Managing Opioid Constipation: How Peripherally Acting Mu Antagonists Work and Who Benefits
 Dec, 6 2025
Dec, 6 2025
PAMORA Selection Tool
Select your key characteristics to determine which PAMORA may be most appropriate for managing opioid-induced constipation (OIC) without affecting pain relief.
When you’re on opioids for chronic pain or cancer-related discomfort, constipation isn’t just an inconvenience-it’s a dealbreaker. Up to 80% of people taking opioids regularly develop severe constipation, and many stop their pain medication because of it. Traditional laxatives? They often fail. That’s where peripherally acting mu-opioid receptor antagonists (PAMORAs) come in. These aren’t just stronger laxatives. They’re targeted drugs designed to undo the gut-slowing effects of opioids without touching your pain relief.
Why Opioids Cause Constipation
Opioids bind to mu receptors all over the body, including in your intestines. These receptors control how fast food moves through your digestive tract. When opioids lock onto them, your gut slows down. Fluids get absorbed, stools harden, and bowel movements become rare-or impossible. This isn’t normal constipation. It’s opioid-induced constipation (OIC), and it doesn’t respond well to fiber, water, or over-the-counter stool softeners. Studies show less than 30% of chronic opioid users get regular relief from standard laxatives.What Are PAMORAs?
PAMORAs are a special class of drugs built to block opioid effects only in the gut. They don’t cross the blood-brain barrier in meaningful amounts, so they leave your pain control untouched. Think of them as precision tools: they target the problem without messing up what’s working. There are three FDA-approved PAMORAs on the market: methylnaltrexone (RELISTOR), naloxegol (MOVANTIK), and naldemedine (SYMPROIC). Each works differently, has different dosing, and fits different patient needs.Methylnaltrexone: The Fast-Acting Option
Methylnaltrexone is the oldest PAMORA, approved in 2008. It’s a quaternary amine-meaning it’s charged and can’t easily enter the brain. That’s why it works only in the gut. It’s available as a subcutaneous injection and as an oral tablet. In clinical trials, 52% of patients had a bowel movement within 4 hours after a single injection, compared to just 30% on placebo. That speed makes it ideal for cancer patients in palliative care who need quick relief. Many patients on Reddit’s r/palliativecare say it’s the only thing that restored their dignity and quality of life without affecting pain control. The oral form (450 mg) is used for chronic noncancer pain. It takes about 30 minutes to start working, and most people see results within 1-2 hours. It doesn’t interact with other drugs because it’s not processed by the liver’s CYP450 system. That’s a big plus if you’re on multiple medications.Naloxegol: The Daily Oral Choice
