SSRI Antidepressants and Serotonin Syndrome Risk from Drug Interactions
 Jan, 7 2026
Jan, 7 2026
When you're taking an SSRI antidepressant like sertraline or escitalopram, you might think the biggest risk is side effects like nausea or sleep changes. But the real danger often comes from what you're combining it with - not the drug itself. Serotonin syndrome isn't rare. It's underdiagnosed, misunderstood, and sometimes deadly. And it's happening more often because people are taking more medications than ever before.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome isn't just feeling a little off. It's a medical emergency caused by too much serotonin building up in your brain and nervous system. Think of serotonin like a chemical messenger. SSRIs stop your brain from reabsorbing it, so more stays around. That's how they help with depression. But when you add another drug that also boosts serotonin - even something you think is harmless - you can flood the system.The symptoms don't sneak up slowly. They hit fast. You might start shivering without being cold. Your muscles go stiff. You sweat like you've run a marathon in the heat. Your heart races. Your temperature spikes above 38°C. Then come the involuntary muscle twitches - clonus - where your leg or foot jerks uncontrollably. In severe cases, confusion, seizures, or even coma can follow.
The Hunter Criteria are what doctors use to diagnose this. You don’t need every symptom. Just one clear sign - like spontaneous clonus - plus another like agitation or high fever - is enough to trigger urgent treatment. And it’s not just theoretical. Between 2018 and 2022, over 1,800 cases were reported to the FDA’s adverse event system. Most involved combinations of SSRIs with other drugs.
High-Risk Drug Combinations You Need to Know
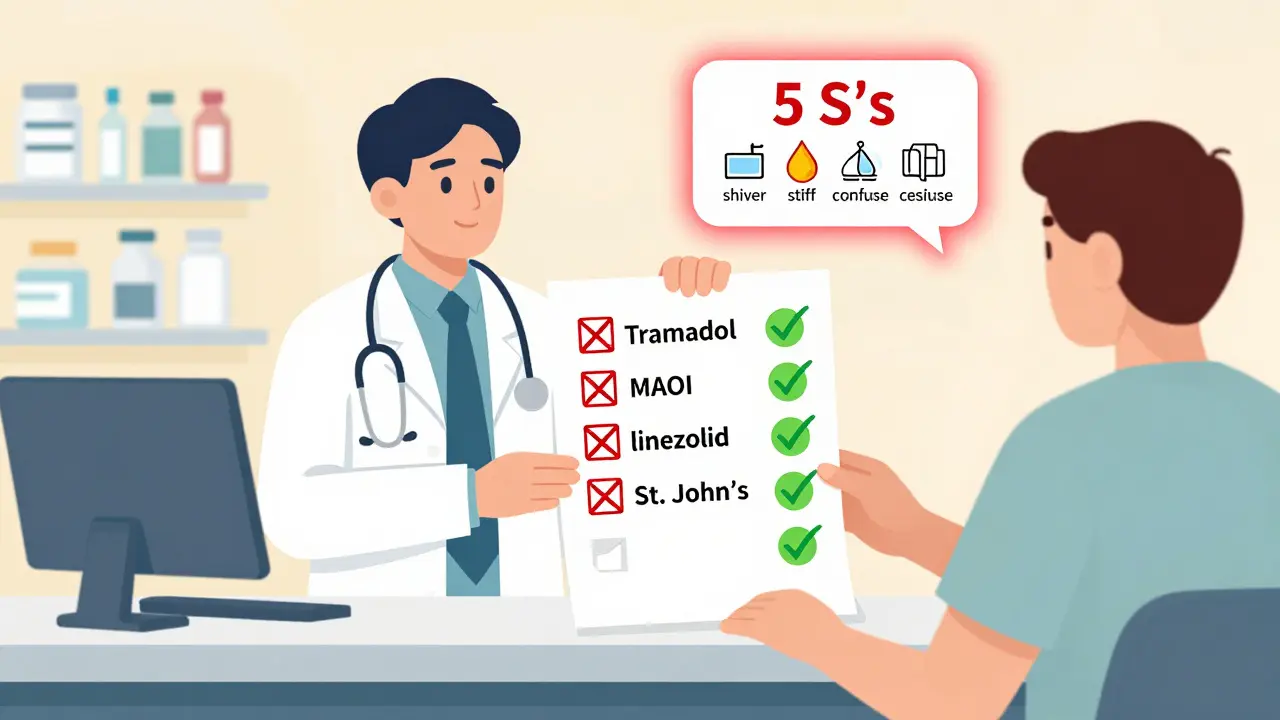
Not all drug interactions are created equal. Some are minor. Others are ticking time bombs.MAOIs are the worst. Monoamine oxidase inhibitors like phenelzine or selegiline are rarely used today, but if you're on one - and you take an SSRI - your risk of death jumps dramatically. Studies show 30% to 50% of people who mix these two can die. That’s why doctors require a full 2-week gap - sometimes 5 weeks if you’ve been on fluoxetine - before switching between them. Fluoxetine sticks around in your body for weeks. You can’t just stop one and start the other.
