Calcium Acetate vs. Calcium Carbonate: Which is Better for Phosphate Control?
 Jul, 12 2023
Jul, 12 2023
Understanding Calcium Acetate and Calcium Carbonate
Before we dive deep into the comparison between Calcium Acetate and Calcium Carbonate, it's important to first understand what these compounds are. Calcium Acetate, also known as Ca(C2H3O2)2, is a type of calcium salt used to control high levels of phosphate in the blood, especially for patients with kidney diseases. On the other hand, Calcium Carbonate, or CaCO3, is a common substance found in rocks and is also used to prevent high phosphate levels.
The Role of Calcium Acetate in Phosphate Control
Calcium Acetate is a potent phosphate binder, which helps to reduce phosphate levels in the body. When consumed, it reacts with the phosphate in food to form calcium phosphate, which is then excreted out of the body. This helps to maintain a balance in the phosphate levels.
This compound is particularly valuable in treating patients with chronic kidney disease (CKD) where the kidneys are unable to filter out excess phosphate. By binding the phosphate in food, Calcium Acetate prevents the phosphate from being absorbed into the blood, thus helping to control the phosphate levels.
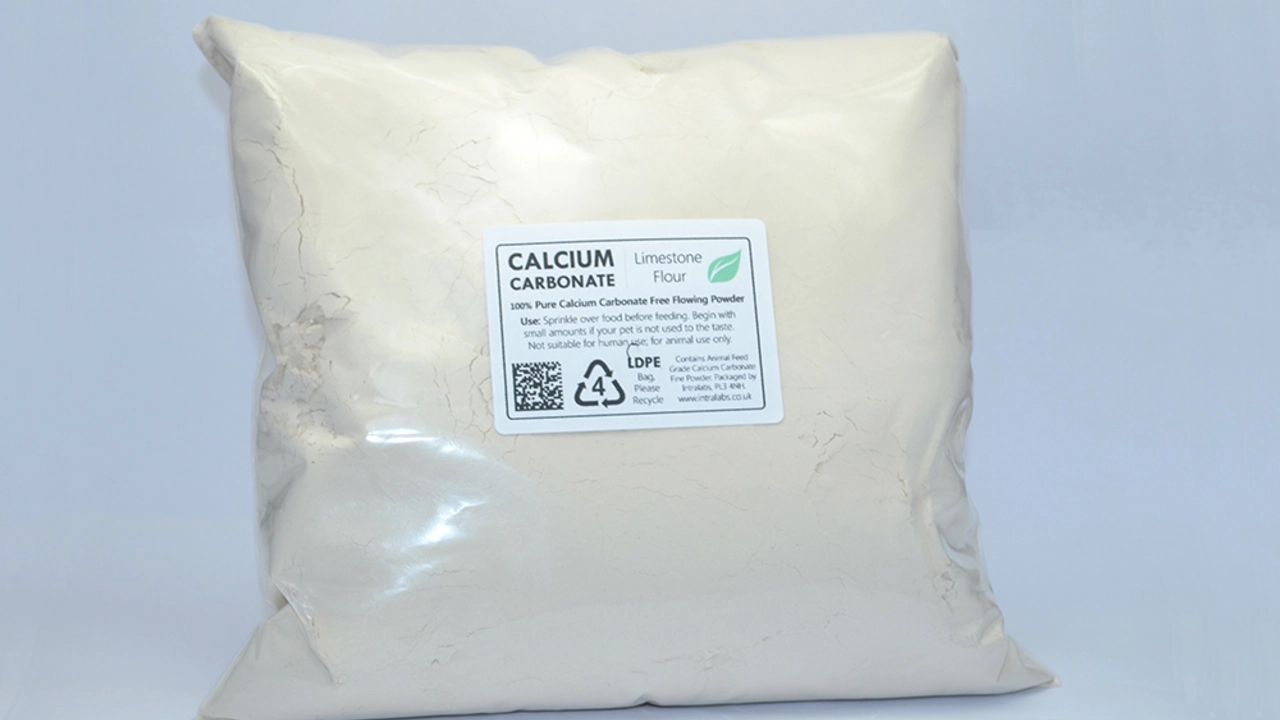
Calcium Carbonate’s Contribution to Phosphate Control
Just like Calcium Acetate, Calcium Carbonate also plays a vital role in managing phosphate levels in the body. It acts as a phosphate binder, which means it binds with dietary phosphate to form insoluble calcium phosphate, which is then eliminated from the body.
Due to its high calcium content, Calcium Carbonate not only helps to control phosphate levels but also contributes to the necessary calcium intake of the body. This is especially beneficial for patients suffering from osteoporosis or other conditions that require increased calcium intake.
Comparing the Efficacy of Calcium Acetate and Calcium Carbonate
When it comes to efficacy in phosphate control, both Calcium Acetate and Calcium Carbonate have shown significant results. However, studies have shown that Calcium Acetate may be slightly superior in terms of controlling serum phosphorus levels in patients with CKD.
Furthermore, Calcium Acetate is less likely to cause hypercalcemia, a condition characterized by excessively high levels of calcium in the blood. This makes it a safer option for long-term use, especially in patients with kidney diseases.
On the other hand, while Calcium Carbonate is also effective in phosphate control, it can potentially lead to hypercalcemia if taken in high doses or for an extended period.
Choosing the Right Compound for Phosphate Control
Choosing between Calcium Acetate and Calcium Carbonate largely depends on the individual's health condition and the doctor's recommendation. For patients with CKD, Calcium Acetate might be a better option due to its superior phosphate-binding capacity and lower risk of hypercalcemia.
However, for those who require additional calcium intake, such as osteoporosis patients, Calcium Carbonate could be more beneficial, as long as the dosage is carefully managed to avoid hypercalcemia.
