Why Early Diagnosis of Sickle Cell Anemia Saves Lives
 Oct, 11 2025
Oct, 11 2025
Sickle Cell Screening Cost Calculator
Compare screening options and see how early diagnosis can save lives and healthcare costs
Choose Your Screening Method
Newborn Screening
Within 24-48 hours after birth
Hemoglobin Electrophoresis
Any age, after symptoms
DNA Testing
Pre-conception or prenatal
Estimated Benefits
Early diagnosis reduces mortality by up to 40%
Preventative treatments like hydroxyurea can reduce pain crises by 50%
Newborn screening cuts hospitalizations by 35% compared to late diagnosis
Vaccinations and antibiotics reduce severe infections by up to 70%
Your Screening Impact
Key Takeaways
- Detecting sickle cell anemia before symptoms appear cuts mortality by up to 40%.
- Newborn screening, hemoglobin electrophoresis, and DNA testing are the three primary screening tools.
- Early treatment with hydroxyurea or blood transfusion can prevent pain crises and organ damage.
- Genetic counseling helps families understand inheritance patterns and plan future pregnancies.
- Regular follow‑up and patient education are essential for long‑term health.
When a child or adult learns they have Sickle Cell Anemia is a hereditary blood disorder caused by a mutation in the beta‑globin gene, producing abnormal hemoglobin (HbS) that makes red blood cells rigid and sickle‑shaped, the news can feel overwhelming. But the biggest factor that determines whether that diagnosis leads to a healthier life is *when* it’s made. early diagnosis of sickle cell anemia lets doctors start life‑saving interventions before complications erupt.
How Sickle Cell Anemia Develops
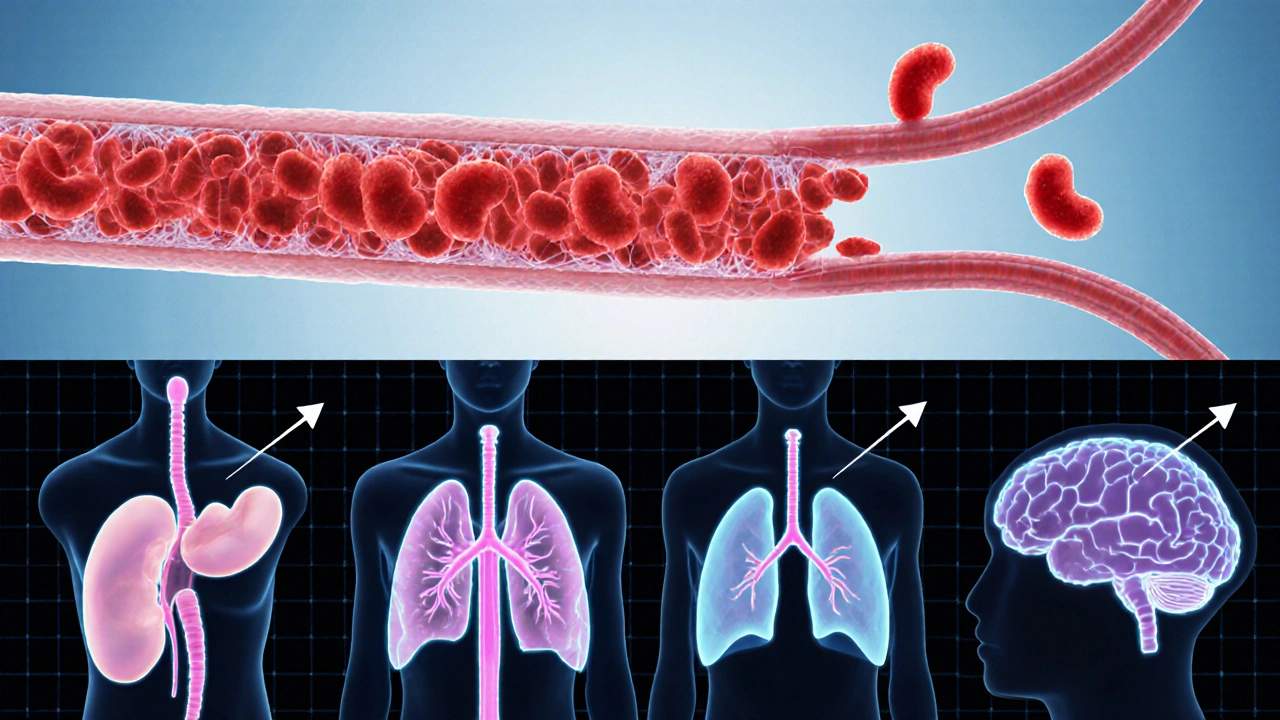
The disease stems from a single nucleotide change (glu‑to‑val) in the HBB gene. That tiny tweak creates hemoglobin S, which polymerizes when oxygen levels drop. The resulting sickle‑shaped cells struggle to flow through tiny capillaries, causing blockages, tissue ischemia, and chronic anemia. Over time, repeated blockages trigger pain crises, damage to the spleen, kidneys, lungs, and even the brain.
