Urticaria and Angioedema Treatment: Acute and Chronic Hives Guide
 Dec, 26 2025
Dec, 26 2025
Urticaria and angioedema are not just itchy skin rashes-they can be life-threatening if they affect your airway. You might wake up with swollen lips, or notice raised, red welts covering your arms after taking a new medication. If you’ve been told it’s "just hives," but the swelling won’t go away after weeks, you’re not imagining things. This isn’t simple allergy stuff. It’s a complex immune reaction, and treating it wrong can make things worse.
What’s the difference between hives and angioedema?
Urticaria-commonly called hives-shows up as red, raised, itchy welts on the skin. They come and go, sometimes within hours. You might get them after eating shellfish, taking ibuprofen, or even after a hot shower. These are histamine-driven. The mast cells in your skin release histamine, which makes blood vessels leak fluid into the tissue, causing the swellings.
Angioedema is deeper. It’s swelling under the skin, often around the eyes, lips, tongue, throat, or even inside the gut. It doesn’t always itch. In fact, if it’s painless and doesn’t itch, it’s likely not histamine-related. That’s critical. Most people assume all swelling from hives is the same. It’s not. About 10-20% of people with hives also get angioedema. But if you have angioedema alone-with no hives-that’s usually a different problem entirely.
Acute vs. chronic: timing changes everything
If your hives or swelling last less than six weeks, it’s acute. Acute cases often have a clear trigger: a new antibiotic, a bee sting, a food you ate, or an ACE inhibitor like lisinopril. These are the easiest to fix-you stop the trigger, and symptoms usually fade in 24 to 48 hours.
If it’s been going on longer than six weeks, it’s chronic. Chronic spontaneous urticaria (CSU) is the most common form, making up 75-80% of all chronic cases. In most of these, doctors can’t find a cause. No food allergy. No medication. No infection. Just your immune system overreacting for no clear reason. That’s frustrating, but it’s common. About 1% of people worldwide develop chronic hives at some point.
First-line treatment: antihistamines (but not all are equal)
For both acute and chronic hives, the first step is always a non-sedating H1-antihistamine. That means drugs like cetirizine (Zyrtec), loratadine (Claritin), or fexofenadine (Allegra). These aren’t just "over-the-counter allergy pills." They’re the backbone of treatment.
At standard doses-10 mg of cetirizine once a day-they work for about 50-60% of people. But here’s what most doctors don’t tell you: if it’s not working, double or quadruple the dose. The British Society for Allergy and Clinical Immunology and NICE guidelines say it’s safe. You can take up to 40 mg of cetirizine daily, or 540 mg of fexofenadine. That’s three times the normal dose. Studies show response rates jump to 70-80% with higher doses.
Don’t wait weeks to increase it. If you’re still breaking out after 7 days on 10 mg, talk to your doctor about going to 20 mg. Many patients get relief at 20-30 mg, not 10 mg.
When angioedema shows up: stop everything and assess
If you have swelling in your throat, tongue, or difficulty breathing-this is an emergency. But not all angioedema needs epinephrine or steroids.
There are two types:
- Histamine-mediated: Happens with hives. Itches. Responds to antihistamines, epinephrine, and steroids.
- Bradykinin-mediated: No itching. Just deep swelling. Caused by ACE inhibitors (like lisinopril, enalapril), hereditary angioedema (HAE), or rarely, other drugs like DPP4 inhibitors (gliptins).
If you’re on an ACE inhibitor and get angioedema, stop it immediately. No exceptions. Symptoms can take weeks to fade, but they will. The AAEM guideline says: discontinuing the drug is the single most important step. And no, switching to an ARB (like losartan) is not risk-free-about 10% of people on ARBs still get angioedema. But it’s better than ACE inhibitors.
Here’s the hard truth: if it’s bradykinin-mediated, antihistamines, epinephrine, and steroids do nothing. They won’t help. They just add side effects. The only treatments that work are C1 esterase inhibitor concentrates, icatibant, or ecallantide-these are hospital-administered drugs for rare genetic conditions. If you don’t have a known genetic cause and you’re on an ACE inhibitor, your treatment is: stop the drug, monitor your airway, and wait.

