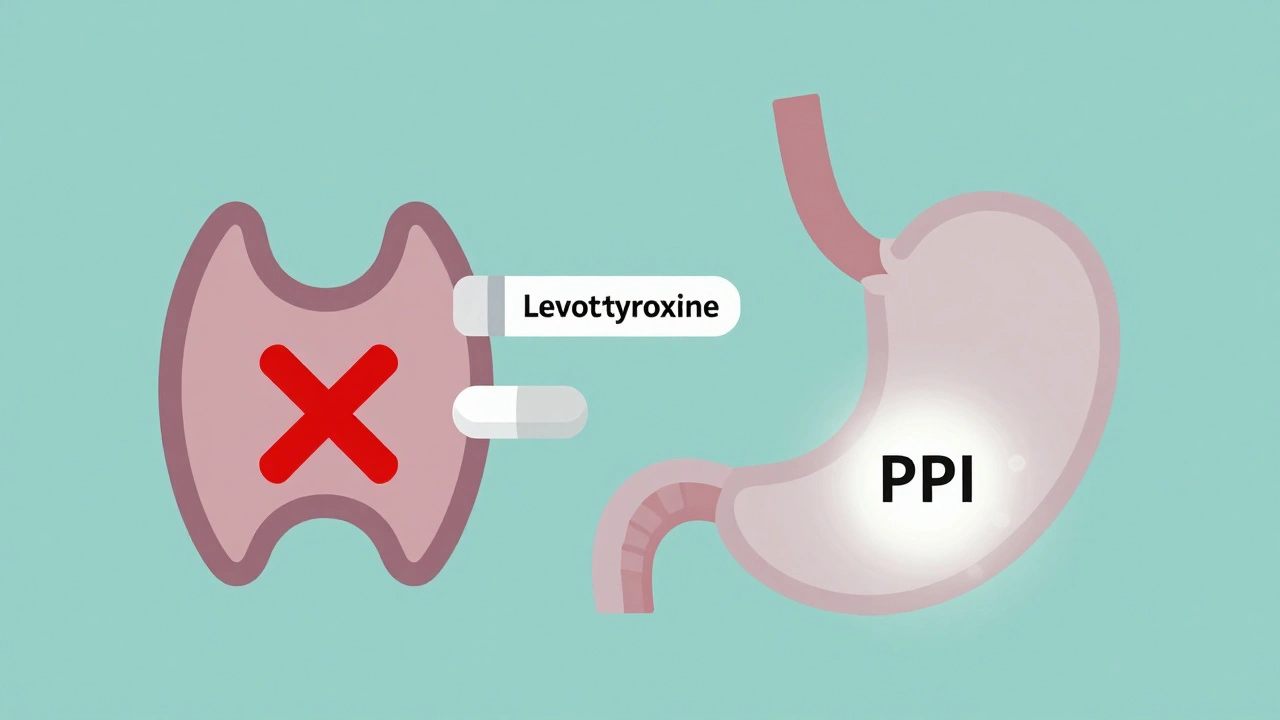
If you’re taking levothyroxine for hypothyroidism and also use a proton pump inhibitor (PPI) like omeprazole or pantoprazole for heartburn, you might be missing something critical. These two common medications don’t just coexist-they can interfere with each other in a way that leaves your thyroid levels out of balance. And most people don’t realize it until they feel worse: more tired, gaining weight, or struggling with brain fog-even though they’re taking their pills exactly as prescribed.
Why Levothyroxine Needs Acid to Work
Levothyroxine isn’t like a vitamin you can swallow with a glass of coffee. It’s a hormone replacement that needs your stomach to be acidic to dissolve and get absorbed. When your stomach pH is between 1 and 2-thanks to natural gastric acid-it breaks down the tablet properly so your body can use it. But proton pump inhibitors stop your stomach from making that acid. They shut down the acid pumps in your stomach lining, raising the pH to 4 or even 6. That’s not just a little change. It’s enough to block levothyroxine from being absorbed at all.
This isn’t theory. A 2021 systematic review in the Journal of General Internal Medicine looked at seven studies and found that people taking both drugs had consistently higher TSH levels. Higher TSH means your thyroid isn’t getting enough hormone. Your body is screaming for more levothyroxine because it’s not getting absorbed.
