Barcode Scanning in Pharmaceuticals: How It Keeps Medications Safe and Accurate
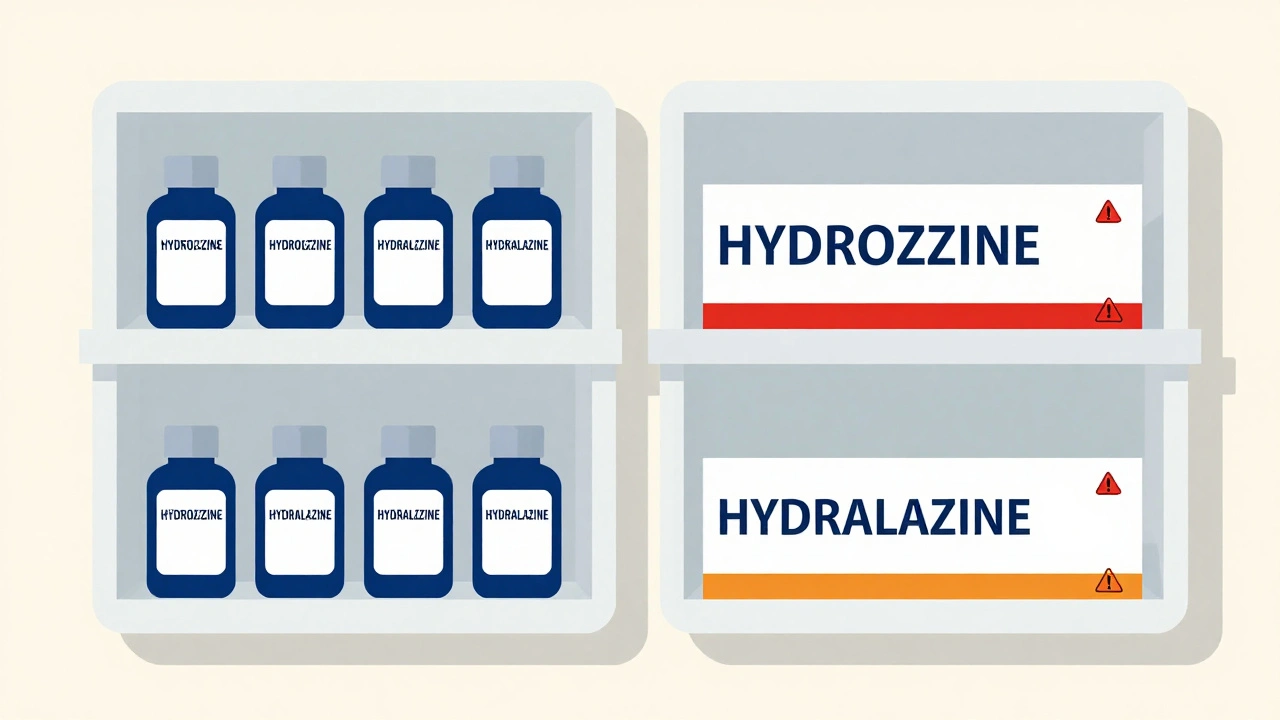
When you pick up a prescription, barcode scanning, a system that reads unique machine-readable codes on drug packaging to confirm identity and dosage. Also known as barcoding in healthcare, it’s not just a tech upgrade—it’s a lifeline that stops wrong meds from reaching patients. Every pill bottle, vial, or box in a U.S. pharmacy carries a barcode tied to its NDC code, a unique 10-digit identifier assigned by the FDA to track every drug product. That code links directly to the drug’s name, strength, manufacturer, and lot number. When a pharmacist scans it, the system checks: Is this the right drug? Is it the right dose? Is it meant for this patient? If anything’s off, the system alerts them before the med leaves the counter.
Barcode scanning doesn’t just help pharmacies—it protects you. Think about how many people take multiple meds. One wrong pill, one misread label, and you could end up in the ER. In 2023, the FDA reported that over 1.5 million medication errors were prevented in U.S. hospitals and pharmacies thanks to barcode systems. That’s not theory. That’s real people avoiding allergic reactions, overdoses, or dangerous interactions. For example, if you’re on levothyroxine and someone accidentally hands you a different thyroid med, the barcode will catch it. Same goes for blood thinners like warfarin or seizure drugs—where even a tiny dose error can be life-threatening. The system also links to your medication history, a digital record of all drugs a patient is taking, updated in real time by providers and pharmacies. This helps spot conflicts, like when someone’s on NSAIDs, a class of pain relievers including ibuprofen and naproxen that can increase bleeding risk when mixed with blood thinners. and gets handed another one.
It’s not perfect. Sometimes the barcode is smudged, the system glitches, or a new generic gets mislabeled. But the data shows: places that use barcode scanning have 40% fewer medication errors than those that don’t. Even the FDA pushes for it. In 2024, new guidelines made it clear: if you’re dispensing meds in a hospital or large pharmacy, scanning barcodes isn’t optional—it’s expected. And it’s not just for prescriptions. OTC drugs like acetaminophen, a common pain reliever found in over 600 products, including cold and flu combos. are now being tracked too, so no one accidentally takes two pills with the same active ingredient. That’s why you see those little black-and-white bars on Advil, Tylenol, and even cough syrups. It’s all part of the same safety net.
What you’ll find below are real stories and breakdowns of how barcode scanning connects to drug safety, generic switching, interactions, and even how the FDA ensures quality. You’ll see how it stops errors before they happen, why NDC codes matter more than brand names, and what happens when the system fails. This isn’t about tech for tech’s sake. It’s about making sure the right pill gets to the right person—every single time.