Tramadol, dextromethorphan, and pethidine are high-risk opioids. These aren’t your typical painkillers. Tramadol, often prescribed for chronic back pain, acts like an SSRI on top of being a pain reliever. Dextromethorphan is in many cough syrups. Pethidine is used in hospitals. All three dramatically increase serotonin levels. A 2023 study found combining SSRIs with tramadol raises serotonin syndrome risk by nearly 5 times. One Reddit user described being hospitalized after taking tramadol with sertraline - his temperature hit 104.2°F. That’s not an exaggeration. That’s a real case.
SNRIs like venlafaxine or duloxetine are also dangerous. These work similarly to SSRIs but affect both serotonin and norepinephrine. Mixing them with an SSRI triples your risk. Many patients don’t realize they’re on two serotonergic drugs at once. One doctor told me about a patient who was prescribed sertraline for anxiety, then later got venlafaxine for depression. No one checked the interaction. Within days, the patient had muscle rigidity and confusion.
Linezolid, an antibiotic, is a hidden threat. It’s used for stubborn infections like MRSA. It’s not an antidepressant. But it blocks serotonin breakdown like an MAOI. A 2022 study found patients over 65 on linezolid with SSRIs had nearly 3 times the risk of serotonin syndrome. Most doctors don’t think to ask about antidepressants when prescribing antibiotics. That’s a gap.
Herbal supplements like St. John’s wort are risky too. People think natural = safe. But St. John’s wort is a potent serotonin booster. Multiple patients on Drugs.com reported shivering, confusion, and hospital visits after mixing it with Prozac or Zoloft. It’s not regulated like prescription drugs. No one warns you.
Why This Is Getting Worse
The problem isn’t just bad choices. It’s the system.More than 22% of Americans over 65 take five or more medications daily. Many are on SSRIs for depression or anxiety, and also on painkillers for arthritis or back pain. Doctors see them for one issue at a time - depression, then pain, then insomnia - and prescribe without seeing the full picture. Pharmacists are the last line of defense. A 2023 study showed pharmacist-led reviews cut serotonin syndrome risks by 47% in Medicare patients. But not everyone has access to that.
Electronic health records are getting better. Epic Systems reduced dangerous SSRI-opioid prescriptions by 32% in 200 U.S. hospitals after adding alerts. But not all systems are updated. And many older patients still get prescriptions on paper.
And then there’s the cost of ignoring this. The average hospital stay for serotonin syndrome costs nearly $29,000. About 1,200 to 1,500 people in the U.S. are hospitalized each year because of this. Most of those cases were preventable.
What You Should Do
If you’re on an SSRI, here’s what you need to do right now:- Make a full list of everything you take. Include prescriptions, over-the-counter meds, supplements, and herbal products. Don’t leave anything out.
- Bring it to every doctor visit. Even if it’s just for a cold. Ask: “Could any of these interact with my antidepressant?”
- Know the red flags. The Cleveland Clinic calls them the “5 S’s”: Shivering, Sweating, Stiffness, Seizures (rare), and Sudden confusion. If you notice even two of these after starting a new drug, get help immediately.
- Don’t start anything new without checking. That includes cough syrup, pain relievers, or sleep aids. Even melatonin can interact in rare cases.
