Methylnaltrexone: What It Is, How It Works, and What You Need to Know
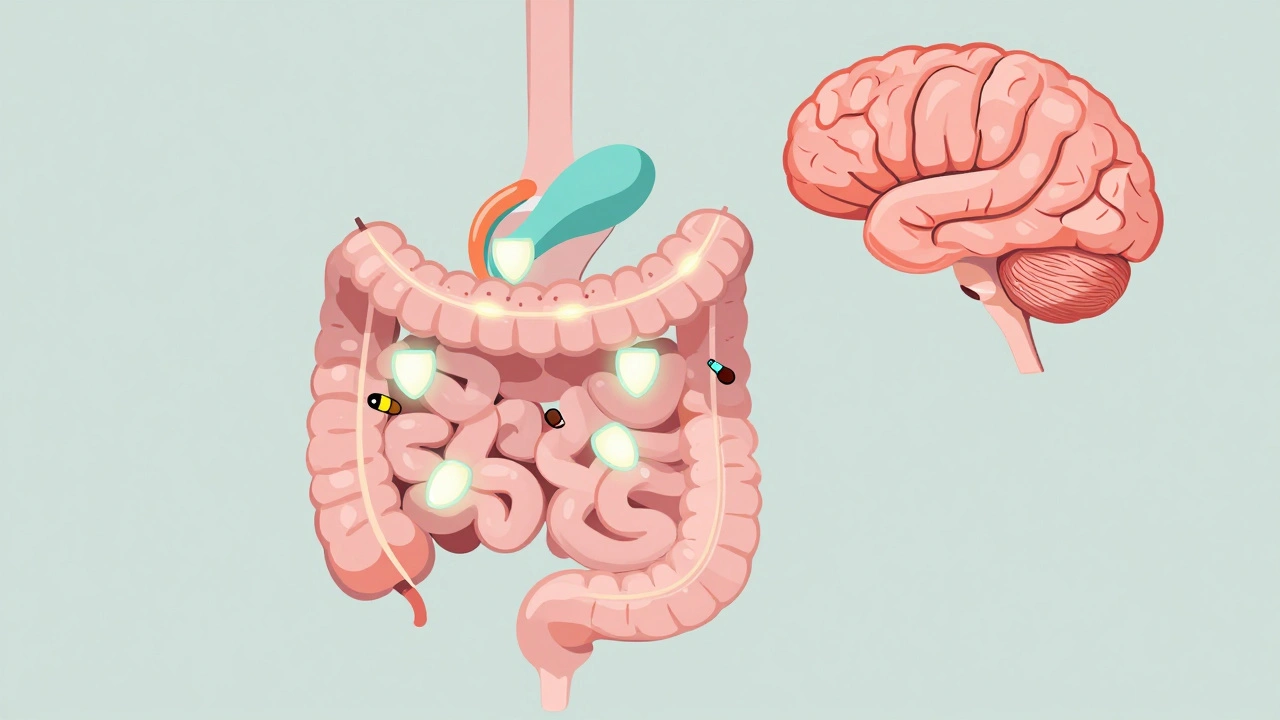
When you’re taking opioids for chronic pain, constipation often comes along as an unwanted side effect. That’s where methylnaltrexone, a peripherally acting mu-opioid receptor antagonist used to treat opioid-induced constipation without affecting pain control. Also known as Relistor, it works by blocking opioid effects in the gut while leaving brain receptors untouched. Unlike laxatives that just stimulate bowel movement, methylnaltrexone targets the root cause — opioids slowing down your digestive system.
This drug is designed for people who’ve tried other treatments and still can’t go. It’s not for everyone. If you have a bowel obstruction, you shouldn’t use it. And it’s not meant for short-term opioid use, like after surgery. It’s for those on long-term opioid therapy — cancer patients, people with chronic pain, or those on high-dose pain meds — whose constipation won’t budge with stool softeners or fiber. Studies show it can produce a bowel movement within 30 minutes to 4 hours for many users, without making their pain worse.
Methylnaltrexone relates closely to naloxone, a similar opioid blocker used to reverse overdoses, but the two work differently. Naloxone crosses the blood-brain barrier and can trigger withdrawal or sudden pain return. Methylnaltrexone doesn’t. That’s why it’s safer for daily use in people who need pain relief. It’s also connected to opioid-induced constipation, a common, often under-treated side effect affecting up to 90% of long-term opioid users. This isn’t just discomfort — it can lead to nausea, loss of appetite, and even hospitalization if ignored.
Many people don’t realize how common this problem is. Doctors often focus on pain control and forget to ask about bowel habits. But constipation from opioids isn’t something you just have to live with. There are options. Methylnaltrexone is one of them — especially when other remedies fail. It’s given as a subcutaneous injection, usually once a day, and is often covered by insurance for qualifying patients.
What you’ll find in the posts below isn’t just about methylnaltrexone. It’s about the bigger picture: how medications interact, how side effects are managed, and what you need to watch for when taking powerful drugs. You’ll see how drugs like levothyroxine and PPIs interfere with absorption, how NSAIDs raise bleeding risks with blood thinners, and how even natural supplements like garlic can change how your meds work. These aren’t isolated issues — they’re part of a system. And understanding that system helps you take control of your health, whether you’re on methylnaltrexone, opioids, or something else entirely.