NSAIDs and Blood Thinners: Risks, Interactions, and What You Need to Know
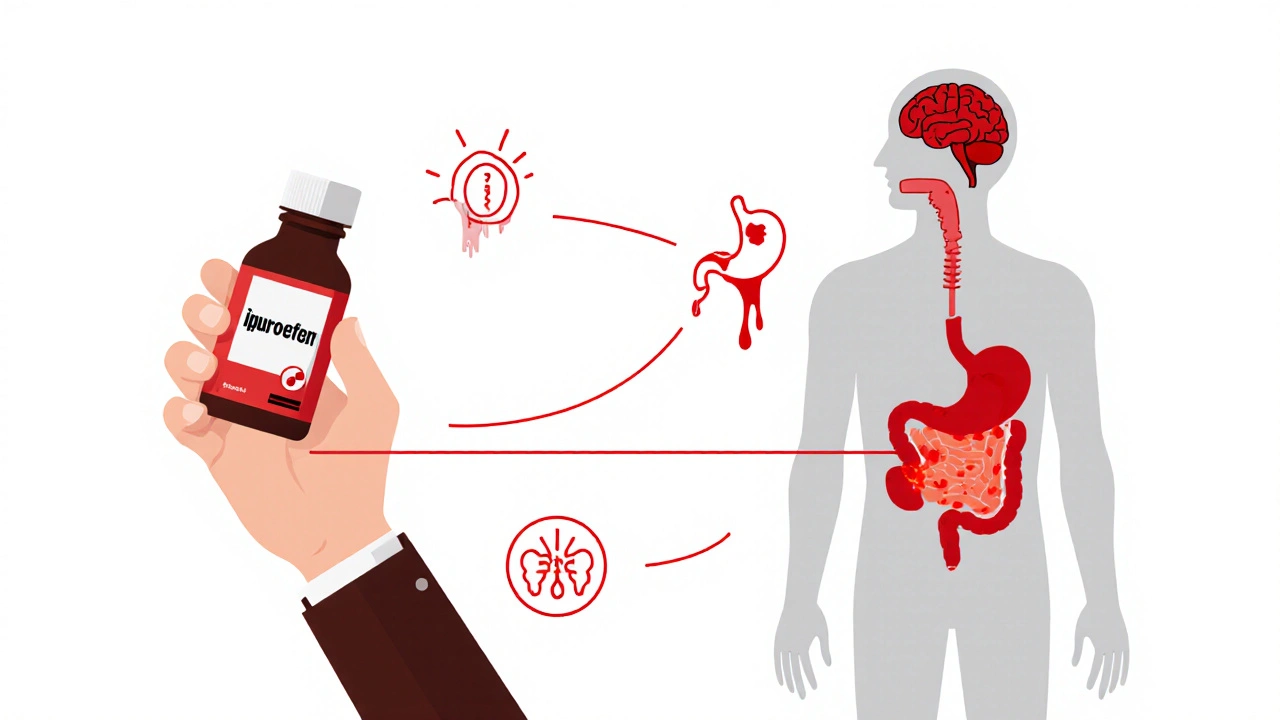
When you take NSAIDs, nonsteroidal anti-inflammatory drugs like ibuprofen or naproxen used for pain and swelling. Also known as anti-inflammatory meds, they help with everyday aches but can quietly increase your risk of serious bleeding if you’re also on blood thinners, medications like warfarin, apixaban, or rivaroxaban that prevent clots.
Here’s the problem: NSAIDs mess with your stomach lining and platelets—the tiny cells that help blood clot. Blood thinners do the same thing, just in different ways. When you stack them, your body’s natural clotting system gets overwhelmed. Studies show people on both types of drugs have up to three times the risk of internal bleeding compared to those on blood thinners alone. It’s not rare. It’s not theoretical. It happens in kitchens, pharmacies, and ERs every day. And it’s often missed because the symptoms—dizziness, dark stools, unexplained bruising—get blamed on aging, stress, or even the flu.
Not all NSAIDs are equal. Ibuprofen is riskier than naproxen when paired with warfarin. Aspirin? It’s technically an NSAID too, and it’s even more dangerous because it permanently disables platelets. Even a single daily low-dose aspirin for heart protection can turn a routine painkiller into a silent threat. And it’s not just prescription blood thinners. Some herbal supplements like garlic, ginkgo, or fish oil act like thinners too. If you’re taking any of these, your doctor needs to know—even if you think it’s "just a supplement."
Who’s Most at Risk?
Older adults. People with ulcers or kidney issues. Those on multiple meds for high blood pressure, diabetes, or heart disease. If you’re over 65 and popping ibuprofen for arthritis while on Xarelto for atrial fibrillation, you’re in the danger zone. But it’s not just seniors. Younger people on blood thinners after a clot or surgery are just as vulnerable. And many don’t realize their OTC pain reliever is part of the problem.
There’s a simple fix: talk to your doctor before taking anything for pain, fever, or inflammation. Acetaminophen (Tylenol) is usually the safer choice—it doesn’t affect clotting. But even that has limits if you have liver problems. Don’t swap one drug for another without checking. And if you’ve been taking NSAIDs for years without issues, don’t assume you’re safe. Risk builds over time.
What you’ll find in the posts below are real stories, clinical data, and clear steps to avoid the most common mistakes. From how garlic supplements quietly boost bleeding risk to why calcium-fortified juice can interfere with your meds, these aren’t theory pages. They’re practical guides written for people who take meds every day and want to stay out of the hospital. No jargon. No scare tactics. Just what you need to know to keep yourself safe.