Warning Signs That Should Prompt Testing
Because the genetic defect is present from birth, many people don’t notice symptoms until later childhood. Look out for these clues:
- Frequent unexplained fatigue or pallor.
- Recurring episodes of severe pain in the limbs, chest, or abdomen.
- Delayed growth or puberty.
- History of infections that seem unusually severe, especially in early childhood.
- Family members diagnosed with sickle cell disease or trait.
If any of these appear, a quick test can confirm the diagnosis.
Screening Options: What’s Available and How They Differ
Three main methods dominate the screening landscape. The table below breaks down their key attributes.
| Method | When Used | Accuracy | Result Turnaround | Typical Cost (USD) |
|---|---|---|---|---|
| Newborn screening | Within 24‑48hours after birth | ≈99% for detecting HbS | 1‑2weeks | ≈$25 |
| Hemoglobin electrophoresis | Any age, usually after symptoms appear | ≈95% for confirming variants (HbS, HbC, HbF) | 3‑5days | ≈$45 |
| DNA testing (PCR or NGS) | Pre‑conception, prenatal, or confirmatory | ≈99.9% for detecting the HBB mutation | 1‑2weeks | ≈$150 |
All three methods reliably detect the disease, but newborn screening offers the earliest chance to act-often before the first painful crisis ever happens.
Why Early Diagnosis Matters: The Tangible Benefits
Once a diagnosis is in hand, clinicians can tailor a care plan that dramatically improves quality of life. Here’s what early detection unlocks:
- Preventive medication. Starting Hydroxyurea as early as age 9 (or even younger in high‑risk cases) raises fetal hemoglobin levels, reducing pain episodes by up to 50%.
- Vaccination schedule. Children with sickle cell are more vulnerable to encapsulated bacteria. Early diagnosis ensures timely pneumococcal and meningococcal vaccines.
- Prophylactic antibiotics. Penicillin prophylaxis from infancy cuts septicemia risk dramatically.
- Transfusion planning. For high‑risk newborns, scheduled blood transfusions can prevent stroke-a leading cause of mortality in pediatric sickle cell.
- Family education. Parents learn how to recognize early signs of a crisis, when to seek care, and how to manage hydration and temperature.
Data from the CDC’s 2023 Sickle Cell Registry show a 35% drop in hospitalizations for children diagnosed through newborn screening compared with those identified after symptom onset.
What Happens After a Positive Test?
The moment a lab confirms sickle cell, a coordinated care pathway kicks in.
- Genetic counseling. A certified counselor explains inheritance (autosomal recessive), discusses reproductive options, and offers testing for siblings.
- Baseline health assessment. Complete blood count, renal function, liver enzymes, and transcranial Doppler ultrasound are ordered to gauge organ status.
- Individualized treatment plan. Based on age, disease severity, and family preferences, doctors may start hydroxyurea, schedule chronic transfusions, or consider emerging gene‑editing trials.
- Education and self‑management tools. Families receive a “pain crisis action plan,” hydration guidelines, and a list of emergency contacts.