When steroids help-and when they don’t
Oral corticosteroids like prednisone (40-60 mg daily for 5-10 days) are often given in acute cases with severe swelling or laryngeal involvement. But here’s what most patients don’t know: steroids don’t help bradykinin angioedema. They also don’t speed up recovery in chronic hives.
Using them long-term is dangerous. Weight gain, bone loss, high blood sugar, mood swings-they add up. The 2021 AAEM guideline and Dr. E. Macy’s analysis both warn: avoid steroids beyond 10 days. They’re a bridge, not a solution. Use them for acute flare-ups only, and never for chronic hives unless you’re out of other options.
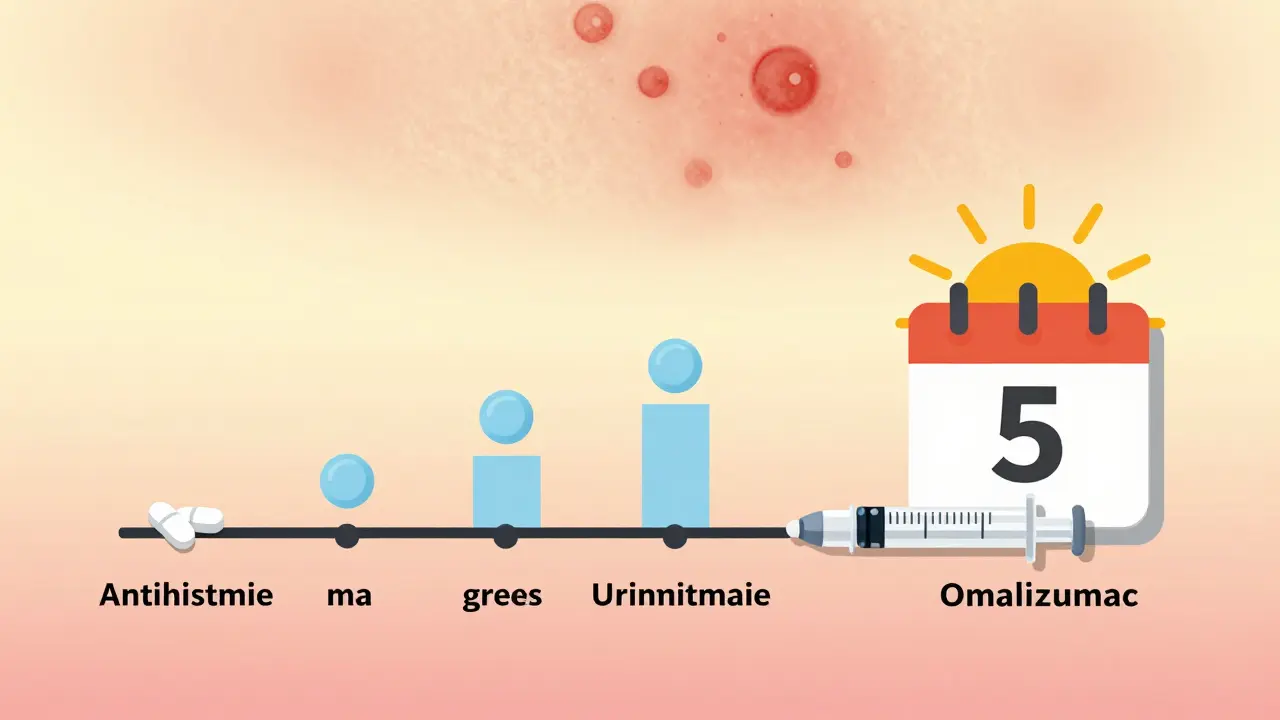
What if antihistamines don’t work?
If you’ve tried high-dose antihistamines for 4-6 weeks and still have hives, it’s time to step up. The next step is omalizumab (Xolair). This is an injectable biologic, originally for asthma, but now approved for chronic hives that don’t respond to antihistamines.
It works by blocking IgE, the antibody that triggers mast cells. Studies show 60-70% of patients get significant improvement. You get a shot every 4 weeks. It’s expensive-around £1,200 per month in the UK-but covered by most insurance if you meet criteria. You need a referral to an allergy specialist to get it.
Other options include montelukast (Singulair), which is sometimes added for patients who react to NSAIDs. It’s not as strong as omalizumab, but it’s cheap and safe. Some people also benefit from cyclosporine or dapsone, but those are last-resort options with more side effects.
