NSAIDs and Blood Thinners: What You Need to Know About the Dangerous Risk
 Nov, 28 2025
Nov, 28 2025
Blood Thinner & Pain Medication Safety Checker
This tool helps you check if a pain medication is safe to take with your blood thinner. Based on current medical research, most NSAIDs (like ibuprofen) are dangerous when combined with blood thinners.
Select your blood thinner and pain medication to see if they're safe together.
If you're taking a blood thinner like warfarin, apixaban, or rivaroxaban, and you reach for ibuprofen or naproxen to ease a headache, sore knee, or back pain, you're putting yourself at serious risk. This isn't a rare edge case-it's a common, dangerous mix that sends tens of thousands to the emergency room every year. The problem isn't just that both drugs thin your blood. It's that they do it in different, overlapping ways, and together, they can turn a minor injury into a life-threatening bleed.
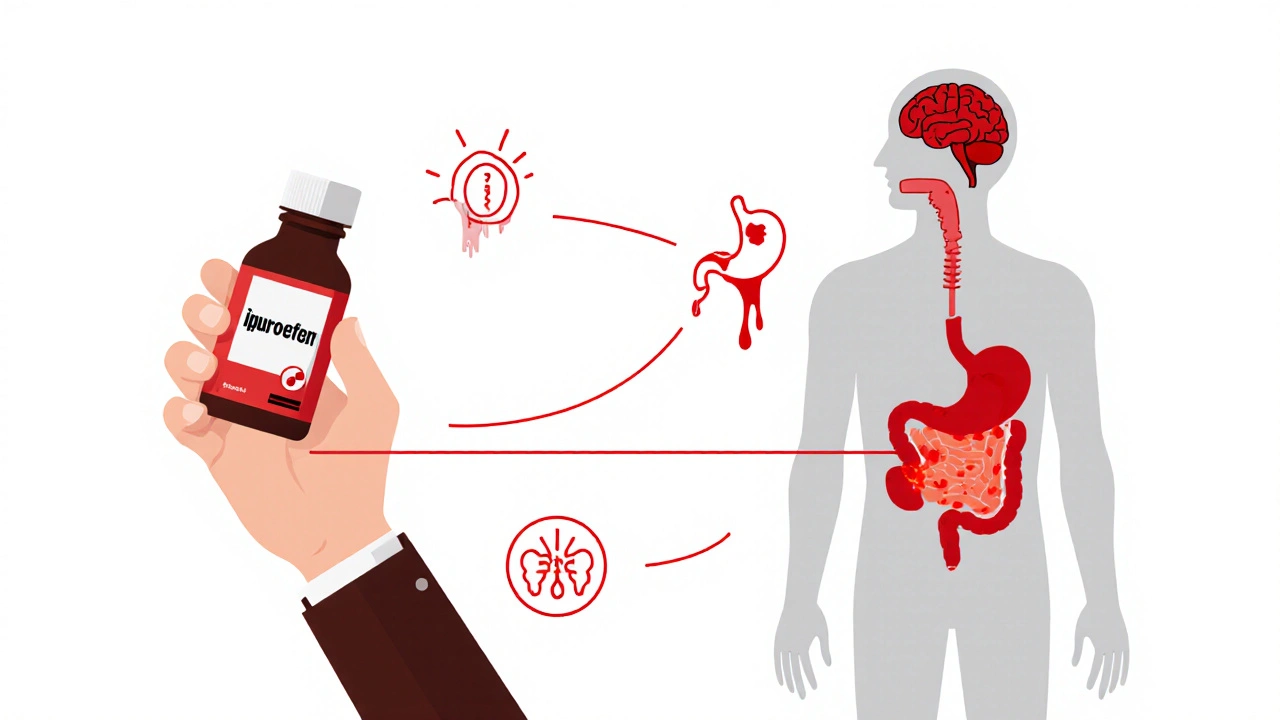
Why NSAIDs and Blood Thinners Don't Mix
NSAIDs-like ibuprofen, naproxen, diclofenac, and even aspirin-work by blocking enzymes called COX-1 and COX-2. These enzymes help your blood platelets stick together to form clots when you get cut. By slowing that down, NSAIDs reduce pain and swelling, but they also make it harder for your body to stop bleeding. Meanwhile, blood thinners like warfarin or the newer DOACs (direct oral anticoagulants) work on different parts of the clotting system, preventing dangerous clots from forming in your veins or heart. When you combine them, your body loses two layers of natural protection. The result? Your blood just doesn't clot the way it should.It's not just a theory. A 2024 study from Denmark tracked over 100,000 people on blood thinners and found that those who took NSAIDs had more than double the risk of serious bleeding. The numbers are specific: diclofenac raised the risk 3.3 times, naproxen 4.1 times, and even common ibuprofen pushed it up nearly 80%. These aren't small increases-they're dramatic.