It's important to remember that both compounds should be taken under medical supervision to ensure safety and efficacy.
Doreen Collins
July 12, 2023 AT 11:43Great overview! If you’re managing phosphate levels, remember to stay consistent with dosing and keep regular lab checks. Your kidneys will thank you.
Casey Morris
July 13, 2023 AT 09:56Hello there, dear reader, I must say, this article is quite enlightening; the juxtaposition of calcium acetate and calcium carbonate is, indeed, thoughtfully presented, and I applaud the clarity.
Teya Arisa
July 14, 2023 AT 08:10Thank you for this comprehensive examination. It is evident that calcium acetate offers a marginal advantage in phosphate binding, which is crucial for patients with chronic kidney disease. 😊 Please ensure to discuss dosage adjustments with your nephrologist. 👍
Kester Strahan
July 15, 2023 AT 06:23From a pharmacokinetic standpoint, calcium acetate exhibits a higher binding affinity for orthophosphate due to its acetate moiety, which facilitates ion exchange in the gastrointestinal tract. The carbonate variant, albeit cheaper, introduces additional calcium load that may predispose to hypercalcemia, especially in the context of CKD-MBD protocols. Also, the formulation differences affect pill burden – a consideration for compliance. lol, the misspelling in the article "Phospate" was kinda funny.
Jordan Levine
July 16, 2023 AT 04:36THIS IS WHY WE NEED TO STAND UP FOR OUR HEALTH! CALCIUM ACETATE IS THE TRUE HERO, NOT THAT BORING CARBONATE STUFF! 🔥💪🇺🇸
Lindy Hadebe
July 17, 2023 AT 02:50The piece glosses over the cost implications, which can be a deal‑breaker for many patients. A more balanced view would acknowledge insurance hurdles.
Ekeh Lynda
July 18, 2023 AT 01:03It is essential to recognise that the therapeutic window for calcium‑based binders is narrow and that individual patient factors dictate the optimal choice. The article correctly highlights the lower risk of hypercalcaemia with acetate yet fails to address the potential for acidosis in some scenarios. Moreover the impact on bone turnover markers is a nuanced topic that warrants further discussion. Long‑term outcomes remain incompletely defined and should be the focus of future trials. Clinicians must weigh the trade‑offs between phosphate control and calcium load judiciously. Patient education remains paramount to ensure adherence and monitor for adverse effects
Mary Mundane
July 18, 2023 AT 23:16Another bland summary with zero actionable insight.
Michelle Capes
July 19, 2023 AT 21:30Interesting points! i think its good 2 see the emphasis on monitoring labs :) but maybe add some tips for patients on diet? thx!
junior garcia
July 20, 2023 AT 19:43Wow, that was a helpful read-thanks for breaking it down so simply.
Dahmir Dennis
July 21, 2023 AT 17:56Ah, the age‑old debate of calcium acetate versus calcium carbonate-how utterly fascinating. One might think that such a topic would inspire groundbreaking research, yet we are left with the same tired conclusions. First, calcium acetate’s superior phosphate‑binding capacity is touted as a miracle, but we forget the modest increase in pill burden for patients already juggling multiple meds. Second, the alleged lower risk of hypercalcemia is presented as if it were a panacea, ignoring the fact that dietary calcium intake varies wildly among individuals. Third, the article neglects to mention the potential for metabolic acidosis, a subtle yet clinically relevant side effect of acetate salts. Fourth, the financial aspect is brushed aside, despite many insurance plans favoring the cheaper carbonate formulation. Fifth, we are reminded that patient adherence hinges on taste and tolerability-acetate can be less palatable. Sixth, the piece fails to address the nuanced role of vitamin D analogs that often accompany phosphate binders. Seventh, the interplay with other medications, such as iron supplements, is omitted, leading to incomplete guidance. Eighth, the long‑term cardiovascular outcomes remain ambiguous, a point that deserves more than a footnote. Ninth, the impact on bone mineral density is not thoroughly explored, leaving clinicians to guess. Tenth, the article’s references are outdated, relying on studies from over a decade ago. Eleventh, there is no discussion of emerging non‑calcium binders that may sidestep these issues altogether. Twelfth, the potential for patient confusion when switching between binders is ignored. Thirteenth, the role of patient education programs in mitigating risks is underplayed. Fourteenth, the ethical considerations of prescribing more expensive drugs without clear superiority are absent. Finally, one must wonder whether the author ever consulted a practicing nephrologist before penning this piece. In short, the article offers a surface‑level comparison while neglecting the depth required for informed clinical decisions.
HILDA GONZALEZ SARAVIA
July 22, 2023 AT 16:10To add some practical guidance: when selecting a binder, start by reviewing the patient’s serum calcium, phosphorus, and PTH levels. If calcium is already elevated, calcium acetate is preferred due to its lower calcium load. For patients with low dietary calcium, calcium carbonate can be beneficial, but monitor for hypercalcemia every 1–3 months. Educate patients to take the binder with meals, preferably spaced evenly throughout the day, and advise them to avoid antacids that may interfere with binding efficiency. Also, consider the pill size; some formulations are chewable, which can improve adherence. Finally, keep an eye on potential drug‑drug interactions, especially with iron supplements and certain antibiotics.
Amanda Vallery
July 23, 2023 AT 14:23Calcium acetate binds roughly 30% more phosphate per gram than calcium carbonate, which is a well‑documented fact.
Kathryn Rude
July 24, 2023 AT 12:36One could argue that the dichotomy presented here mirrors the eternal struggle between form and function, yet we forget that both compounds are merely tools wielded by the physician’s hand. The true art lies in discerning which tool aligns with the patient’s metaphysical balance, not simply the biochemical equation. :)