Shingles: Effective Antiviral Treatment and Pain Management Strategies
 Dec, 25 2025
Dec, 25 2025
Shingles isn’t just a rash. It’s a sharp, burning pain that can turn everyday life into a nightmare - especially if you’re over 50. The virus behind it, varicella-zoster, has been hiding in your nerves since you had chickenpox as a kid. And when it wakes up, it doesn’t knock. It attacks.
Why Timing Matters More Than Anything
If you feel tingling, burning, or itching on one side of your body - maybe along your ribs, forehead, or waist - and then see red bumps forming, don’t wait. The clock starts ticking the moment the rash appears. You have 72 hours to start antiviral medication, and every hour counts.
Studies show that starting treatment within the first 48 hours can cut the length of the outbreak by nearly half. People who waited longer often ended up with pain that lasted months, even years. That’s not just discomfort - it’s chronic nerve damage called post-herpetic neuralgia (PHN). About 1 in 5 people over 60 get it. For some, the pain never fully goes away.
Three antivirals are approved for shingles: valacyclovir, acyclovir, and famciclovir. Of the three, valacyclovir is the most commonly prescribed because it’s easier to take. You only need three pills a day for seven days. Acyclovir? You’d need five doses daily - a lot harder to stick to when you’re already in pain.
Here’s what the numbers say: Valacyclovir at 1,000 mg three times a day reduces acute pain by about 30% compared to no treatment. It also heals blisters 2-3 days faster. Famciclovir and acyclovir do similar things, but valacyclovir has the edge in pain control. One 2023 study from NYU found that patients on valacyclovir used 22-25% less gabapentin or pregabalin - drugs that cause dizziness, especially in older adults.
What Happens If You Miss the Window?
Some people delay because they think it’s just a bug or a rash. Others don’t have easy access to a doctor. But if it’s been more than 72 hours? Antivirals still help - just not as much. They won’t reverse nerve damage, but they can still reduce the spread of the virus and lower the risk of complications like skin infections or eye damage.
That’s especially true if you have shingles near your eye. The Zoster Eye Disease Study (ZEDS), which tracked patients for over a year, found that long-term low-dose valacyclovir (500 mg daily) cut new or worsening eye problems by 26%. It also reduced flare-ups by nearly a third. For people with shingles in the eye, this isn’t optional - it’s life-changing. Without it, you could lose vision.
Pain Management: It’s Not Just About Pills
Antivirals tackle the virus. But they don’t fix the pain. That’s where you need a layered approach.
For nerve pain, doctors often start with gabapentin or pregabalin. These are anticonvulsants, not painkillers. They calm overactive nerves. Typical doses start at 300 mg once a day and can go up to 3,600 mg daily - but it takes weeks to build up. Side effects? Drowsiness, dizziness, swelling. Older adults often struggle with these.
Amitriptyline, a tricyclic antidepressant, is another go-to. You take it at night, even if you’re not depressed. It helps rewire how nerves send pain signals. Doses are low - 25 to 75 mg - and it can take two to four weeks to work. Many patients report better sleep and less burning pain after a month.
Topical treatments are underrated. Lidocaine patches (5%) go on for 12 hours, off for 12. They numb the area without affecting your whole body. Capsaicin cream (0.075%) burns at first - yes, really - but after a few days, it depletes the pain chemical in nerves. Use it four times a day. It’s messy, but it works for many.
Don’t rely on opioids. They’re not good for nerve pain. They might help for a few days if the pain is unbearable, but they don’t fix the root problem. And they come with risks - addiction, constipation, breathing issues. Dermatology experts warn against long-term use.

