When to Seek Emergency Care: Red Flags and Symptoms from Medications
 Jan, 19 2026
Jan, 19 2026
Medication Emergency Symptom Checker
Symptom Assessment Tool
Enter the symptoms you're experiencing after taking any medication. This tool will help you determine if you need immediate emergency care.
Important Information
Emergency signs: If you experience any red flag symptoms from the article, call 911 immediately. These include difficulty breathing, swelling, blue skin, sudden chest pain, stroke symptoms, high fever with rash, uncontrollable vomiting, abnormal heart rate, severe high blood pressure, or loss of consciousness.
When to see a doctor: Mild symptoms like a localized rash, headache, nausea, or fatigue may not require emergency care but should be reported to your doctor within 24 hours.
Remember: Your body knows when something is wrong. If you feel something is "wrong" rather than just uncomfortable, trust your instincts and seek medical help.
Every year, more than 106,000 people in the U.S. die from reactions to medications. Many of these deaths aren’t from overdoses-they’re from symptoms people ignored because they didn’t know what was dangerous. If you’re taking even one prescription drug, you need to know the medication emergency signs that demand immediate action. Waiting could cost you your life.
What Counts as a Medication Emergency?
Not every side effect is an emergency. Nausea after taking antibiotics? Common. Trouble breathing after taking penicillin? That’s a 911 call. The difference lies in how your body reacts-and how fast it escalates. Adverse drug reactions (ADRs) happen when your body responds badly to a medication. Some are mild, like a rash or dizziness. Others are life-threatening. The FDA defines serious reactions as those that cause death, hospitalization, permanent damage, or birth defects. The key is recognizing the red flags before it’s too late.Life-Threatening Symptoms That Need Immediate Care
These symptoms don’t wait. If you or someone you know experiences any of these after starting a new medication or changing a dose, call 911 right away:- Difficulty breathing or wheezing-Even if it feels like a cold, if your airway is tightening, it could be anaphylaxis.
- Swelling of the lips, tongue, or throat-This can block your airway within minutes. Don’t wait to see if it gets better.
- Cyanosis-Blue or gray lips, fingernails, or skin means your body isn’t getting enough oxygen.
- Sudden severe chest pain-Especially if it radiates to your arm, jaw, or back. Could be a heart attack triggered by a drug interaction.
- Slurred speech, weakness on one side of the body, or sudden confusion-These are stroke signs. Medications like blood thinners can cause bleeding in the brain.
- High fever (102°F or higher) with rash or blistering skin-Could be Stevens-Johnson Syndrome, a rare but deadly reaction to antibiotics, seizure meds, or NSAIDs.
- Uncontrollable vomiting or diarrhea-Especially if you’re dizzy, can’t keep fluids down, or your urine is dark or gone for 12+ hours. Dehydration from meds can crash your system.
- Heart rate below 50 or above 110 beats per minute-Especially if you feel faint, dizzy, or short of breath.
- Blood pressure over 180/120 with headache, vision changes, or nausea-This isn’t just high blood pressure. It’s a hypertensive emergency.
- Loss of consciousness or collapse-No matter how minor the medication seems, if you pass out, it’s an emergency.
Common Medications That Trigger Serious Reactions
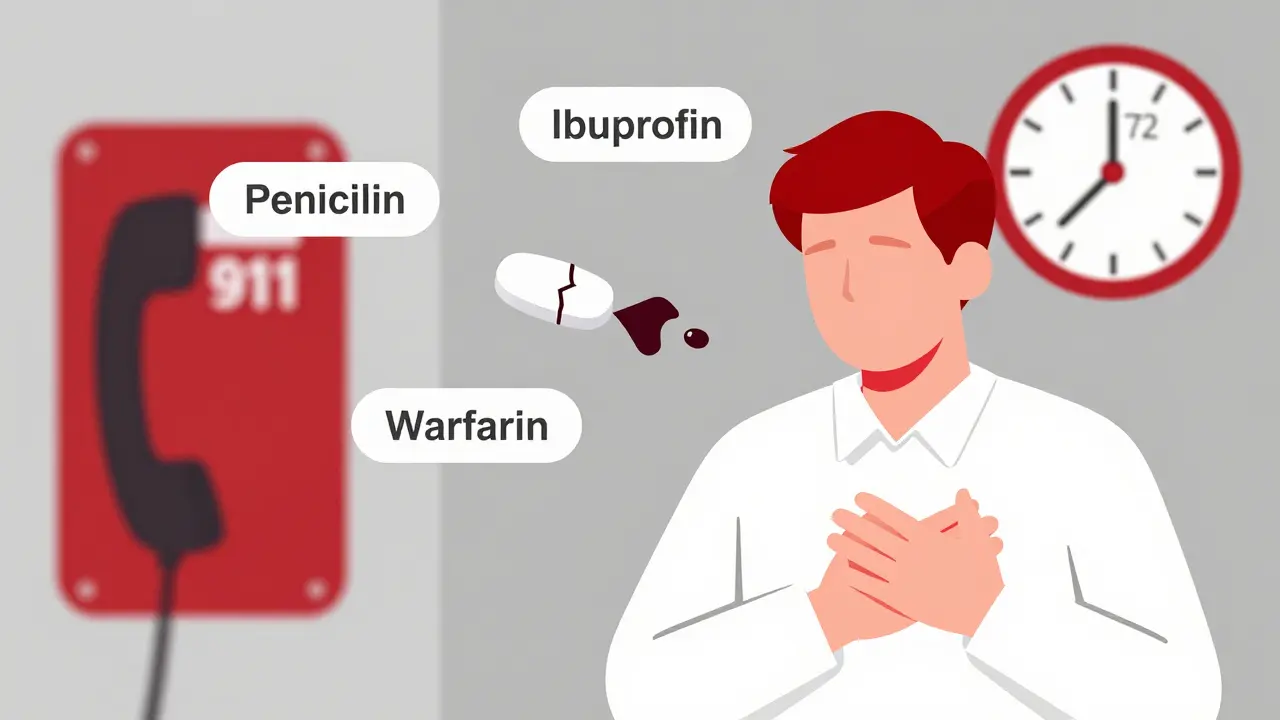