Where the Bleeding Happens
The danger isn't random. Bleeding from this combo shows up in predictable, dangerous places:- Gastrointestinal tract: Stomach and intestinal bleeding is the most common. NSAIDs damage the protective lining of your stomach, and blood thinners prevent the clotting that would normally seal those small ulcers. This leads to black, tarry stools, vomiting blood, or sudden dizziness from internal blood loss.
- Brain: Intracranial hemorrhage risk jumps over threefold. A fall, even a minor one, can turn into a stroke or brain bleed.
- Urinary tract: Blood in urine isn't always infection-it can be from internal bleeding caused by the drug combo.
- Under the skin: Unexplained bruising, especially large, painful patches, is a red flag.
One patient in Melbourne, 72, was on apixaban for atrial fibrillation. He took ibuprofen for his arthritis, thinking it was harmless. After a minor stumble, he ended up in the ER with a massive stomach bleed. His hemoglobin dropped from 13 to 7 in under 48 hours. He needed two blood transfusions. He didn’t know the risk-his doctor never warned him.
Not All Blood Thinners Are the Same
The risk isn't equal across all anticoagulants. Warfarin, the older drug, has the highest bleeding risk when mixed with NSAIDs-up to 3.8 times higher. That's because NSAIDs interfere with how warfarin is processed in the liver, making its effects stronger and harder to predict. Newer drugs like apixaban and rivaroxaban are more consistent, but they're still dangerous when combined with NSAIDs. Studies show even these “safer” blood thinners double the risk of bleeding when taken with NSAIDs.And here's something most people don’t realize: the risk doesn't disappear just because you're on a DOAC. A 2022 study in the Journal of the American Heart Association showed that patients on rivaroxaban who took NSAIDs had a 2.1 times higher chance of bleeding compared to those who didn't. That's not a small number-it's a major red flag.
What About Celecoxib? Is It Safer?
Celecoxib (Celebrex) is a COX-2 selective NSAID, marketed as being gentler on the stomach. It does reduce the risk of gastrointestinal bleeding compared to naproxen or diclofenac-but it's still not safe. Studies show it still increases bleeding risk by 40% when taken with blood thinners. It doesn’t fix the platelet problem. So while it might be a slightly better choice than ibuprofen, it’s still not a safe one.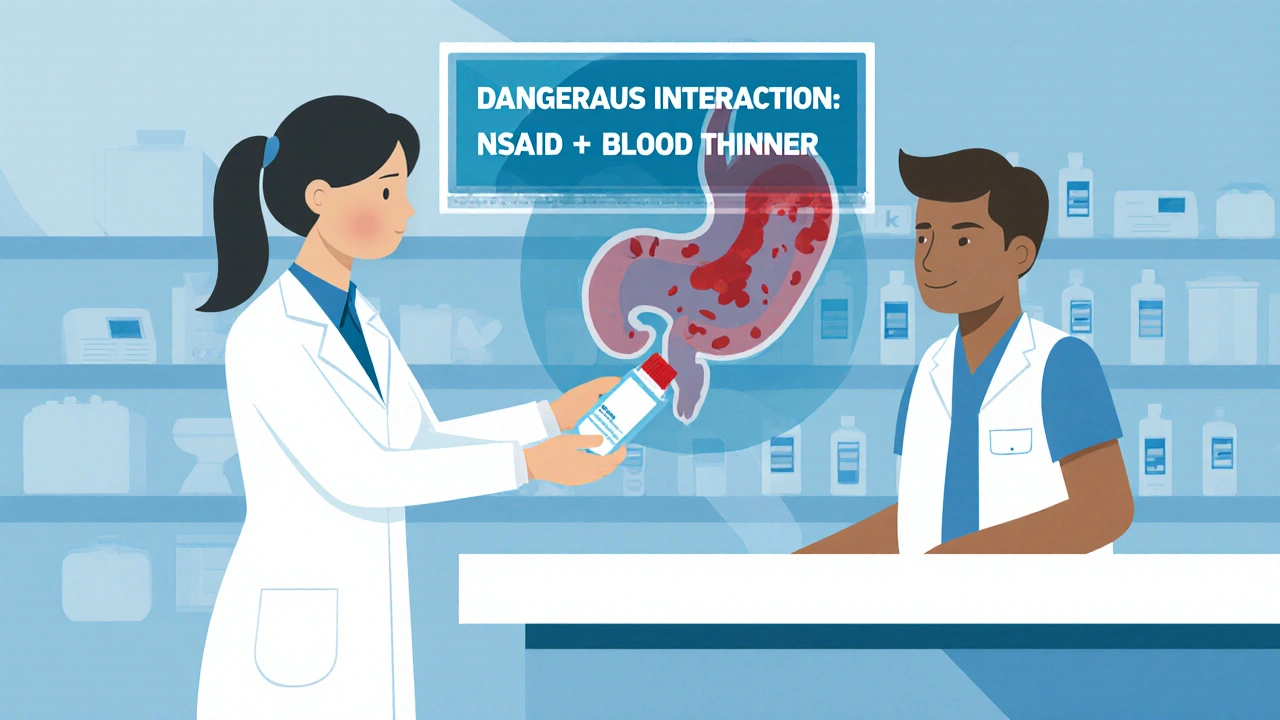
The Only Safe Pain Reliever: Acetaminophen
There is one painkiller you can usually take safely with blood thinners: acetaminophen (Tylenol). Unlike NSAIDs, it doesn’t affect platelets or the stomach lining. Multiple studies confirm it doesn’t raise bleeding risk when used at standard doses-up to 4,000 mg per day.But it's not perfect. High doses can damage your liver, especially if you drink alcohol, have fatty liver disease, or take other medications that stress the liver. If you're on long-term pain relief, talk to your doctor about your liver health before using acetaminophen daily.