Each step is documented in the patient’s electronic health record, ensuring that every specialist-from hematology to neurology-has a unified view of the case.
Common Pitfalls and How to Avoid Them
Even with screening programs, gaps happen. Recognize and sidestep these mistakes:
- Assuming a negative newborn screen means the baby is fine. Rare variants (like HbS‑beta‑thalassemia) can be missed; a follow‑up hemoglobin electrophoresis at 6months is advisable for high‑risk families.
- Delaying hydroxyurea because of fear of side effects. Regular monitoring of blood counts mitigates risk; most patients tolerate the drug well.
- Skipping routine transcranial Doppler scans. These detect silent strokes early; missing them can lead to irreversible brain injury.
- Neglecting psychosocial support. Chronic disease can cause anxiety and depression; early referral to mental‑health services improves adherence.
Staying vigilant about these issues keeps the care plan on track.

Future Directions: From Early Diagnosis to Curative Therapies
Early detection isn’t just about managing symptoms-it also opens doors to curative options that are still emerging.
- Gene therapy. CRISPR‑based trials in 2024 showed >80% of participants achieved transfusion‑independence after a single infusion.
- Bone‑marrow transplant. When performed before major organ damage, success rates exceed 90%.
- Pre‑implantation genetic diagnosis (PGD). Couples with a known carrier status can select embryos without the HBB mutation, preventing disease transmission entirely.
All of these pathways rely on a confirmed diagnosis early enough to keep organ function intact.
Take Action Today
If you or a lovedone belong to a high‑risk ethnic group (African, Mediterranean, Middle Eastern, or Indian ancestry), ask your pediatrician about newborn screening or request a hemoglobin electrophoresis. For adults, a simple blood test can confirm status before planning a family.
Remember, the sooner the disease is identified, the more tools you have to stay healthy.
Frequently Asked Questions
What age is newborn screening for sickle cell performed?
Most U.S. states collect a few drops of blood from a heel prick within the first 24‑48hours after birth. The sample is sent to a state lab for hemoglobin analysis.
Can adults be screened if they missed newborn testing?
Yes. A simple blood draw for hemoglobin electrophoresis or DNA testing can determine carrier or disease status at any age.
Is hydroxyurea safe for children?
Clinical trials and long‑term studies have shown it is well‑tolerated. Doctors monitor blood counts every 4‑8weeks to catch any rare side effects early.
How often should a person with sickle cell get a transcranial Doppler scan?
Guidelines recommend an initial scan before age 5, then annually if velocities are elevated, or every 2‑3years if results are normal.
Can sickle cell be cured?
Bone‑marrow transplant can cure the disease but carries significant risks. Gene‑editing therapies are promising and may become curative options within the next decade, especially when started early.
Brufsky Oxford
October 11, 2025 AT 20:56When we stare at the numbers on a newborn screen, we’re really peering into a future that could be rewritten with a single early test 😊. The biology of sickle cell is relentless, yet the moment we catch that HBB mutation before pain spikes, we gain a sliver of mercy that stretches into years of healthier living. It’s not just about saving lives; it’s about gifting families the chance to plan, to dream, and to watch their children grow without the shadow of preventable crises. In that tiny blood drop lies a paradox – a genetic flaw that, if identified early, becomes a catalyst for proactive care, turning destiny into choice.
Lisa Friedman
October 20, 2025 AT 19:26The CDC data actually shows a 35% drop in hospitalizations for children caught via newborn screening versus those diagnosed after symptoms appear. Its important to note that the cost‑benefit analysis factors in not just immediate savings but long‑term reductions in organ damage and mortality rates.