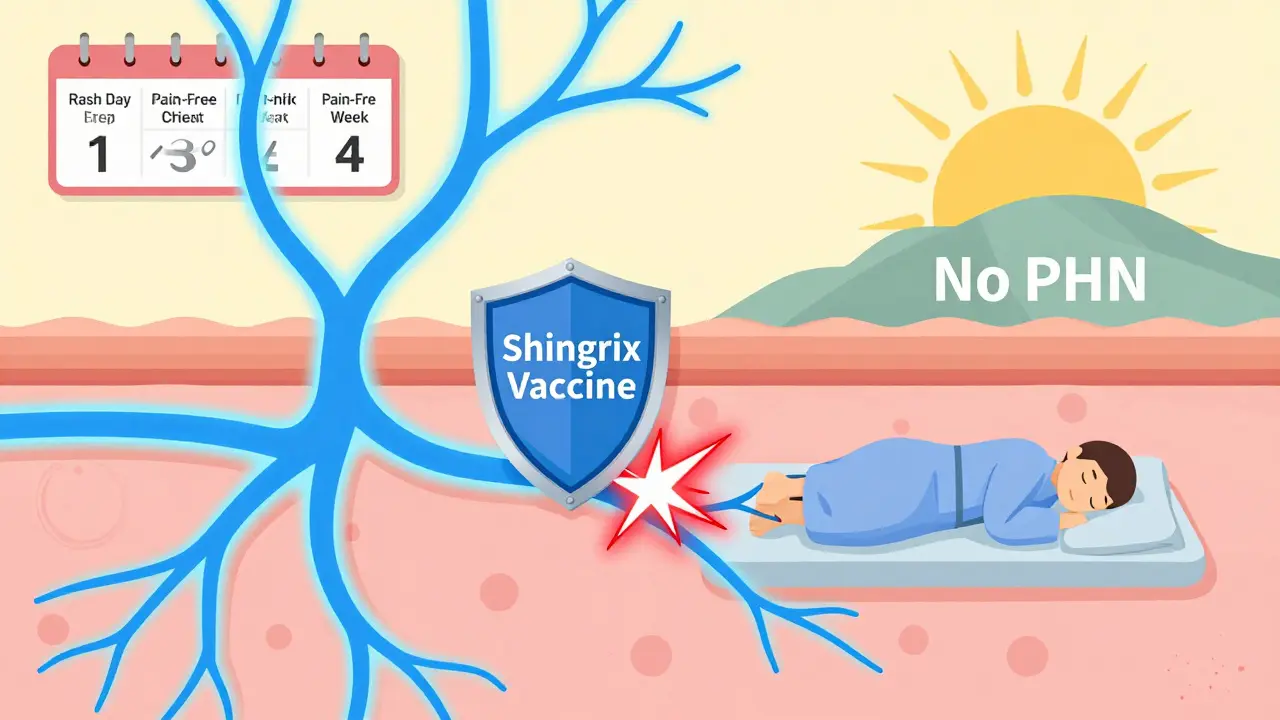
The Vaccine That Changes Everything
The best treatment for shingles? Not taking it at all.
The Shingrix vaccine is over 90% effective at preventing shingles. It’s two shots, given 2 to 6 months apart. Even if you’ve had shingles before, you still need it. The vaccine cuts your risk of PHN by more than 85%. It’s recommended for everyone 50 and older, even if you got the old Zostavax vaccine years ago.
Side effects? Sore arm, fatigue, muscle aches. Some people feel like they’ve been hit by a truck for a day or two. But that’s nothing compared to weeks of burning pain. And if you’re immunocompromised - from cancer treatment, HIV, or steroids - Shingrix is even more critical.
When Antivirals Aren’t Enough: The Controversial Add-On
Some doctors add steroids - like prednisone - to antiviral treatment. The idea? Reduce inflammation fast. A few small studies show it might cut acute pain by another 20-30%. But it’s not standard. Why? Because steroids weaken your immune system. If your body can’t fight the virus, the rash might spread. Or you could get a secondary infection.
The Mayo Clinic doesn’t recommend it routinely. But for severe cases - especially in younger patients with intense pain - some specialists still use it short-term (40-60 mg for 1-2 weeks, then slowly tapered). It’s a gamble. Only a doctor should decide.
What Patients Really Say
On forums like Reddit’s r/chronicpain, people who started antivirals within 48 hours reported being back to normal in 10-14 days. Those who waited? Some were still in pain after three months. One woman in her 60s said she didn’t realize the tingling in her chest was shingles until the blisters showed up. By then, it was too late. She developed PHN. Now she uses lidocaine patches every day.
Another survey of 1,200 people on PatientsLikeMe showed 62% believed early antivirals stopped their pain from becoming chronic. But 38% still got PHN - even with treatment. That’s the harsh truth: antivirals help, but they’re not magic.
Cost, Access, and Real-World Barriers
A seven-day course of valacyclovir costs $85-$150 without insurance. With Medicare or private plans, it’s often under $20. But many people don’t fill the prescription because they don’t know it’s urgent. Or they can’t get an appointment fast enough.
One study found early treatment saves $487 per person by avoiding ER visits, hospital stays, and long-term pain meds. That’s money saved for the system - and for you.
And yet, in rural areas or places with limited specialists, people wait days to see a doctor. That’s why awareness matters. If you’re over 50 and feel unusual pain on one side of your body - don’t wait. Call your doctor. Go to urgent care. Say: “I think it might be shingles.”
What You Can Do Right Now
If you’re at risk - over 50, or immunocompromised - get vaccinated. If you haven’t had Shingrix, schedule it. It’s safe, effective, and your best defense.
If you think you have shingles:
- Look for a one-sided rash or burning pain - not both sides.