- Ask about alternatives. If you need pain relief, ask if morphine or oxycodone is safer than tramadol. If you have a cough, ask for something without dextromethorphan.
Pharmacists can run interaction checks in seconds. Use them. If your pharmacy doesn’t offer counseling, go to a different one. Your life depends on it.
What Doctors Should Be Doing
Doctors need to stop prescribing in silos. The American Psychiatric Association and the International Consortium for Serotonin Toxicity agree: avoid SSRIs with MAOIs, linezolid, and methylene blue - period. For opioids, avoid tramadol, pethidine, and dextromethorphan entirely if possible. If you must use them, monitor closely. Reduce the dose. Check in after 48 hours.And stop assuming patients know what they’re taking. Many elderly patients take pills from multiple pharmacies. They don’t know the names. They just know what color the pill is. That’s a recipe for disaster.
Electronic prescribing systems need mandatory alerts. The FDA is pushing for this in 2024. But until then, it’s up to you and your doctor to be the safety net.

Real Stories, Real Consequences
The Libby Zion case in 1984 changed medicine forever. An 18-year-old died after being given meperidine (a strong opioid) while on phenelzine (an MAOI). Her death exposed how poorly supervised residents were, and how little doctors knew about drug interactions. It led to rules limiting resident work hours - but it didn’t fix the drug interaction problem.Today, people still die from the same mistake. A 72-year-old woman in Ohio was prescribed sertraline for depression and tramadol for arthritis. Two weeks later, she was found unresponsive. Her temperature was 40.1°C. She had clonus. She didn’t survive. The autopsy confirmed serotonin syndrome.
These aren’t outliers. They’re predictable. And they’re preventable.
What’s Coming Next
Science is catching up. Researchers at UCSF found people with a specific gene variant (CYP2D6 poor metabolizers) are 2.4 times more likely to develop serotonin syndrome when taking tramadol with SSRIs. Genetic testing might soon be part of routine screening.And in 2026, a blood test called SerotoninQuant may become available. Right now, doctors diagnose serotonin syndrome by symptoms - which can look like infections, heatstroke, or neurological disorders. A blood test that measures serotonin levels could make diagnosis faster and more accurate.
But until then, the safest approach hasn’t changed: know what you’re taking. Ask questions. Don’t assume. And never mix an SSRI with another serotonergic drug without professional guidance.
Can you get serotonin syndrome from just one SSRI?
Rarely. Serotonin syndrome almost always happens when SSRIs are combined with another drug that increases serotonin - like an SNRI, opioid, or herbal supplement. Taking an SSRI alone at a normal dose is very unlikely to cause it. Overdose is a different story, but even then, it’s uncommon compared to combinations.
How long does it take for serotonin syndrome to develop after a drug interaction?
Usually within hours. Most cases start within 2 to 6 hours after taking a new drug. But with long-acting SSRIs like fluoxetine, symptoms can appear up to 5 days later if you start another serotonergic agent. Don’t wait to see if symptoms go away. If you feel something’s wrong, seek help immediately.
Is it safe to take ibuprofen or acetaminophen with an SSRI?
Yes. Ibuprofen and acetaminophen are not serotonergic. They don’t raise serotonin levels. These are generally safe to take with SSRIs for pain or fever. But avoid combination cold medicines that contain dextromethorphan or other hidden serotonergic ingredients.
What should I do if I think I have serotonin syndrome?
Stop taking all non-essential medications immediately. Call emergency services or go to the nearest ER. Do not wait. Serotonin syndrome can worsen quickly. Treatment involves stopping the triggering drugs, giving IV fluids, cooling the body, and sometimes using benzodiazepines or cyproheptadine. Early treatment saves lives.
Can I restart an SSRI after having serotonin syndrome?
Yes - but only after a full recovery and with extreme caution. Your doctor will likely avoid the same drug or any that caused the reaction. They may choose a different class of antidepressant, like bupropion, which doesn’t affect serotonin. Never restart an SSRI without medical supervision.
Are there any SSRIs that are safer than others?