Some drugs are riskier than others. Penicillin causes the most common severe allergic reactions. But other everyday meds carry hidden dangers:- Antibiotics (amoxicillin, sulfa drugs)-Can trigger anaphylaxis or Stevens-Johnson Syndrome.
- NSAIDs (ibuprofen, naproxen)-Increase bleeding risk when taken with blood thinners like warfarin. Studies show this combo raises bleeding risk by 50%.
- Anticoagulants (warfarin, rivaroxaban)-Interact with antibiotics like ciprofloxacin, causing INR levels to spike dangerously within 24-48 hours. This can lead to internal bleeding or stroke.
- Insulin and diabetes drugs-Can cause severe hypoglycemia if combined with certain heart or kidney meds.
- Barbiturates and seizure meds-Linked to deadly skin reactions.
- Herbal supplements-St. John’s Wort can make antidepressants, birth control, or blood thinners dangerously strong or weak.
Over 15,000 drug interactions are documented. About 700 of them are serious enough to cause death if ignored. If you take three or more medications daily, your risk jumps. If you take five or more, your chance of a severe reaction triples.
What’s Not an Emergency (But Still Needs Attention)
Not every weird feeling means the ER. Some reactions are annoying-but not deadly:- Mild rash without swelling or breathing trouble
- Headache after starting a new blood pressure med (could just be adjusting)
- Nausea or upset stomach with antibiotics (usually fades in a few days)
- Fatigue or drowsiness from antihistamines or sleep aids
Still, don’t ignore these. Call your doctor or pharmacist within 24 hours. But if you’re unsure, err on the side of caution. It’s better to be checked than to wait until it’s too late.
Why People Delay-And Why That’s Deadly
A 2023 Mayo Clinic survey found 61% of patients didn’t know when their reaction needed emergency care. Many think:- “It’s just a side effect-I’ve had this before.”
- “I’ll wait and see if it gets better.”
- “I don’t want to bother the doctor.”
- “It’s probably just stress.”
But here’s the truth: 68% of severe reactions happen within 72 hours of starting a new med or changing the dose. The most dangerous reactions mimic other illnesses-like a heart attack, stroke, or infection. That’s why doctors miss them. One patient had abdominal pain and dizziness after starting a new antibiotic. They were treated for a stomach bug. It turned out to be a ruptured aortic aneurysm.
And here’s another scary stat: 35% of anaphylaxis cases are misdiagnosed as asthma or panic attacks. That delay costs lives. Epinephrine works best if given within minutes. Waiting even an hour can turn a survivable reaction into a fatal one.
What to Do If You Suspect a Medication Emergency
1. Stop the medication-If you’re sure it’s the cause, but only if you can do so safely. Don’t stop life-saving drugs like blood thinners or insulin without medical advice. 2. Call 911-Don’t drive yourself. Emergency crews can start treatment on the way. 3. Have your meds ready-Bring the pill bottles or a list of everything you’re taking-including supplements, vitamins, and over-the-counter drugs. 4. Use an epinephrine auto-injector if you have one-If you’re allergic to penicillin, bee stings, or other triggers, and you have an EpiPen, use it immediately. Then call 911 anyway. The reaction can come back. 5. Don’t rely on online symptom checkers-They’re useful for mild issues, but they can’t detect internal bleeding, anaphylaxis, or brain bleeds.
How to Prevent Medication Emergencies
Prevention starts before you even take the pill:- Get a full med review-Ask your pharmacist to check all your meds (including supplements) for dangerous interactions. Medicare Part D now covers this service for high-risk patients.