Which PPIs Cause the Most Trouble?
All major PPIs interfere: omeprazole (Prilosec), esomeprazole (Nexium), pantoprazole (Protonix), lansoprazole (Prevacid), and rabeprazole (AcipHex). A 2023 study published in PubMed (PMID: 37259094) tested pantoprazole at 40mg daily for six weeks in people already stable on levothyroxine. Even though they took their thyroid pill in the morning and the PPI at night, TSH still jumped. Why? Because PPIs don’t just work for a few hours. Their effect lasts up to 72 hours. So timing them apart-say, four hours-isn’t enough. The acid suppression is too long-lasting.
And you can’t assume it’s safe just because you’ve been on both for months. A 2020 analysis in Mayo Clinic Proceedings showed that 15-20% of hypothyroid patients on long-term PPIs need their levothyroxine dose increased. For some, that means going from 75 mcg to 100 mcg. For others, it’s 125 mcg. It’s not about being noncompliant-it’s about chemistry.
What Happens When Absorption Drops
When levothyroxine doesn’t get absorbed, your body doesn’t know. Your pituitary gland keeps pumping out TSH, thinking your thyroid is underactive. You start feeling the symptoms again: fatigue, cold hands, dry skin, constipation, brain fog, weight gain. Many patients on Reddit’s r/Hashimotos subreddit reported exactly this. In a 2023 analysis of 147 posts, 72% said they felt more tired after starting a PPI. 58% noticed unexplained weight gain. And 68% said they had to increase their levothyroxine dose to feel normal again.
These aren’t anecdotes. They match clinical data. The American Thyroid Association’s 2022 guidelines say this interaction is common enough that doctors should expect it. If you’re on both drugs and your TSH is rising, don’t assume you’re just getting worse. Your meds might be fighting each other.

What Can You Do?
There are four real solutions-not just "take it at a different time."
- Switch to liquid levothyroxine - Tirosint-SOL is a brand-name liquid form that doesn’t need acid to absorb. It’s made with glycerin, not fillers that require stomach acid to dissolve. A 2019 study in the Journal of Clinical Endocrinology & Metabolism confirmed it works just fine with PPIs. But it costs $350 a month, compared to $15-25 for generic tablets. Insurance doesn’t always cover it unless you’ve tried everything else.
- Switch from PPIs to H2 blockers - Famotidine (Pepcid) and nizatidine are H2 receptor antagonists. They reduce acid too, but not as strongly or as long. A 2018 study in Pharmacotherapy found no significant change in TSH when patients switched from PPIs to famotidine. They still got heartburn relief, but their thyroid levels stayed stable. The trade-off? H2 blockers don’t work as well for severe GERD. They’re better for occasional use.
- Get your TSH tested - If you’re starting a PPI, get a baseline TSH before you begin. Then test again at 6-8 weeks. Most guidelines, including those from the American Association of Clinical Endocrinologists, recommend this. If TSH is up by more than 2.5 mIU/L, increase your levothyroxine by 12.5-25 mcg. Cleveland Clinic data shows 43% of patients stabilize within 12 weeks after a dose adjustment.
- Ask if you even need the PPI - Long-term PPI use (over 3 months) is linked to bone loss, kidney issues, and nutrient deficiencies. Many people take them for years without ever reassessing. Talk to your doctor: Can you reduce the dose? Try lifestyle changes? Use it only when needed? Short-term use (under 4 weeks) rarely causes problems, according to Dr. Elizabeth Pearce, an endocrinologist at Boston Medical Center.
What Doesn’t Work
Separating doses by 4 hours? Doesn’t help. Taking levothyroxine on an empty stomach but then taking the PPI right after? Still doesn’t help. Waiting until after breakfast? No. The problem isn’t timing-it’s the lack of acid in your stomach. PPIs suppress acid production for days. Even if you take your thyroid pill at 5 a.m. and your PPI at 8 p.m., your stomach is still too neutral at 7 a.m. the next day.
