Generic Drug Cost Savings: How Generics Cut Bills Without Sacrificing Quality
When you hear generic drug cost savings, the financial benefit of using FDA-approved versions of brand-name medications. Also known as generic medications, they deliver the same active ingredients, strength, and effectiveness as their brand-name counterparts—but often at a fraction of the price. You’re not getting a cheaper version. You’re getting the exact same medicine, just without the marketing, fancy packaging, or patent protection.
That’s why generic medications, FDA-approved copies of brand-name drugs that meet the same strict standards for safety and performance. Also known as generic drugs, they make up over 90% of prescriptions filled in the U.S. But many people still hesitate, worried they’re compromising on quality. The truth? A 2021 FDA review of over 500 generic drugs found no meaningful difference in how well they worked compared to brand names. For thyroid meds like levothyroxine, blood thinners like warfarin, or seizure drugs like phenytoin, switching to generics is safe—if you monitor your lab results and symptoms, as shown in our post on monitoring your health after switching to generics.
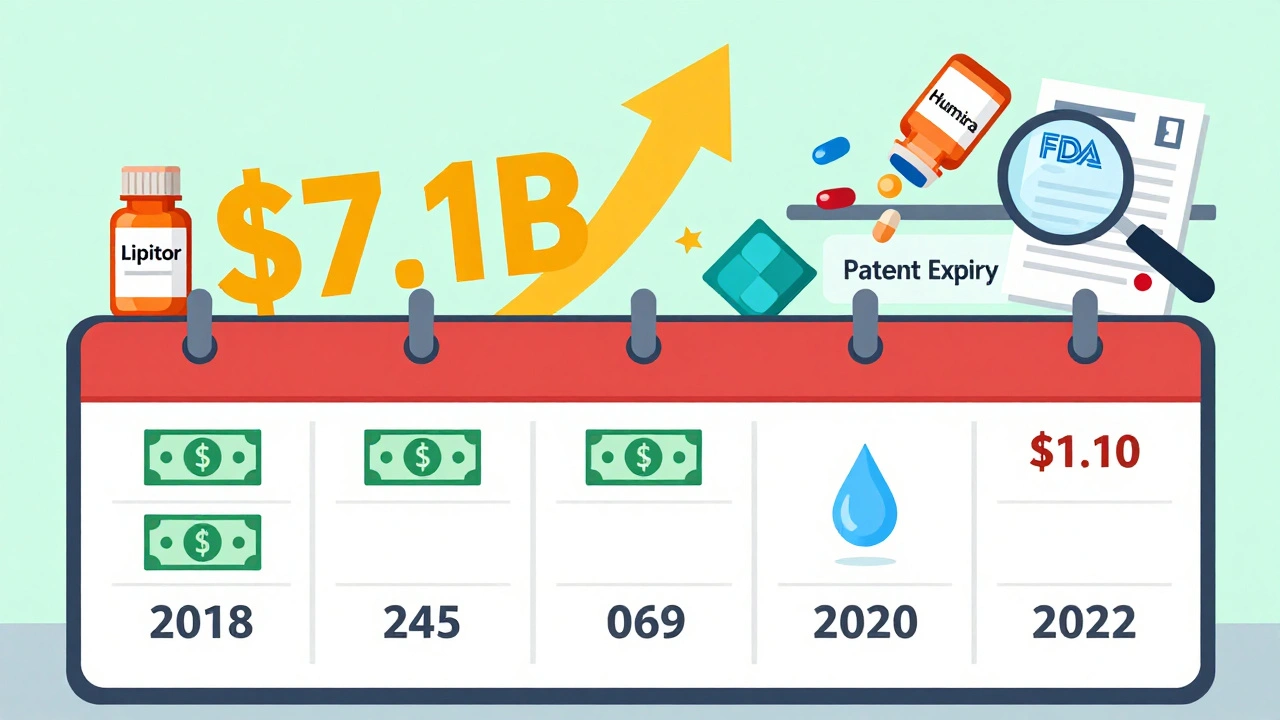
How much can you actually save? On average, generics cost 80% to 85% less than brand-name drugs. A monthly supply of Lipitor might run $300. The generic atorvastatin? Around $10. That’s not a small difference—it’s life-changing for people on fixed incomes or juggling multiple prescriptions. And it’s not just about pills. brand name drugs, medications marketed under a proprietary name, often protected by patents that delay generic competition can cost thousands more over a year. When you factor in insurance copays, deductibles, and out-of-pocket spending, the savings add up fast.
But here’s the catch: not all generics are created equal in perception. Some patients notice subtle differences—like pill color, size, or even how they feel when switching. That’s not because the drug doesn’t work. It’s because inactive ingredients (fillers, dyes, coatings) can vary. For most people, that’s harmless. But for those on drugs with a narrow therapeutic index—where even a small change in blood level can cause problems—tracking your response matters. That’s why our posts cover everything from how generics are approved to what to watch for after switching.
And it’s not just about saving money on your own script. Generic drug cost savings ripple through the whole system. When generics enter the market, they force brand-name companies to lower prices too. That’s why drug price comparison, the practice of evaluating costs between brand-name and generic versions of the same medication is so powerful. It’s not just personal finance—it’s healthcare economics. The Hatch-Waxman Act, which made generics possible, has saved U.S. patients over $3 trillion in the last 20 years. That’s billions saved every single year.
What you’ll find below isn’t just a list of articles. It’s a practical toolkit. You’ll read how generics are tested for therapeutic equivalence, why some people react differently after switching, how to spot fake or substandard versions, and how to talk to your pharmacist about the best low-cost option. You’ll also learn about the legal battles behind the scenes—like Paragraph IV certifications—that let generics hit the market faster. And you’ll see real-world examples: how switching from a $200 brand to a $12 generic for your blood pressure pill can mean the difference between paying for meds or skipping doses.
Generic drug cost savings isn’t a myth. It’s a proven, everyday reality for millions. The question isn’t whether you should switch—it’s how to do it safely and confidently. Below, you’ll find everything you need to make that decision with your eyes wide open.