Naloxegol is a modified version of naloxone, tweaked with a polyethylene glycol chain so it stays out of the brain. It’s taken as a 25 mg tablet once a day, on an empty stomach. In the COMPOSE trials involving over 1,300 people, 44% of those on naloxegol had a spontaneous bowel movement each week, compared to 30% on placebo. That’s solid-but not magic. Some patients report it works well at first, then loses effectiveness after a few weeks. One 67-year-old with osteoarthritis on Healthgrades said, “It worked for two weeks, then stopped. I paid $450 a month for nothing.” It’s not for everyone. If you have moderate liver problems, your dose needs to be lowered. If you have severe kidney issues, you can’t take it at all. And because it’s absorbed through the gut, eating a big meal before taking it can cut its effectiveness.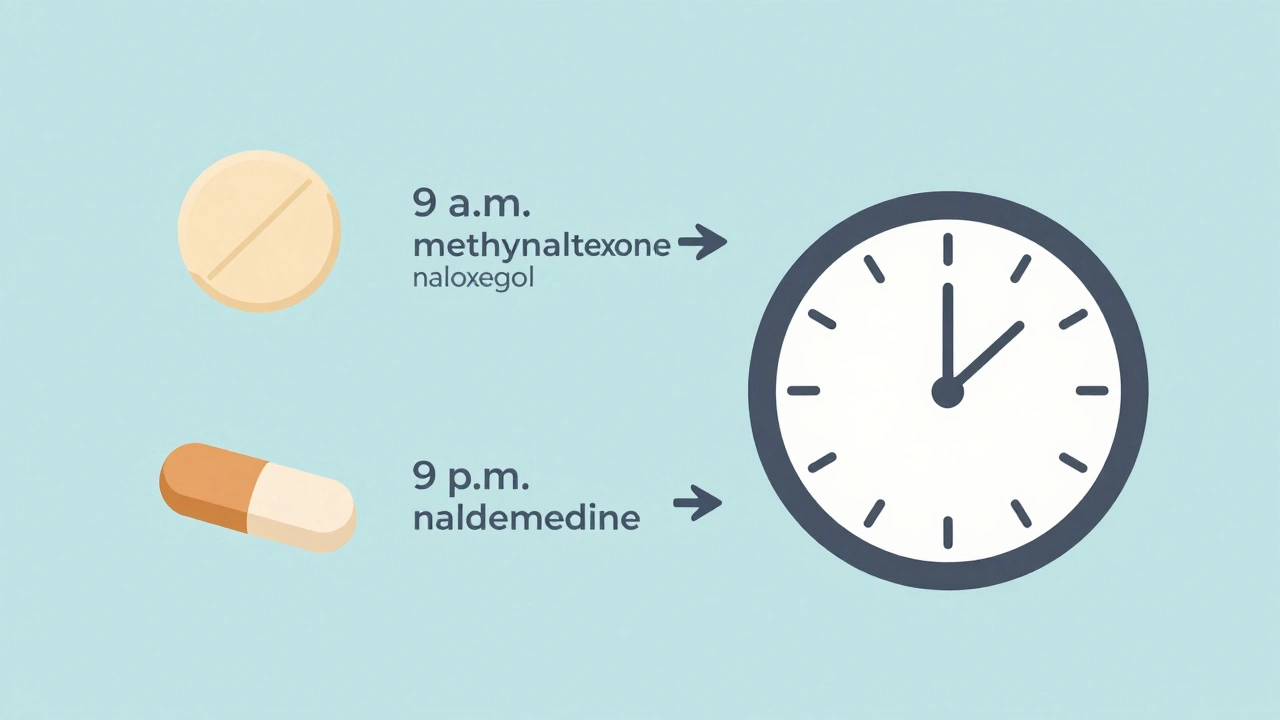
Naldemedine: The Balanced Approach
Approved in 2017, naldemedine also has a polyethylene glycol chain to keep it peripheral. It’s taken as a 0.2 mg tablet once daily, with or without food. In the COMPOSE-3 trial, 48% of patients on naldemedine had a weekly spontaneous bowel movement, compared to 35% on placebo. That’s slightly better than naloxegol. It’s also less likely to cause cramping than the others, which is why some prescribers prefer it for long-term use. It’s metabolized by the liver, so people with severe liver disease should avoid it. But unlike naloxegol, it’s safe in mild-to-moderate kidney problems. That makes it a go-to for older adults with multiple health issues.What They All Have in Common
All three PAMORAs are off-limits if you have a blocked intestine. That’s a hard rule. They can cause dangerous pressure buildup if there’s a mechanical obstruction. They’re also expensive. Without insurance, annual costs range from $5,000 to $6,000. Many patients rely on manufacturer coupons or patient assistance programs just to afford them. That’s a major barrier-especially for those on fixed incomes or without good drug coverage. Side effects are mostly mild: abdominal pain, diarrhea, nausea. But about 1 in 3 people report cramping, especially early on. That’s why doctors often start low and go slow. Some patients need to wait a few days before the cramping eases.Who Gets the Most Benefit?
Not everyone with opioid constipation needs a PAMORA. If you’re on short-term opioids after surgery, lifestyle changes and laxatives might be enough. But for people on daily opioids for months or years-especially those with cancer, chronic back pain, or neuropathic pain-PAMORAs change everything. Cancer patients on palliative care respond best to methylnaltrexone. The injection gives fast, reliable relief. For noncancer patients, oral options like naloxegol or naldemedine are more practical. Naldemedine tends to have fewer GI side effects, while naloxegol has a longer track record.
How to Use Them Right
Timing matters. PAMORAs work best when taken about an hour before your opioid dose hits its peak. For example, if you take oxycodone at 8 a.m. and 8 p.m., and it peaks around 10 a.m. and 10 p.m., take your PAMORA at 9 a.m. and 9 p.m. Start with the lowest dose. Many prescribers initially underdose because they’re afraid of side effects. But studies show that 78% of pain specialists had to increase the dose after a few weeks to get results. Monitor for diarrhea. If you’re having more than 3 loose stools a day, hold the dose and talk to your doctor. It’s rare, but it can happen.What’s Coming Next?
