Azathioprine: What It Is and What You Need to Know
Azathioprine is a common immune-suppressing medicine used to treat autoimmune diseases and prevent organ rejection. It helps calm an overactive immune system so inflammation goes down and organs stop getting attacked. Doctors prescribe it for conditions like Crohn’s disease, ulcerative colitis, rheumatoid arthritis, and after some transplants.
How azathioprine works and common uses
Azathioprine turns into active compounds that reduce how fast immune cells grow. That slows the immune response. People take it when other medicines alone aren’t enough or when long-term control is needed. It’s not a quick fix—benefits often take weeks to months. Typical uses include keeping inflammatory bowel disease in remission and lowering rejection risk after kidney or liver transplant.
Doctors usually start with a low dose and adjust it based on weight, response, and blood tests. Some people need a genetic test for an enzyme called TPMT before starting. Low TPMT activity raises the chance of serious bone marrow suppression, so doses change or the drug is avoided.
Side effects, interactions, and safety tips
Common side effects include nausea, mild liver enzyme rises, and increased risk of infections. Serious but less common problems are low blood counts, pancreatitis, and rare skin cancers or lymphoma after long use. If you get fever, sore throat, unusual bruising, or yellow skin, call your doctor right away.
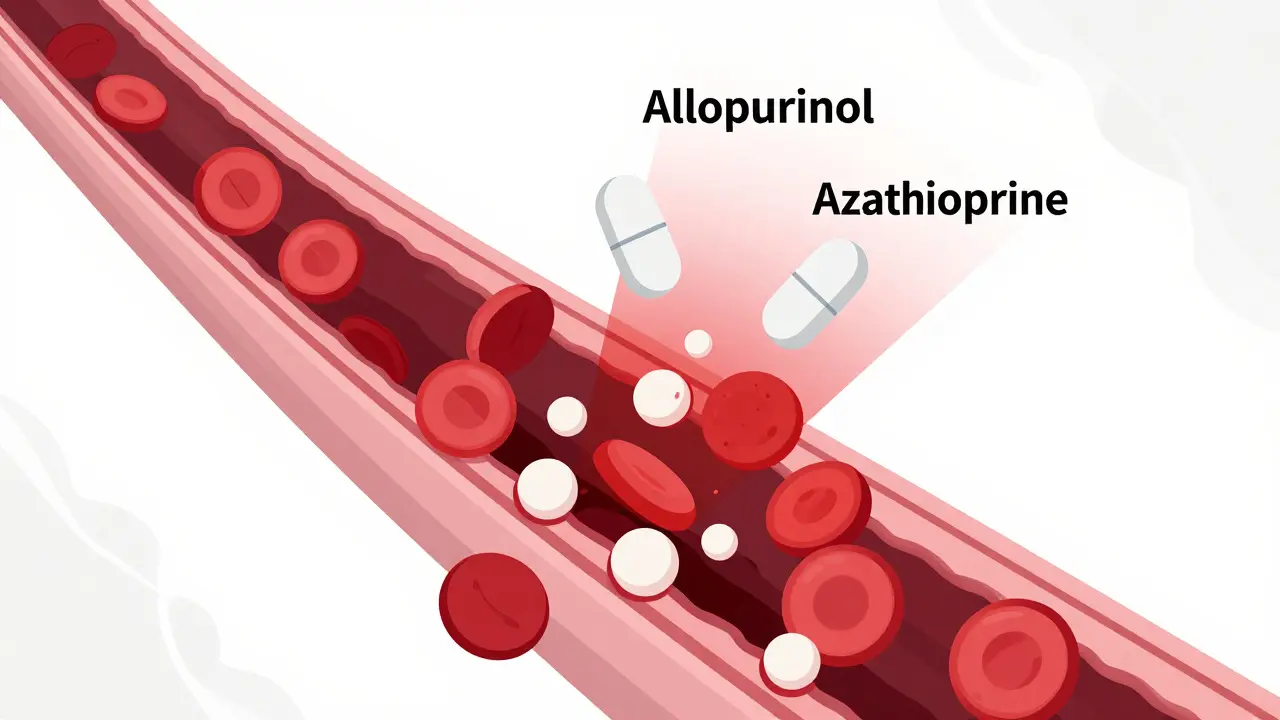
Azathioprine interacts with some drugs. Allopurinol and similar medicines that lower uric acid can greatly increase azathioprine levels; doctors usually lower the dose dramatically or pick another option. Live vaccines should be avoided while immune-suppressed. Tell your provider about all medicines, supplements, and herbs you use—some can change how azathioprine works.
Pregnancy and breastfeeding need special attention. Azathioprine is sometimes used in pregnancy when benefits outweigh risks, but this must be managed by a specialist. Don’t stop or change your dose without talking to the prescriber.
Practical tips: get baseline blood tests and repeat them regularly—often every 1–3 months at first, then less often if stable. Protect your skin from sun and get regular skin checks. Carry a note or card saying you take azathioprine in case of emergency. If you plan travel, check vaccine rules and infection risks where you’re going.
Want to learn more or find trusted articles and buying guides? Visit Medstore-365.com for plain-language guides on drugs, safety tips, and how to talk with your doctor. Always check with your health provider before making changes to medicines.
Quick checklist for visits: bring a current medicine list, note any infections or unusual bruising, ask for TPMT testing if you haven’t had it, confirm blood test schedule, and ask whether your vaccines are up to date. If you use herbal remedies like St. John’s wort or high-dose vitamin C, mention them. If switching from or to allopurinol, get a clear plan. If side effects feel severe, go to urgent care. Small steps like this make treatment safer and easier to manage. Questions? Talk with your pharmacist or specialist for personalised advice today.