Phosphate control: simple steps you can use today
High phosphate is a common problem for people with kidney disease and it affects your bones, heart, and energy. If your doctor mentioned "phosphate control," you don’t need confusion—just clear, practical steps. Here are things that actually change numbers on your lab report.
Diet: what to cut and what to keep
Start with food. Cut processed foods—those often hide phosphate additives like "phosphoric acid," "sodium phosphate," or "pyrophosphate." Think colas, canned sauces, packaged deli meats, and many ready meals. These additives raise phosphate much more than natural foods.
Limit high-phosphate whole foods in measured portions: dairy (milk, cheese), nuts, seeds, chocolate, and organ meats. You don’t have to stop these forever—small portions and spacing them through the day helps.
Choose lower-phosphate swaps: fresh fruit, many vegetables, white bread instead of wholegrain for some patients (only if your care team approves), and lean chicken or fish in moderate portions. Cooking methods like boiling can reduce mineral content slightly—useful when your phosphate is high.
Medicine and monitoring
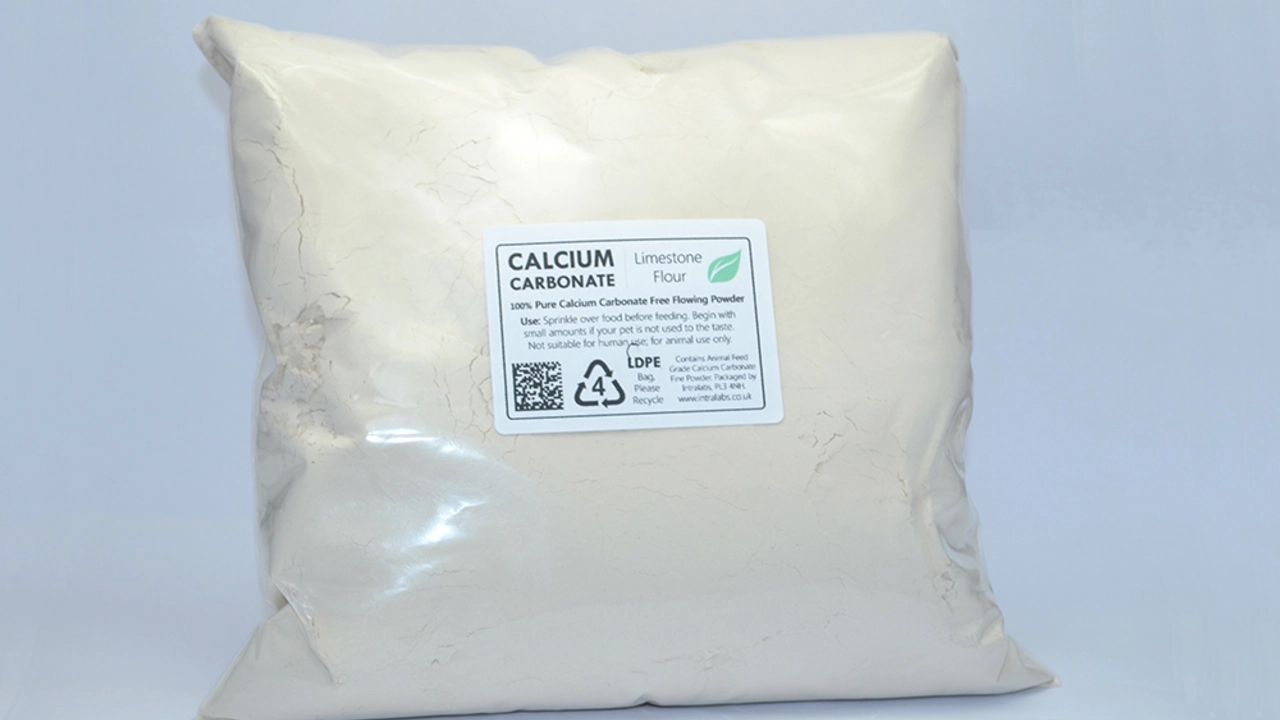
Phosphate binders are a main tool. Common options are sevelamer, calcium acetate (PhosLo), lanthanum, and newer iron-based binders. The key rule: take binders with meals. They work in your gut to stop phosphate being absorbed.
Never change binders or stop them without talking to your doctor. Your team will balance phosphate with calcium and vitamin D because these interact. Too much calcium can cause problems; too little vitamin D can make parathyroid hormone rise.
Labs matter. Target ranges differ a bit by country, but a common adult range is about 0.8–1.5 mmol/L (2.5–4.5 mg/dL). Your nephrologist will set your specific target and check phosphorus, calcium, and PTH regularly. Bring recent food lists and meds to clinic visits—small details change treatment choices.
Dialysis removes some phosphate but not enough for many people. That’s why diet and binders still matter even if you’re on dialysis. Timing dialysis sessions and binder use is part of a plan your clinic should explain.
Practical daily tips: read labels for "phosphate" terms, take binders with every meal, keep portion sizes steady, and work with a renal dietitian. Small, consistent changes beat big short-term diets.
If you experience muscle cramps, bone pain, itchiness, or fatigue, tell your doctor—these can be signs of phosphate imbalance or related issues. Your care team can adjust diet, binders, or dialysis settings to lower risk.
Want specific food swaps or a sample meal plan? Ask your clinic dietitian—personal plans beat generic lists. Tracking a few days of what you eat before a clinic visit helps them tune your plan fast.