Some online forums suggest taking levothyroxine with water only, avoiding coffee or calcium. That’s good advice-but it won’t fix a PPI interaction. You need to address the root cause: the acid suppression.

What’s New in 2025?
The FDA is updating its labeling rules for thyroid medications to explicitly warn about PPI interactions. That’s new. And there’s research underway. A phase 3 trial (NCT04892357) is testing enteric-coated levothyroxine tablets designed to dissolve in the small intestine instead of the stomach. If approved, these could bypass the problem entirely.
Also, Tirosint-SOL’s patent expires in 2025. That means generic versions could hit the market, possibly lowering the price from $350 to under $100. That would be a game-changer for millions.
Meanwhile, the American Thyroid Association’s 2024 guidelines are expected to push harder for alternatives to long-term PPI use in thyroid patients. The message is clear: don’t just accept rising TSH. Investigate why.
Bottom Line
If you’re on levothyroxine and take a PPI, your thyroid levels might be off-even if you feel fine. Don’t wait for symptoms to get worse. Get your TSH checked. Talk to your doctor about switching to famotidine or liquid levothyroxine. And ask if you really need the PPI at all. This isn’t a rare side effect. It’s a well-documented, common interaction affecting nearly 3 million Americans. You’re not alone. But you need to act.
Suzanne Johnston
December 4, 2025 AT 09:03So let me get this straight - we’re telling people to stop taking PPIs because of a 15-20% chance their thyroid med might not absorb? Meanwhile, those same people are at risk for Barrett’s esophagus, pneumonia, and kidney damage from long-term acid suppression. Who’s really being harmed here? The system isn’t broken - it’s just lazy. We optimize for convenience, not physiology. And now we’re punishing patients for trusting their doctors? That’s not science. That’s fear-mongering dressed up as a public service.
Graham Abbas
December 4, 2025 AT 21:50Imagine your body is a cathedral. Levothyroxine is the sacred flame that needs the right kind of incense - acid - to rise properly. PPIs? They’re the janitor who turns off the gas to the whole altar because he’s afraid of a tiny spark. And now the congregation is confused why the lights went out. We’ve turned medicine into a puzzle where the pieces don’t fit - and the patient is blamed for not solving it alone. This isn’t just pharmacology. It’s a metaphor for how we treat chronic illness: fragmented, disconnected, and deeply unfair.
Haley P Law
December 6, 2025 AT 00:17OMG I WAS THIS PERSON 😭 I took omeprazole for 3 years and thought I was just getting older… then switched to famotidine and suddenly I could THINK again?? Like my brain un-fogged?? I cried in the pharmacy. Also I started drinking apple cider vinegar in water before breakfast and now I feel like a new person. #thyroidwarrior #PPIsAreEvil
Andrea DeWinter
December 6, 2025 AT 09:17If you're on levothyroxine and a PPI check your TSH at 6 weeks after starting the PPI. If it's up more than 2.5 adjust your dose by 12.5 to 25 mcg. That's it. No drama. No panic. Just numbers. You don't need to stop the PPI unless you have other reasons. Liquid levothyroxine works but it's expensive. H2 blockers are fine for occasional use. If you're asymptomatic and your TSH is stable don't fix what ain't broke. But if you're tired and gaining weight and your TSH is climbing - yeah that's your PPI talking. Talk to your doctor. Get tested. You got this.
Steve Sullivan
December 6, 2025 AT 23:27bro i took pantoprazole for like 2 years and never knew this… my tsh went from 2.1 to 8.9 and i thought i was just depressed or something… then my endo was like ‘wait u on a ppi?’ and i was like ‘uhhh yeah’ and she was like ‘that’s your problem’ and i cried in the parking lot lmao. switched to pepcid and my energy came back in 3 weeks. also i still take my thyroid med at 5am with water and now i can eat toast at 7am without feeling like a zombie. life changing. also why does no one talk about this???
George Taylor
December 7, 2025 AT 13:55ian septian
December 8, 2025 AT 07:09Check TSH. Adjust dose if needed. Try famotidine. If it works, stick with it. If not, talk to your doctor about liquid levothyroxine. Don't panic. Don't quit your PPI cold. Just act. You got this.