- Know your triggers-If you’ve had a reaction before, write it down. Tell every new doctor. Don’t assume they’ll check your history.
- Use one pharmacy-It helps them spot interactions across all your prescriptions.
- Ask: “What symptoms mean I need to go to the ER?”-Most patients never ask this. 58% of doctors don’t volunteer the info. Be the one to ask.
- Set alerts-Use your phone to remind yourself when you start a new med. Mark the next 72 hours as high-risk.
Pharmacists who give clear safety instructions reduce emergency visits by 27%. That’s not a small number. It’s lives saved.
What’s Changing in Medication Safety
The system is improving. The FDA now requires stronger emergency warning labels on 78% of new drugs-up from 42% in 2018. AI tools are being tested to predict your personal risk based on your genes and meds, with 82% accuracy in early trials. Pharmacist-led medication management programs are cutting ER visits by 18% in Medicare patients.But the biggest gap isn’t technology-it’s education. Only 42% of patients get clear instructions on when to seek emergency care. That’s on the system. But you can fix it for yourself.
Final Reminder: When in Doubt, Go
You don’t need to be an expert to save your life. If you feel something is wrong-not just uncomfortable, but wrong-trust that feeling. Your body knows. Don’t rationalize it away. Don’t wait for a second opinion. Don’t worry about being a bother.Emergency care for medication reactions isn’t about being dramatic. It’s about being smart. One call could mean the difference between recovery and death. Know the signs. Know your meds. And when in doubt-call 911.
Can a medication reaction happen days after starting the drug?
Yes. While 68% of severe reactions happen within 72 hours of starting or changing a dose, some can take days or even weeks. Skin reactions like Stevens-Johnson Syndrome often appear 1-3 weeks after starting a drug. Blood thinners can cause delayed internal bleeding. Always monitor your body for new symptoms, even if you’ve been on the medication for a while.
Is it safe to take over-the-counter painkillers with my prescription meds?
Not always. NSAIDs like ibuprofen and naproxen can dangerously increase bleeding risk when taken with blood thinners like warfarin or aspirin. They can also raise blood pressure and damage kidneys when combined with certain heart or diabetes drugs. Always check with your pharmacist before mixing OTC meds with prescriptions-even if they seem harmless.
What should I do if I miss a dose and then feel worse?
Missing a dose can cause rebound effects. For example, skipping blood pressure meds can cause a sudden spike. Stopping antidepressants abruptly can trigger severe anxiety or seizures. Never double up to make up for a missed dose. Call your doctor or pharmacist for instructions. If you feel chest pain, dizziness, or confusion after missing a dose, seek emergency care immediately.
Can herbal supplements cause dangerous reactions?
Absolutely. St. John’s Wort can make birth control fail, reduce the effectiveness of antidepressants, and interfere with heart meds. Garlic, ginkgo, and ginseng can increase bleeding risk when taken with blood thinners. Many people assume supplements are “natural” so they’re safe-but they’re drugs too. Always tell your doctor and pharmacist what you’re taking, even if it’s labeled “herbal” or “dietary.”
How do I know if my rash is an allergic reaction or just irritation?
A mild, itchy rash that stays localized is often just irritation. But if the rash spreads quickly, blisters, peels, or affects your mouth, eyes, or genitals, it could be Stevens-Johnson Syndrome-a medical emergency. Add swelling, fever, or trouble breathing, and you’re in danger zone. Don’t wait. Get checked immediately.
Should I keep an epinephrine auto-injector if I’ve had a mild reaction before?
Yes. Even a mild allergic reaction can become severe the next time you’re exposed. If you’ve ever had swelling, hives, or breathing trouble after a medication, talk to your doctor about getting an EpiPen. It’s a simple, life-saving tool. Studies show 89% of anaphylaxis survivors credit immediate epinephrine use with saving their lives.
Are older adults at higher risk for medication emergencies?
Yes. Nearly half of Americans over 65 take five or more medications daily. This increases the risk of dangerous interactions. Older bodies also process drugs slower, so side effects last longer and hit harder. Kidney and liver function decline with age, making toxicity more likely. Regular med reviews with a pharmacist are critical for seniors.
Carolyn Rose Meszaros
January 20, 2026 AT 07:05Greg Robertson
January 21, 2026 AT 14:17Crystal August
January 22, 2026 AT 00:47pragya mishra
January 23, 2026 AT 01:27Edith Brederode
January 23, 2026 AT 11:10Arlene Mathison
January 24, 2026 AT 15:53Emily Leigh
January 24, 2026 AT 17:20Renee Stringer
January 25, 2026 AT 04:12Courtney Carra
January 26, 2026 AT 08:01Andy Thompson
January 26, 2026 AT 08:59thomas wall
January 26, 2026 AT 18:15Shane McGriff
January 28, 2026 AT 10:26Paul Barnes
January 28, 2026 AT 17:28