Opioid Constipation: What It Is, Why It Happens, and How to Handle It
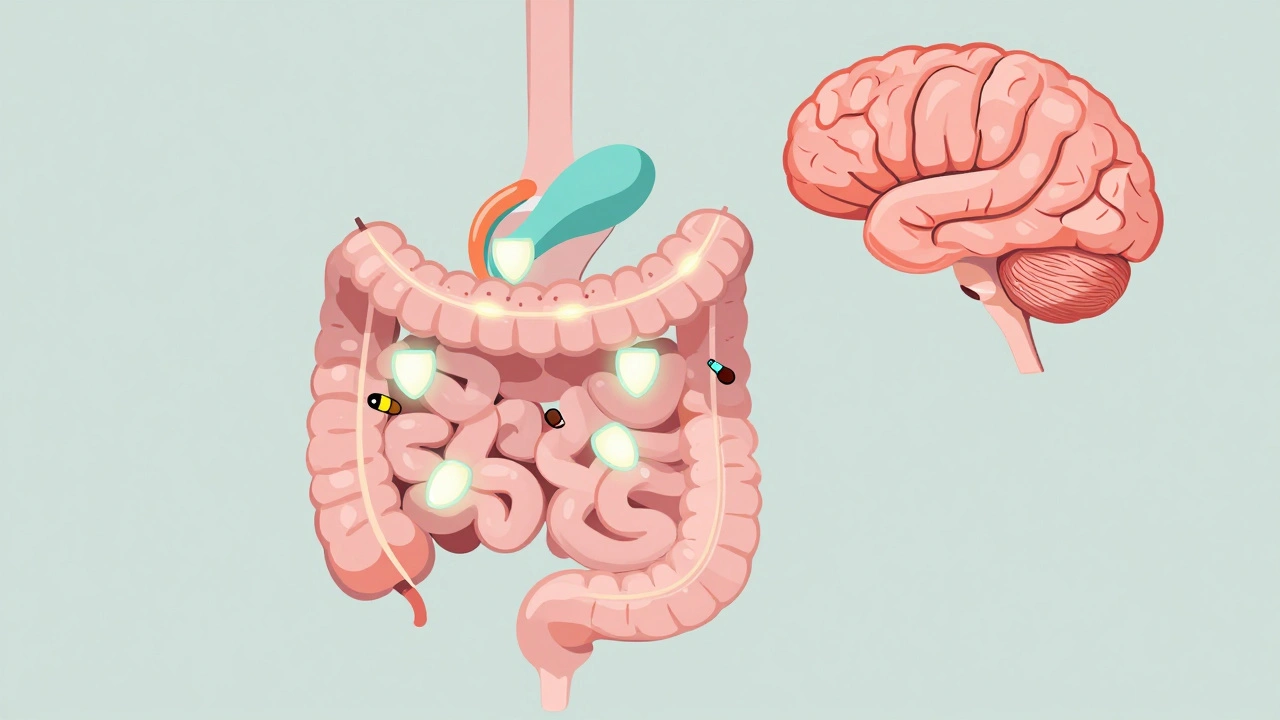
When you take opioid constipation, a side effect caused by pain medications like oxycodone, hydrocodone, or morphine that slows down the digestive tract. It's not just discomfort—it's a real medical issue that affects up to 90% of people on long-term opioid therapy. Unlike regular constipation, which might clear up with more fiber or water, opioid constipation sticks around because the drugs directly mess with the nerves in your gut. They don’t just reduce pain—they also shut down the natural contractions that move stool through your intestines. That’s why even people who eat well and drink plenty of water still struggle.
This problem doesn’t go away on its own. bowel function, the natural process of moving waste through the digestive system gets stuck in slow motion. You might feel bloated, full, or like you’re straining without results. Some people stop taking their pain meds because of this—but that’s not always safe or necessary. There are better ways. laxatives for opioid use, specific types of stool softeners and stimulants designed to work even when opioids are suppressing gut movement exist for this exact reason. Not all laxatives work the same. Over-the-counter options like MiraLAX or docusate can help, but sometimes you need prescription meds like naloxegol or methylnaltrexone that target the gut without reducing pain relief.
What makes opioid constipation tricky is that doctors often don’t talk about it until you bring it up. Many patients think it’s just something they have to live with. But it doesn’t have to be. Managing it well means understanding how opioids affect your body, knowing which treatments actually work, and avoiding the ones that don’t. For example, fiber supplements alone won’t cut it—without enough fluid, they can make things worse. And stimulant laxatives like Dulcolax? They help short-term but aren’t meant for daily, long-term use. The goal isn’t just to have a bowel movement—it’s to restore normal function without risking dependence or damage.
You’ll find real-world advice in the posts below—from how to spot early signs of trouble, to what medications actually help, to what to avoid when you’re already on opioids. Some posts cover how these side effects compare to other drug interactions, like those with PPIs or calcium-fortified juices. Others show you how to monitor your body after switching meds or managing multiple drugs at once. This isn’t theoretical. These are experiences and solutions from people who’ve been there—and from clinicians who’ve seen the damage of ignoring it.