All SSRIs carry some risk when combined with other serotonergic drugs. But fluoxetine has the longest half-life, meaning it stays in your system longer - so the washout period before switching is longer. Paroxetine is the most potent serotonin reuptake blocker, so it may pose slightly higher risk in combinations. Sertraline and escitalopram are often preferred because they’re effective and have fewer drug interactions overall - but they’re not risk-free.
christy lianto
January 8, 2026 AT 20:04I’ve seen this happen to my cousin-she took tramadol for her back pain and sertraline for anxiety, and within 36 hours she was in the ER sweating bullets, shaking like she had Parkinson’s, and screaming that the walls were breathing. No one warned her. No one asked about her meds. She’s fine now, but she won’t touch anything without checking with her pharmacist first. This isn’t hype-it’s a silent killer.
Ken Porter
January 9, 2026 AT 07:14Why are we letting unregulated supplements like St. John’s wort be sold like candy? If this was a prescription drug, the FDA would’ve shut it down years ago. Wake up, America.
swati Thounaojam
January 10, 2026 AT 01:18in india, people just buy pills from local shops without knowing anything. i saw a man take fluoxetine with dextromethorphan cough syrup and passed out in the bus. no one knew why.
Molly Silvernale
January 10, 2026 AT 19:25It’s not just about drugs-it’s about how we’ve outsourced our health to a system that treats symptoms like inventory, not people. We’re drowning in pills, but starved for context. Who’s checking the whole picture? Not the doctor who sees you for 7 minutes. Not the pharmacist who’s rushing to the next customer. Not the algorithm that flags ‘possible interaction’ but doesn’t scream ‘THIS WILL KILL YOU.’ We’ve turned medicine into a spreadsheet-and now we’re surprised when the numbers turn red?
Serotonin syndrome isn’t a glitch. It’s a moral failure. It’s the cost of convenience. Of ‘just one more pill.’ Of believing that if it’s legal, it’s safe. If it’s natural, it’s harmless. If it’s prescribed, it’s understood. But the body doesn’t care about prescriptions. It doesn’t care about labels. It just reacts. And when you flood it with serotonin, it doesn’t whisper-it screams. And too many of us are too busy to hear it.
Maybe we need a new word. Not ‘side effect.’ Not ‘interaction.’ Maybe we need ‘body betrayal.’ Because that’s what it feels like when the thing meant to heal you becomes the thing that kills you. And no one saw it coming.
Luke Crump
January 11, 2026 AT 19:27So… you’re saying SSRIs are basically chemical landmines? That every person on them is one cough syrup away from a coma? What’s next? Are we gonna ban happiness? Maybe we should just let people die from depression instead of letting them die from antidepressants. Either way, someone’s gonna lose. I call it the serotonin paradox.
Annette Robinson
January 11, 2026 AT 19:29Thank you for writing this. I’m a nurse, and I’ve seen too many patients come in confused, overheated, trembling-no one connecting the dots. I always ask about supplements. Always. Even if the patient says ‘I don’t take anything.’ I say, ‘Even the little green pill from the health food store?’ Half the time, they say yes. And then we catch it before it turns dangerous. You’re right-pharmacists are the unsung heroes here. If your pharmacy doesn’t offer med reviews, find one that does. Your life matters more than the extra $5.
Donny Airlangga
January 13, 2026 AT 04:45I was on sertraline for years, then got prescribed venlafaxine for ‘better results.’ No one told me it was a double serotonin hit. I got muscle stiffness, blurred vision, and felt like my brain was boiling. I went to the ER and the doctor said, ‘Oh, you’re on both?’ Like it was normal. I’ve been scared to take anything since. This needs to be standard education, not a lucky accident.
Kristina Felixita
January 15, 2026 AT 04:05my abuela took st. john’s wort with her zoloft because her friend said it ‘cleanses the soul’-she ended up in the hospital with fever and wild eyes. we didn’t know what was happening. now she only takes her meds with me beside her. no more ‘natural’ shortcuts. love means asking questions, even when it’s awkward.
Dave Old-Wolf
January 15, 2026 AT 10:28So if I’m on an SSRI and I need pain relief, what’s actually safe? Ibuprofen? Tylenol? What about gabapentin? CBD? I’ve been too scared to ask my doctor because I don’t want to sound like a hypochondriac.