And don't assume all cold and flu meds are safe. Many contain hidden NSAIDs-like ibuprofen or naproxen-in combination products. Always check the label. A common “sinus and pain” tablet might have 200 mg of ibuprofen in it. You might think you're just taking a cold remedy, but you're adding a dangerous drug to your blood thinner.
What If You Really Need an NSAID?
Sometimes, pain is so bad that avoiding NSAIDs feels impossible-especially for arthritis patients. The American Heart Association says if you absolutely must use one, keep it short and low. Use the smallest effective dose for the shortest time possible-no more than 3 days. Ibuprofen at 200-400 mg once or twice a day is the least risky option.And if you're on warfarin, your INR (a blood test that measures clotting time) will likely go up when you take NSAIDs. Your doctor may need to check it weekly during this time. If you're on a DOAC, no blood test is needed-but that doesn't mean you're safe. The risk is still there.
Many doctors now prescribe a proton pump inhibitor (PPI) like pantoprazole (80 mg daily) along with NSAIDs to protect the stomach. But this isn't a magic shield. It helps with ulcers, but it doesn't stop bleeding from platelet issues. It's a band-aid, not a fix.
What Patients Are Really Doing
Online forums like Reddit’s r/Anticoagulants show how widespread this problem is. In a 2024 survey of over 1,400 users, 62% admitted to using NSAIDs with their blood thinners. Almost 4 in 10 had bleeding symptoms-nosebleeds, bruising, or stomach bleeding. Many said they didn’t know it was dangerous. Others said the pain was worse than the risk.One patient wrote: “I took ibuprofen for my knee before my dentist appointment. They had to pack gauze in my mouth for hours. I didn’t know why. Now I do.”
Another: “My doctor never mentioned it. My pharmacist didn’t say anything. I just thought it was normal.”
This isn't just about ignorance-it's about systemic failure. Only 38% of U.S. hospitals have electronic systems that block doctors from prescribing NSAIDs to patients on blood thinners. In Australia, the system is better, but not perfect. Many patients get NSAIDs from pharmacies without a prescription, and no one checks their medication list.

What to Do Instead
You don’t have to suffer. There are alternatives:- Acetaminophen for mild to moderate pain.
- Physical therapy for joint pain-studies show 68% of patients manage pain well after 4 weeks of targeted exercises.
- Topical NSAIDs like diclofenac gel. These are absorbed through the skin and have much less effect on the bloodstream. They’re safer, though still not risk-free.
- Heat, ice, compression for arthritis or muscle pain.
- Acupuncture or massage for chronic pain relief.