- Check for fluid-filled blisters forming in a band or stripe.
- Call your doctor immediately. Don’t wait for the rash to get worse.
- Ask for valacyclovir 1,000 mg three times a day for 7 days.
- Start gabapentin or amitriptyline if the pain is severe.
- Use lidocaine patches or capsaicin cream for local relief.
- Keep the area clean and dry. Avoid scratching.
Shingles doesn’t care if you’re busy, tired, or scared. It moves fast. But you can move faster - if you know what to do.
Can shingles go away without antivirals?
Yes, shingles can resolve on its own in 3 to 5 weeks. But without antivirals, the pain is likely to be worse, the rash may spread further, and your risk of long-term nerve pain (post-herpetic neuralgia) increases significantly - especially if you’re over 60. Antivirals don’t cure shingles, but they make it much more manageable.
Is shingles contagious?
Shingles itself isn’t contagious. But the virus inside the blisters - varicella-zoster - can spread to someone who’s never had chickenpox or the chickenpox vaccine. If they get infected, they’ll develop chickenpox, not shingles. Cover the rash, avoid touching it, and don’t be around pregnant women, newborns, or people with weak immune systems until the blisters scab over.
Can I get shingles more than once?
Yes, although it’s uncommon. About 1 in 3 people get shingles once in their lifetime, and around 1 in 25 of those will have it again. The risk goes up if you’re older, stressed, or have a weakened immune system. That’s why the Shingrix vaccine is recommended even after you’ve had shingles - it reduces the chance of recurrence.
Do antivirals prevent post-herpetic neuralgia (PHN)?
Evidence is mixed. Some studies show early antiviral treatment lowers PHN risk by 20-30%. Others, like the Cochrane review, say acyclovir doesn’t significantly reduce PHN at 6 months. But most doctors still recommend starting antivirals within 72 hours - because even if they don’t fully prevent PHN, they reduce the severity and duration of the initial pain, which may lower the chance of nerves becoming permanently damaged.
Why is valacyclovir preferred over acyclovir?
Valacyclovir is a prodrug that turns into acyclovir in the body - but it’s absorbed better. That means you take it fewer times per day: three times instead of five. This improves compliance, especially for older adults. Studies also suggest it reduces acute pain slightly more than acyclovir. While both work, valacyclovir is easier to use and just as safe.
Can I use over-the-counter pain relievers for shingles?
Yes, for mild pain. Ibuprofen or acetaminophen can help with fever and general discomfort. But they won’t touch the nerve pain - that’s the burning, shooting, electric kind. For that, you need prescription meds like gabapentin or amitriptyline. OTC painkillers are fine as a short-term help, but don’t rely on them alone.
Is it safe to take antivirals if I’m on other medications?
Generally yes, but interactions matter. Valacyclovir can affect kidney function, especially with NSAIDs or certain blood pressure drugs. If you’re on immunosuppressants, chemotherapy, or have kidney disease, tell your doctor. They may adjust the dose. Never start antivirals without checking with a healthcare provider if you’re on multiple medications.
How long does shingles pain last after the rash is gone?
For most people, pain fades within a few weeks after the rash clears. But for 10-18% of patients - and up to 30% of those over 60 - pain lasts longer than 90 days. That’s called post-herpetic neuralgia. It can persist for months or years. Early antiviral treatment and proper pain management reduce the odds, but not everyone avoids it. Long-term nerve pain is the biggest complication of shingles.
Can stress trigger shingles?
Yes. Stress doesn’t cause the virus, but it can weaken your immune system enough to let the dormant virus reactivate. People under long-term stress - from caregiving, job loss, or illness - are more likely to get shingles. That’s why it often appears after major life events. Managing stress won’t cure shingles, but it helps your body fight it better.
Should I stay home if I have shingles?
If your rash is covered and you’re not around high-risk people (pregnant women, newborns, unvaccinated children, immunocompromised individuals), you can return to work or daily activities. But if the rash is open and weeping, stay home until it crusts over. Also, if you’re in extreme pain or dizzy from meds, rest. Shingles is exhausting. Listen to your body.
roger dalomba
December 26, 2025 AT 23:45Brittany Fuhs
December 28, 2025 AT 21:49Sophia Daniels
December 29, 2025 AT 09:52Nikki Brown
December 30, 2025 AT 22:08Peter sullen
December 31, 2025 AT 22:46Steven Destiny
January 2, 2026 AT 17:27Fabio Raphael
January 4, 2026 AT 01:09Amy Lesleighter (Wales)
January 5, 2026 AT 21:01Natasha Sandra
January 6, 2026 AT 03:34Erwin Asilom
January 6, 2026 AT 22:36Sumler Luu
January 8, 2026 AT 20:58