Myoclonic Seizures: What They Look Like and What to Do
A sudden, shock-like jerk of your arm or a quick twitch while you’re awake can be a myoclonic seizure. They’re often brief but can be confusing and scary. This page gives clear, practical steps for spotting them, what usually causes them, and how to handle the situation right away.
What are myoclonic seizures?
Myoclonic seizures are quick, involuntary muscle jerks. They last a second or two and may affect one limb, both arms, or the whole body. Unlike a tonic-clonic seizure, people usually stay conscious during a myoclonic event. Still, when jerks are frequent or happen in clusters, daily life and safety can be affected.
Some jerks are harmless — think of the tiny twitch you get as you fall asleep. Myoclonic seizures are different because they repeat unexpectedly and can hint at an underlying brain condition or medication effect.
Causes & common triggers
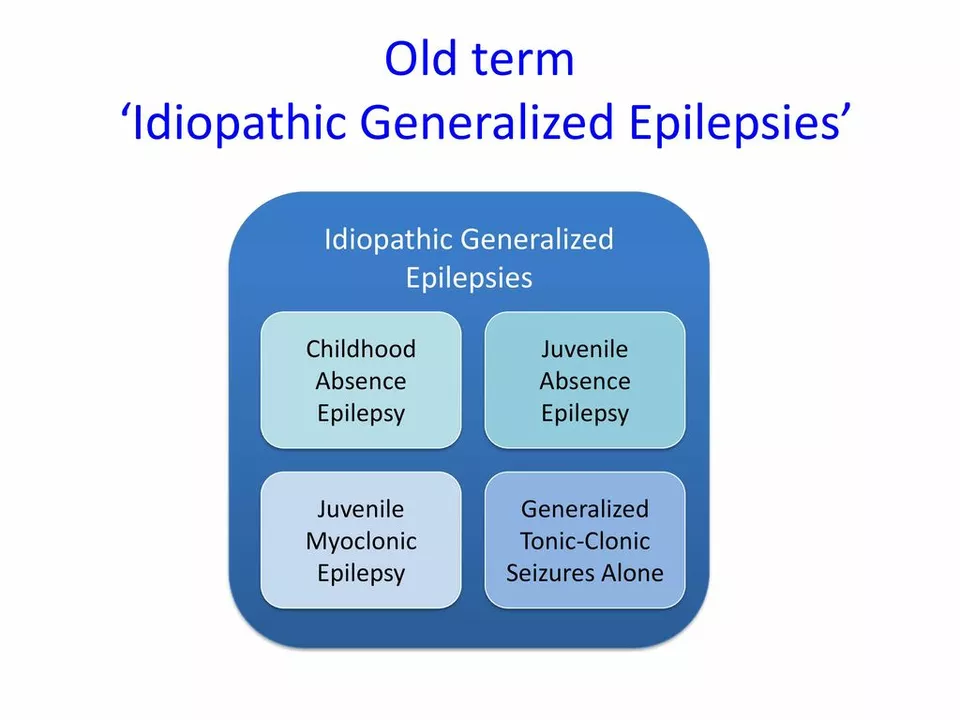
Several things can cause myoclonic seizures. They show up in genetic conditions like juvenile myoclonic epilepsy, during withdrawal from alcohol or sedatives, after a head injury, or with certain infections and metabolic problems. Some medicines can trigger them too.
Common triggers to watch for: lack of sleep, flashing lights, fever, stress, and sudden stopping of medications such as benzodiazepines. If jerks start after a new drug or during withdrawal, tell your doctor right away.
Doctors diagnose myoclonic seizures using your history, a neurological exam, and tests. An EEG (brain wave test) is the main tool; it can catch abnormal patterns that match myoclonus. Blood tests, MRI scans, and sometimes genetic tests help find the cause.
If jerks happen only once or injury is possible, visit urgent care. If jerks are new, getting worse, or come with confusion, weakness, or trouble speaking, head to the emergency room.
What to do and treatment options
During a myoclonic jerk, keep the person safe: move sharp objects away and support them so they don’t fall. Most events end quickly and don’t need CPR. Stay calm and note how long it lasted and what the jerks looked like — that helps the doctor.
Treatment depends on cause. For many people, anti-seizure medications like valproate, levetiracetam, or clonazepam reduce myoclonic jerks. If a medication or substance is the trigger, adjusting that factor often helps. Sleep hygiene, stress control, and avoiding known triggers make a real difference.
Living with myoclonic seizures means tracking patterns and working with your neurologist. Small changes — regular sleep, cutting alcohol, reviewing prescriptions — often lower frequency. For complex or genetic causes, a specialist can map a treatment plan and discuss options like diet changes or newer therapies.
If jerks are troubling or new, don’t ignore them. A quick check by a doctor can find a simple fix or prevent bigger problems.