Generic vs Brand Drug Savings: What You Really Save and Why It Matters
When you pick up a prescription, you might see two options: the familiar brand name and a much cheaper generic. Generic drugs, FDA-approved versions of brand-name medications with identical active ingredients, dosage, and effectiveness. Also known as generic medications, they’re not knockoffs—they’re the exact same medicine, just without the marketing cost. The generic vs brand drug savings aren’t just a little bit better—they’re often 80% cheaper. For someone taking a monthly pill like levothyroxine or metoprolol, that’s hundreds of dollars a year back in your pocket.
But here’s what most people don’t realize: the brand name drugs, medications originally developed and marketed by pharmaceutical companies under a patent aren’t better. They’re the same pills, made in the same factories, sometimes even by the same company. The difference? Packaging, logo, and price tag. The therapeutic equivalence, the scientific guarantee that a generic performs just like its brand-name counterpart in the body isn’t a guess—it’s a legal requirement. The FDA tests generics to make sure they deliver the same amount of medicine into your bloodstream at the same rate. No shortcuts. No compromises.
That’s why switching to generics is safe for most people. But not all meds are created equal. If you’re on a drug with a narrow therapeutic index—like warfarin, lithium, or seizure meds—your doctor might suggest monitoring your levels after the switch. That’s not because generics are less reliable. It’s because tiny changes in blood levels can matter more in these cases. That’s why posts like Monitoring Your Health After Switching to Generics exist: to help you track symptoms, lab results, and even NDC numbers to stay in control.
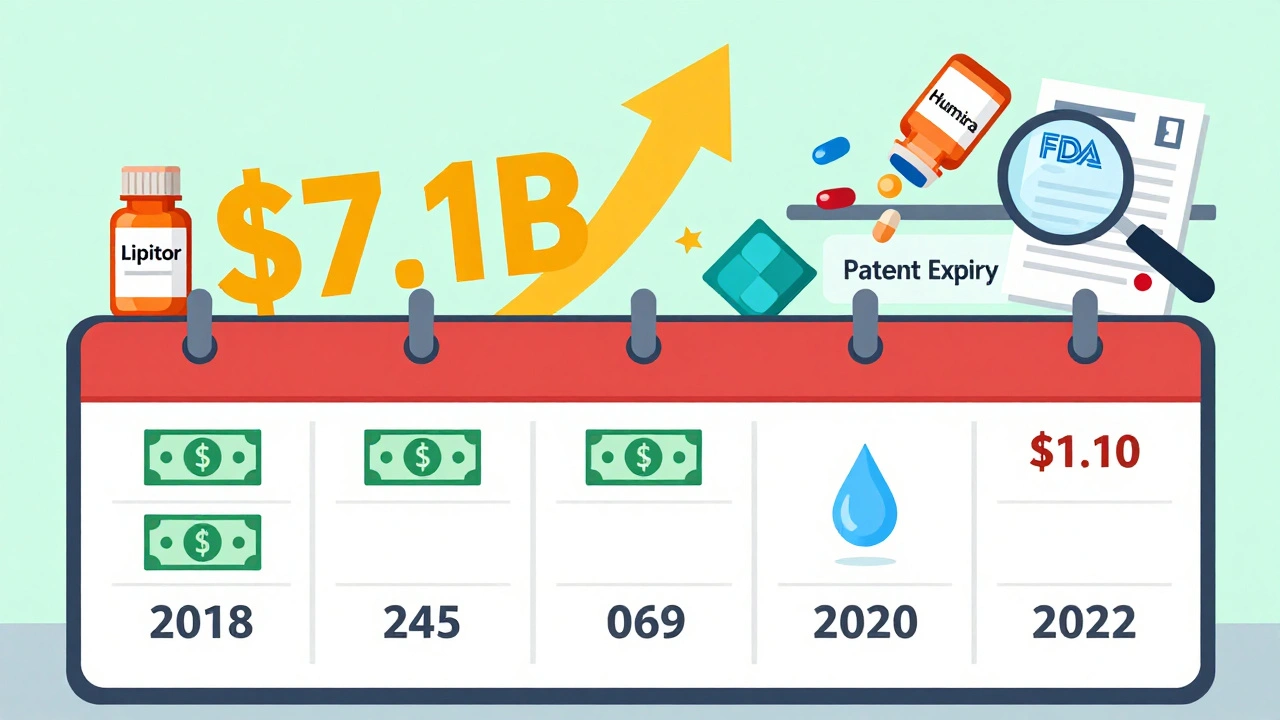
And the savings aren’t just personal. The whole system benefits. When you choose a generic, you’re not just saving money—you’re helping reduce the national drug spending burden. That’s why companies use Paragraph IV certifications, a legal tool under the Hatch-Waxman Act that lets generic makers challenge brand patents early to bring cheaper options to market faster. It’s a system designed to push prices down without sacrificing safety.
Still, confusion lingers. People think generics are "inferior" because they look different or cost less. But that’s like saying a store-brand battery is weaker because it’s not Duracell. The power inside is the same. The same goes for active ingredients, the medically effective components in every pill, whether branded or generic. Whether it’s acetaminophen in Tylenol or ibuprofen in Advil, the molecule doesn’t care what the label says. That’s why reading OTC labels matters—brand names hide the truth, but the Drug Facts label tells you exactly what you’re taking.
So when you see that generic option at the pharmacy, ask yourself: is this really a risk? Or is it just a smarter way to pay less for the same result? The data doesn’t lie. Billions are saved every year because people choose generics. And if you’re on a long-term medication, that’s money you can put toward groceries, rent, or even a vacation. The real question isn’t whether generics work—it’s why you’d ever pay more when you don’t have to.
Below, you’ll find real stories, hard data, and practical advice on how to switch safely, spot hidden costs, and make sure your savings don’t come with hidden risks.