Generic Drug Savings: How Cheaper Medications Cut Costs Without Compromising Care
When you hear generic drug savings, the cost difference between brand-name pills and their generic versions. Also known as generic medication savings, it's one of the most straightforward ways to cut your healthcare bills without giving up quality care. Most people assume generics are knockoffs—cheap, unreliable, maybe even dangerous. But that’s not true. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also prove they work the same way in your body. That’s not luck. That’s science.
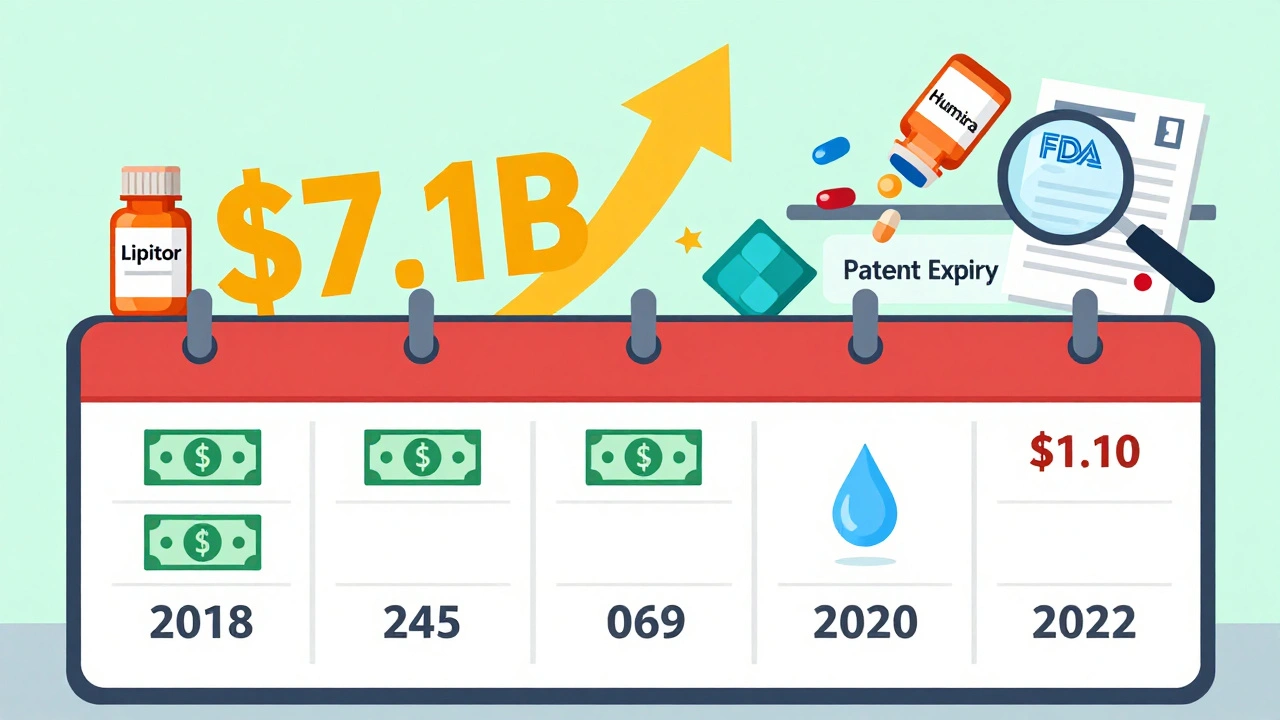
That’s why generic medications, FDA-approved copies of brand-name drugs with identical active ingredients and bioequivalence. Also known as generic drugs, they save patients billions every year. A pill that costs $300 as a brand name? The generic version? Often under $10. And it’s not just for common meds like ibuprofen or metformin. Even complex drugs like levothyroxine or blood thinners have generics that work just as well—when you switch correctly. But here’s the catch: not all switches are equal. If you’re on a drug with a narrow therapeutic index—like warfarin, lithium, or seizure meds—your body is sensitive to tiny changes. That’s why monitoring your health after switching matters. Lab results, symptoms, even the NDC number on the bottle can tell you if the generic is working right for you.
And it’s not just about price. brand name drugs, originally developed medications protected by patents and sold under proprietary names. Also known as originator drugs, they cost more because of marketing, patent protection, and research recovery—not because they’re better. The active ingredient is identical. The pills are made to the same standards. The only real difference? The color, the shape, and the sticker price. You’re not buying better medicine. You’re paying for a logo.
That’s why so many posts here focus on what happens after you switch. From thyroid levels shifting after a generic switch to how PPIs mess with levothyroxine absorption—these aren’t edge cases. They’re everyday realities. And they’re why knowing your meds matters. You don’t need to be a pharmacist to protect yourself. Just learn to read labels, track changes, and ask questions. The FDA inspects generic factories just like brand-name ones. Biosimilars and generics follow different rules, but both are designed to cut costs without cutting corners.
Real savings come from smart choices—not just grabbing the cheapest option. That’s why we cover everything from how Paragraph IV certifications let generics enter the market to why some people need to avoid certain generics if they’re on multiple meds. We’ve got posts on how calcium juice blocks absorption, how garlic supplements interfere with blood thinners, and how to avoid mixing OTC drugs that look harmless but can overdose you. All of it ties back to one thing: knowing what’s in your bottle, why it costs what it does, and how to use it safely.
There’s no magic trick to saving money on meds. Just facts. And the facts are clear: generics work. They’re safe. And they’re the smartest financial move most people make in their healthcare journey. But only if you know how to use them right.
Below, you’ll find real stories, real data, and real advice from people who’ve been there—switching meds, tracking side effects, and learning how to get the same results for a fraction of the cost.