What to avoid: hidden triggers
Even if you’re on medication, you can still flare up. Here are common triggers you might not know about:
- NSAIDs (ibuprofen, naproxen): Trigger flares in 20-30% of chronic hives patients. Use paracetamol instead.
- Alcohol: Can worsen symptoms, especially in chronic cases.
- Stress: Emotional stress is a well-documented trigger. Not the cause-but a major amplifier.
- Hot showers, tight clothes, sweating: Physical urticaria. If heat makes you break out, you might have cholinergic urticaria.
- DPP4 inhibitors (gliptins): Diabetes drugs like sitagliptin can cause angioedema in 0.1-0.3% of users. If you’re on one and get swelling, ask your doctor to switch.
Keep a symptom diary. Note what you ate, what meds you took, how stressed you felt, and when the hives appeared. Patterns emerge over time.
Chronic hives: long-term management
Chronic hives can last years. But here’s the good news: 65-75% of people go into remission within 5 years, even without treatment. The goal isn’t to cure it overnight-it’s to control it until your body calms down.
Once your symptoms are under control for 3-6 months, start weaning off antihistamines. Reduce by one tablet every 6-8 weeks. If hives come back, go back to the previous dose. Don’t stop cold turkey. Many people can eventually stop all meds.
During pregnancy or breastfeeding, cetirizine and loratadine are considered safest. Avoid high-dose regimens. Always check with your OB-GYN.
When to see a specialist
You don’t need to see a specialist for every case. But you should if:
- Your hives last more than 6 weeks
- You have angioedema without hives
- You’re on an ACE inhibitor and had swelling
- Antihistamines aren’t working after 6 weeks
- You have recurrent swelling in the throat or gut
- You have a family history of unexplained swelling
Specialists will check your C1 inhibitor, C3, and C4 levels if hereditary angioedema is suspected. For most people, no testing is needed-just treatment.
What’s new in 2025
Research is moving fast. Omalizumab is now standard for refractory cases. New biologics like ligelizumab are in trials and may be available soon. The focus is shifting from symptom control to targeting the root immune dysfunction.
Also, the 2025 Beaumont Hospital guidelines now recommend ARBs over ACE inhibitors if you need blood pressure control after angioedema. They’re not perfect, but they’re safer.
The biggest change? Doctors are finally learning not to treat all swelling the same. If it doesn’t itch, don’t give antihistamines. If you’re on lisinopril and your lips swell-stop the drug, don’t reach for Zyrtec.
Bottom line: treat smart, not hard
Urticaria and angioedema are not one-size-fits-all. Acute cases? Stop the trigger, take antihistamines, watch for breathing trouble. Chronic cases? Start with antihistamines, escalate the dose, then consider omalizumab. Angioedema without itching? Stop ACE inhibitors, don’t waste time on steroids.
Most people get better. It just takes patience and the right approach. Don’t let anyone tell you it’s "just hives." Your symptoms matter. And with the right plan, you can get your life back.
Kylie Robson
December 27, 2025 AT 15:15Let's be clear: the first-line treatment for chronic spontaneous urticaria isn't just "high-dose antihistamines"-it's pharmacokinetic optimization of H1-receptor antagonism with titration protocols aligned to BA/BE guidelines. Most clinicians still treat this like a 1990s allergy algorithm, ignoring the 2020 EAACI/GA²LEN consensus that supports up to 4-fold dosing. The real bottleneck isn't efficacy-it's provider education. You can't manage what you don't measure, and we're still measuring IgE when we should be tracking mast cell tryptase kinetics.
Olivia Goolsby
December 28, 2025 AT 19:32Everyone’s ignoring the REAL truth-hives are caused by 5G towers, glyphosate in the water supply, and the CDC’s secret vaccine microchip program that triggers mast cell degranulation. They don’t want you to know that ACE inhibitors are just a cover-up-the real culprit is the fluoride in your toothpaste! They’ve been silencing research since 2017! I’ve got 17 PDFs from anonymous whistleblowers in Big Pharma, and if you Google ‘bradykinin suppression by aluminum hydroxide’ you’ll see the pattern-it’s all connected! They want you dependent on Xolair so they can charge $1,200/month-while your kidneys fail from prednisone! Wake up!!!