One 68-year-old woman in Sydney stopped all NSAIDs after a stomach bleed. She started daily walking, used heat packs for her hips, and took acetaminophen as needed. Within a month, her pain dropped from 8/10 to 3/10. She didn’t need a single NSAID.
The Bigger Picture
This isn't just a personal health issue-it's a public health crisis. In the U.S. alone, NSAID and blood thinner interactions cause 87,000 ER visits and 24,000 hospitalizations every year. The cost? Over $1.2 billion. And it's preventable.Health systems are starting to respond. The FDA now requires warning labels on all OTC NSAID packages. The European Medicines Agency mandates digital guides. Some hospitals use AI tools that flag dangerous combinations before prescriptions are filled. But until every pharmacist checks your meds, every doctor asks about over-the-counter drugs, and every patient knows the risk, this will keep happening.
The message is clear: if you're on a blood thinner, avoid NSAIDs. Not sometimes. Not if you’re careful. Avoid them. Use acetaminophen. Talk to your doctor about other pain options. Your life depends on it.
What to Ask Your Doctor
- Is my current pain medication safe with my blood thinner?
- Should I stop taking any over-the-counter pills I’m using for pain or inflammation?
- Can we check my INR if I’ve taken an NSAID recently?
- What non-drug options do you recommend for my type of pain?
- Do I need a stomach protector if I must take an NSAID?
Can I take ibuprofen with warfarin?
No. Taking ibuprofen with warfarin significantly increases your risk of serious bleeding, especially in the stomach and brain. Warfarin’s effects become stronger and harder to control when combined with NSAIDs like ibuprofen. Even small doses can cause dangerous spikes in INR. Use acetaminophen instead, or talk to your doctor about other pain management options.
Is Tylenol safe with blood thinners?
Yes, acetaminophen (Tylenol) is generally safe to use with all types of blood thinners, including warfarin, apixaban, rivaroxaban, and dabigatran. It doesn’t affect platelets or the clotting system. However, don’t exceed 4,000 mg per day, and avoid it if you have liver disease or drink alcohol regularly.
What if I accidentally took ibuprofen with my blood thinner?
If you took a single dose of ibuprofen or another NSAID, monitor yourself closely for signs of bleeding: unusual bruising, nosebleeds, dark or tarry stools, vomiting blood, severe headaches, or dizziness. If you’re on warfarin, contact your doctor-they may want to check your INR. If you experience any bleeding symptoms, go to the ER immediately. Don’t wait.
Can I take aspirin with a blood thinner?
No. Aspirin is an NSAID and affects platelet function just like ibuprofen or naproxen. Even low-dose aspirin for heart protection increases bleeding risk when combined with anticoagulants. If you're on a blood thinner and need heart protection, your doctor will choose the right medication-don’t add aspirin without their approval.
Do topical NSAIDs like Voltaren gel pose the same risk?
Topical NSAIDs like diclofenac gel are much safer than oral versions because very little enters your bloodstream. They’re often recommended for localized joint pain in patients on blood thinners. But they’re not completely risk-free-long-term use on large areas or broken skin can still lead to systemic absorption. Use only as directed and avoid combining with oral NSAIDs.
Why don’t pharmacists always warn me about this?
Many pharmacies do check for interactions, but not all systems are connected. If you buy NSAIDs over the counter without a prescription, the pharmacy may not know you’re on a blood thinner unless you tell them. Always disclose all medications-prescription, OTC, and supplements-when picking up any new drug. Don’t assume they’ll catch it.
Next Steps
- Review your medicine cabinet. Look for any NSAIDs-ibuprofen, naproxen, diclofenac, aspirin-even in cold or flu products.
- Make a list of everything you take daily, including supplements and OTC pills.
- Schedule a medication review with your doctor or pharmacist. Bring your list.
- Ask: “Is there a safer way to manage my pain without increasing my bleeding risk?”
- If you’ve had unexplained bruising, nosebleeds, or dark stools, get checked immediately.
This isn’t about fear-it’s about awareness. You’re not alone. Thousands of people face this exact dilemma. But with the right information and support, you can manage your pain without risking your life.
Justina Maynard
November 30, 2025 AT 02:16My grandma took ibuprofen for years with warfarin and never had an issue-until she didn’t. One Tuesday morning, she passed out in the kitchen with a hemorrhage in her stomach. Turned out the pharmacy didn’t flag it because she bought it online. Now she’s on acetaminophen and walks every day. I wish someone had told us sooner.