The market is evolving. In early 2023, a new 300 mg tablet of methylnaltrexone was approved for patients who don’t respond to the standard dose. Researchers are testing a combo drug that combines a PAMORA with a 5-HT4 agonist-a gut stimulant-to boost effectiveness even more. Early results show a 68% response rate. Biosimilars are on the horizon. The first methylnaltrexone biosimilar is in phase 3 trials in China. That could bring down costs significantly in the next few years. But here’s the catch: even with all the science behind them, PAMORAs still only reach about 35-40% of eligible patients because of cost. The American Gastroenterological Association warns that without price reductions, many will keep suffering-and quitting opioids out of frustration.Bottom Line
Opioid constipation isn’t something you just have to live with. PAMORAs offer real, targeted relief without sacrificing pain control. Methylnaltrexone works fast and is ideal for cancer care. Naloxegol and naldemedine offer daily convenience for chronic pain. None are perfect. All are costly. But for the right person, they’re life-changing.If you’ve tried laxatives, fiber, and fluids and still can’t have regular bowel movements while on opioids, talk to your doctor about PAMORAs. Don’t accept constipation as a side effect you must endure. There’s a better way.
Olivia Hand
December 7, 2025 AT 01:42I’ve been on oxycodone for 7 years after a spinal fusion. Laxatives? Useless. I tried everything-psyllium, magnesium, even enemas. Then my GI doc slipped me a sample of naldemedine. First week, I had a BM every other day. Not perfect, but I could leave the house without panic. The cramps? Yeah, they hit hard day one. But by day four, it was like my gut remembered how to work. Worth every penny if you’re stuck in this hell.
Sangram Lavte
December 7, 2025 AT 23:04In India, these drugs are nearly impossible to get. Even if you can find them, the cost is like buying a used scooter. My uncle is on morphine for bone cancer. He uses coconut oil, warm water enemas, and a daily massage with mustard oil. It’s not science, but it keeps him going. Maybe we need low-cost alternatives, not just fancy pills.
Stacy here
December 9, 2025 AT 01:35Let’s be real-Big Pharma didn’t invent PAMORAs to help you. They invented them because people were quitting opioids and losing their prescriptions. Suddenly, constipation became a ‘medical condition’ worth $6,000 a year. The real scandal? They knew this would happen since the 90s. They just didn’t care until the lawsuits started rolling in. Now they’re selling hope at the price of a Tesla. And don’t get me started on those ‘patient assistance programs’-they require 17 forms, a notarized letter from your priest, and a blood sample.
Meanwhile, your doctor gets a free trip to Vegas from the rep who handed them the sample pack. Wake up. This isn’t medicine. It’s a revenue stream disguised as relief.
Kyle Flores
December 10, 2025 AT 19:36My mom was on methylnaltrexone injections for her stage 4 lung cancer. She hated needles but said the relief was worth it. One night, she texted me: ‘I peed and pooped in the same hour. I haven’t felt human in months.’ That’s the real win. No one talks about how dignity matters more than pain control sometimes. These drugs don’t just move bowels-they move people back into life. If you’re on opioids long-term and your gut’s turned to concrete, don’t wait. Ask for PAMORAs. Even if it’s scary, even if it’s expensive-your body deserves better.
Louis Llaine
December 12, 2025 AT 13:19So we spent billions developing a drug that just unblocks your colon so you can stop feeling like a sack of bricks. And we call it ‘innovation.’ Cool. Next up: a pill that makes your socks stop stink.
Jane Quitain
December 12, 2025 AT 15:10OMG I JUST GOT MY FIRST BM IN 5 DAYS AFTER TRYING NALDEXEDINE!! I’M CRYING RN!! THIS IS A MIRACLE!! THANK YOU SCIENCE!! 🙏💖
Ernie Blevins
December 13, 2025 AT 13:31These drugs are just fancy laxatives with a marketing budget. You still get diarrhea, cramps, and you’re still constipated if you miss a dose. The real fix? Stop taking opioids. But no, let’s keep pumping people full of painkillers and then sell them $5K/month to undo the damage. Classic.
Nancy Carlsen
December 13, 2025 AT 17:55Just wanted to say-this post saved my life. I thought I had to live with this. I cried reading about naldemedine because it sounded too good to be true. I asked my doctor last week. She prescribed it. Two days later, I had my first normal BM in over a year. I’m not just relieved-I’m free. To anyone reading this: don’t suffer in silence. You deserve to poop without pain. 💕🫶