Alex Lopez
December 29, 2025 AT 05:00Well. That was... surprisingly accurate. For a moment, I thought I was reading a peer-reviewed review article. Kudos to the author. Now, let’s all take a deep breath and remember: antihistamines are not magic. They’re pharmacological bandaids. And yes, omalizumab is expensive-but so is ER visits for laryngeal edema. Maybe if we stopped calling it "just hives," insurance would cover it. :)
Raushan Richardson
December 30, 2025 AT 13:44YES. This is the info I wish I’d had 3 years ago. I was on prednisone for 6 months because my doctor thought it was "allergic"-turns out I had CSU and was on lisinopril. Stopped it. Swelling faded in 3 weeks. No steroids needed. Thank you for saying it clearly. I finally feel seen. 💪
Robyn Hays
January 1, 2026 AT 10:22I love how you broke this down like a map for confused souls. It’s like someone took the medical jargon jungle and turned it into a trail with signs: "Danger: Bradykinin Ahead" and "Antihistamines: Only for Itchy Paths." I’ve been wandering in circles for years-this feels like the first time someone handed me a flashlight. Thank you for writing this like you care.
Liz Tanner
January 1, 2026 AT 21:28Minor correction: the 2021 AAEM guideline actually says "avoid prolonged corticosteroid use," not "avoid beyond 10 days." The 10-day window is a common clinical approximation, but not a hard cutoff. Also, cetirizine’s half-life is dose-dependent-higher doses may extend duration of action beyond 24 hours. Just precision matters.
Babe Addict
January 3, 2026 AT 18:33Antihistamines don't work because they're designed to treat pollen allergies, not immune dysregulation. The real issue is gut permeability from glyphosate and GMOs. Your mast cells are screaming because your microbiome is dead. Omalizumab? That's just a Band-Aid on a bullet wound. Try fasting, colloidal silver, and grounding. I cured my CSU with a 21-day lemon water cleanse and a crystal bracelet. Science is just religion with lab coats.
Satyakki Bhattacharjee
January 4, 2026 AT 21:01Why do we treat symptoms when the problem is sin? God gave us bodies to endure. Medicine is arrogance. I had hives for 10 years. I prayed. I fasted. I stopped taking pills. Now I am healed. You do not need drugs. You need repentance.
Kishor Raibole
January 6, 2026 AT 20:09One must pause and reflect upon the metaphysical implications of histamine-mediated inflammation in the context of late-stage capitalist pharmacology. The pharmaceutical-industrial complex, through its commodification of immune dysregulation, has engineered a condition of chronic dependency-where the patient becomes a perpetual consumer of biologics, while the true etiology-existential alienation, spiritual dissonance, and the collapse of communal care-is systematically erased. We treat the skin, while the soul screams in silence.
Liz MENDOZA
January 8, 2026 AT 08:42This is so helpful. I’ve been terrified to tell my doctor I’m on lisinopril because I didn’t know it could cause swelling. Now I’m going to ask about switching. Thank you for making me feel less alone. You’re right-it’s not "just hives." It’s my body screaming for help.
Anna Weitz
January 10, 2026 AT 06:02Stop overtreating. Antihistamines are overprescribed. Your immune system isn’t broken-it’s trying to tell you something. Stress. Toxins. Trauma. The body doesn’t lie. You’re not allergic to food-you’re allergic to modern life. Take a walk. Breathe. Stop chasing pills. Let your body heal. The drugs are the problem, not the solution.
Jane Lucas
January 10, 2026 AT 12:36i was on zyrtec for 2 years and nothing happened then i stopped the lisinopril and boom no more swelling. why does no one tell you this??
Elizabeth Alvarez
January 10, 2026 AT 18:06They don't want you to know this, but the real cause of chronic hives is the government's secret weather modification program. They spray aluminum nanoparticles to control population stress levels, and your immune system reacts to it as a foreign invader. That's why antihistamines only mask it-because the trigger is still in the air. They’ve been doing this since the 90s. Check the chemtrail maps. Look at the correlation between hives outbreaks and military flight paths. It’s not coincidence-it’s conspiracy. And omalizumab? That’s just a distraction to keep you from demanding answers.