Don’t wait for a crisis to learn this. Talk to your pharmacist. Bring your pill bottles. Write it down. This isn’t fearmongering-it’s survival.
And yes, I know ‘everyone does it.’ But ‘everyone’ is dead wrong.
Stop normalizing this.
Evelyn Salazar Garcia
December 1, 2025 AT 03:40USA healthcare is a scam. Doctors don’t care. Pharmacies don’t care. You’re on your own.
Clay Johnson
December 1, 2025 AT 10:43The real tragedy isn't the NSAID-blood thinner interaction-it's the assumption that pharmaceutical safety is a priority rather than an afterthought.
We treat medicine like a menu. Pick your poison. Add extra risk. No one asks why the system lets this happen.
It’s not ignorance. It’s design.
Jermaine Jordan
December 1, 2025 AT 20:31This is not just medical advice-it’s a lifeline. Every single person reading this has someone in their life on a blood thinner. A parent. A sibling. A friend. Don’t let them die because you didn’t speak up.
Share this. Print it. Tape it to the fridge. Send it to your doctor. Demand better.
Your courage could save a life. Today. Not tomorrow. Today.
Chetan Chauhan
December 3, 2025 AT 12:39Wait so acetaminophen is safe? But i heard it causes liver damage? So now we’re just swapping one death for another? This is why i dont trust doctors. Everything is a tradeoff. Nothing is clean. Just let me take my ibuprofen and live my life.
Phil Thornton
December 3, 2025 AT 15:48I took naproxen for my back and didn’t tell my doctor. Got a nosebleed that wouldn’t stop. Ended up in the ER. They gave me a lecture. I didn’t cry. I just nodded. Now I use heat packs. Pain’s still there. But I’m alive.
Pranab Daulagupu
December 4, 2025 AT 02:42Topical diclofenac gel is a game-changer for osteoarthritis. Minimal systemic absorption. Safe for most on DOACs. Just avoid open wounds and massive application areas. Talk to your PT-they’ll show you how to use it right.
Barbara McClelland
December 5, 2025 AT 16:15Hey-I’ve been on rivaroxaban for 5 years. I used to take ibuprofen every weekend. Then I started yoga, used a foam roller, and switched to Tylenol. My pain dropped. My anxiety dropped. My doctor was shocked at how much better my INR stabilized.
You don’t have to suffer. You just have to try something new.
Start small. One change. One week. See what happens. You’ve got this.
Alexander Levin
December 5, 2025 AT 23:18They say NSAIDs are dangerous. But what if the real danger is the pharmaceutical industry pushing these drugs so hard that doctors forget to warn us? I think this whole thing is a cover-up. Why else would OTC labels be so vague? They want us bleeding so they can sell more blood transfusions. 🤔
Ady Young
December 7, 2025 AT 07:01I didn’t know this until my dad had a GI bleed. He’d been taking naproxen for 10 years. His doctor never mentioned it. We found out from a nurse in the ER. Now I make sure everyone I know checks their meds. It’s not complicated. Just ask. Just check. Just care.
Travis Freeman
December 7, 2025 AT 07:48As someone from a country where OTC meds are sold without any screening, I can tell you this: the lack of system-wide warnings is terrifying. But the fact that people are sharing this info? That’s hope. Keep talking. Keep educating. Change starts with one person saying, ‘I didn’t know.’
Sean Slevin
December 7, 2025 AT 15:09Let’s be real: the body is not a machine. You can’t just ‘block COX-1’ and expect no consequences. Life is messy. Biology is messy. We’ve been told to treat pain like a bug to be eradicated-but what if pain is a signal? What if we’re treating symptoms instead of causes? Maybe we need to stop reaching for pills… and start listening to our bodies.
...but also, Tylenol is fine. Just don’t overdose.
Chris Taylor
December 7, 2025 AT 21:35My mom’s on apixaban. I showed her this post. She cried. Said her doctor never told her. I made her throw out her ibuprofen. We’re trying heat wraps now. She says it’s weird… but it kinda works.
Melissa Michaels
December 8, 2025 AT 17:25Acetaminophen is the gold standard for analgesia in anticoagulated patients. Clinical guidelines from ACC, AHA, and ESC consistently endorse it. Topical NSAIDs are acceptable for localized pain. Avoid all oral NSAIDs unless absolutely necessary and under close monitoring. Always disclose OTC use. This is not debatable-it’s evidence-based.