cris wasala
October 29, 2025 AT 16:56Hey folks, if you or someone you know is from a high‑risk background get that test done early the support system is there and you’ll have a whole team ready to guide you through the steps we’ve all learned from experience
Tyler Johnson
November 7, 2025 AT 15:26Early diagnosis of sickle cell anemia is a cornerstone of modern hematology that cannot be overstated. The data from recent registries consistently demonstrate that children screened at birth experience significantly fewer vaso‑occlusive crises. This reduction in pain episodes translates directly into decreased hospital admissions, which eases the burden on both families and the healthcare system. Moreover, initiating hydroxyurea therapy before the first crisis has been shown to raise fetal hemoglobin levels and cut the frequency of painful events by roughly half. Vaccination schedules, particularly against encapsulated organisms, become more effective when administered on a known diagnosis timeline. Prophylactic penicillin, started in infancy, dramatically lowers the risk of sepsis, a leading cause of mortality in untreated sickle cell patients. For those with high‑risk transcranial Doppler velocities, regular blood transfusions can prevent silent strokes, preserving cognitive function into adulthood. The psychosocial benefits are equally important; families who know the diagnosis early report lower anxiety and higher confidence in managing emergencies. Genetic counseling, offered promptly after a positive screen, empowers parents with information about inheritance patterns and reproductive options. In regions where newborn screening is universal, the overall life expectancy for sickle cell patients has risen by several years compared to areas lacking such programs. Economic analyses reveal that the upfront cost of a $25 heel‑prick test is offset many times over by savings in avoided hospital stays and emergency care. Importantly, early detection keeps patients eligible for emerging curative therapies such as gene editing and bone‑marrow transplantation before organ damage accrues. Clinicians should therefore advocate for mandatory newborn screening as a public health priority, reinforcing the message that early knowledge saves both lives and resources. Communities must remain vigilant, ensuring that follow‑up testing at six months catches any atypical hemoglobin variants that could be missed initially. Ultimately, the simple act of testing at birth opens a pathway to comprehensive, life‑saving care that transforms a potentially tragic diagnosis into a manageable chronic condition.
Annie Thompson
November 16, 2025 AT 13:56Reading through the statistics feels like swallowing a bitter pill, yet the reality is that each percentage point represents a child whose future could be dramatically altered. When I think about the families who miss that early window, I can’t help but feel the weight of lost opportunities, the quiet grief that stays hidden behind hospital doors. The numbers on mortality reduction are not just abstract; they are the echo of countless stories where a simple heel‑prick could have lightened a lifetime of suffering. It’s a stark reminder that our healthcare system must prioritize equitable access to these screenings, because every delay feels like a betrayal to those waiting in the shadows.
Parth Gohil
November 25, 2025 AT 12:26From a health‑systems perspective, the cost‑effectiveness ratio of newborn screening for sickle cell is compelling; the incremental cost‑utility analysis yields an ICER well below typical willingness‑to‑pay thresholds, especially when you factor in QALY gains from reduced vaso‑occlusive events and lower transfusion dependence.
VAISHAKH Chandran
December 4, 2025 AT 10:56Honestly the whole debate is just Western elites trying to overcomplicate a simple public health measure
Pat Merrill
December 13, 2025 AT 09:26Sure, because spending $25 on a heel prick is obviously a waste of taxpayers' money-said no rational person who has ever seen a child avoid a painful crisis.
Vicki Roth
December 22, 2025 AT 07:56Early screening truly changes the trajectory for many patients.
Vishal Bhosale
December 31, 2025 AT 06:26Looks like another hype article trying to sell a thing that already exists.
Garima Gauttam
January 9, 2026 AT 04:56If we keep focusing on early detection we might ignore the root causes of health inequity.
Georgia Nightingale
January 18, 2026 AT 03:26Everyone’s acting like this is the end of the world, but the data is clear: early diagnosis saves lives, even if some prefer to keep living in denial.
Chris Kivel
January 27, 2026 AT 01:56It’s great to see tools that let families visualize potential savings and benefits – keeps the conversation practical and hopeful.
sonia sodano
February 5, 2026 AT 00:26While the calculator looks neat, numbers alone can’t capture the emotional toll families endure when dealing with chronic disease.
Praveen Kumar BK
February 13, 2026 AT 22:56The long‑winded essay is fine but it overlooks the fact that many guidelines still lack clarity on follow‑up protocols after a positive newborn screen.
Viji Sulochana
February 22, 2026 AT 21:26Good points but watch out for those little typos – they can change meaning, especially in medical docs.