Satisfaction Measurement: Are Patients Really Happy With Generic Medications?
 Feb, 9 2026
Feb, 9 2026
When you pick up a prescription, do you ever check if it’s the brand name or the generic? For most people, it doesn’t matter - as long as it works. But for others, the difference between a pill labeled "Lisinopril" and one labeled "Prinivil" can feel huge. And that feeling? It’s not just in their head. It’s measurable. It’s real. And it’s affecting whether they take their medicine at all.
Generic drugs are not second-rate. They contain the same active ingredients, work the same way, and are held to the same safety standards as brand-name drugs. The FDA requires them to be bioequivalent - meaning they deliver the same amount of medicine into the bloodstream within the same timeframe. In theory, there should be no difference. But in practice? Patients often report otherwise. And that gap between science and perception is where satisfaction measurement comes in.
What Exactly Are We Measuring?
Patient satisfaction with generics isn’t about whether the drug cures a disease. It’s about whether the patient feels it works. Researchers have built tools to capture this, like the Generic Drug Satisfaction Questionnaire (GDSQ) is a 12-item survey that measures effectiveness, convenience, and side effects. It’s not fancy. It asks simple things: "Did the medication work as well as you expected?" "Did you notice any new side effects?" "Did the pill look different from what you were used to?"
These questions matter because they predict behavior. A 2021 study in Sage Publications found that effectiveness and convenience together explained 66.8% of why patients felt satisfied or dissatisfied with their generics. That’s huge. It means if a patient thinks the generic doesn’t work as well - even if it does - they’re far more likely to skip doses, stop taking it, or switch back to the brand name. And that costs the U.S. healthcare system about $300 billion a year in avoidable hospital visits and complications.
Why Do People Think Generics Don’t Work?
Let’s be honest: the packaging is different. The shape, color, and even the little imprint on the pill can change every time you refill. One patient told Reddit: "I switched from brand-name Synthroid to generic levothyroxine and my TSH levels became erratic." Another said: "Generic lisinopril works exactly the same as Prinivil but costs $4 instead of $40."
These aren’t contradictions. They’re both true. The science says they’re equivalent. The patient’s experience says otherwise. Why? Because the brain doesn’t process medicine like a lab. It processes it like a story. And if the pill looks different, or if you heard a friend say "I felt worse on the generic," your brain starts to believe it’s not the same.
Studies show this isn’t random. Patients are 2.5 times more likely to report side effects on generics when they know they’ve switched. That’s called the nocebo effect - the opposite of placebo. If you expect to feel bad, you will. And in some cases, it’s not just perception. A 2024 Nature Communications study found 18.2% of patients who switched from brand-name aspirin to generic reported new stomach upset. Was it the drug? Or the change in inactive ingredients? We don’t fully know. But it’s enough to make people hesitate.
Which Medications Cause the Most Doubt?
Not all generics are created equal in the eyes of patients. Antibiotics? Most people don’t care. If it clears up the infection, it’s fine. Satisfaction rates? 85.3%. But for drugs where small changes can have big consequences? The numbers drop hard.
- Antiepileptics: Only 68.9% satisfaction. Patients fear even a 5% difference in blood levels could trigger a seizure.
- Antidepressants: 32.1% of negative online comments mention generics. People report mood swings, fatigue, or emotional numbness - even when labs show no change in drug levels.
- Thyroid meds: Levothyroxine is one of the most switched generics. Yet 15% of users report feeling worse after switching. That’s why some doctors still prescribe the brand name - not because it’s better, but because the patient believes it is.
These aren’t just anecdotes. They’re patterns. And they’re why the FDA launched its Generic Drug User Fee Amendments (GDUFA) III Patient Perception Initiative a $15.7 million effort to build better tools for measuring patient perception of generics in 2024.
Who’s More Likely to Accept Generics?
It’s not just about the drug. It’s about the person.
According to a 2024 Frontiers study in Greece:
- Patients over 60 had 71.4% safety acceptance - higher than younger adults.
- Employed patients showed 82.1% safety acceptance - likely because they’re used to making decisions about cost and value.
- Those who received counseling from their doctor or pharmacist? Satisfaction jumped 34.2%.
That last one is critical. A 2023 PLOS ONE study in Saudi Arabia found that when doctors explained the FDA’s bioequivalence standards - "It’s the same medicine, just cheaper" - patient satisfaction soared. Not because the drug changed. But because the story changed.
Doctors and pharmacists are the bridge between science and belief. If they don’t say anything, patients assume the worst. If they say, "This is exactly the same as your old pill, just without the fancy label," trust goes up.
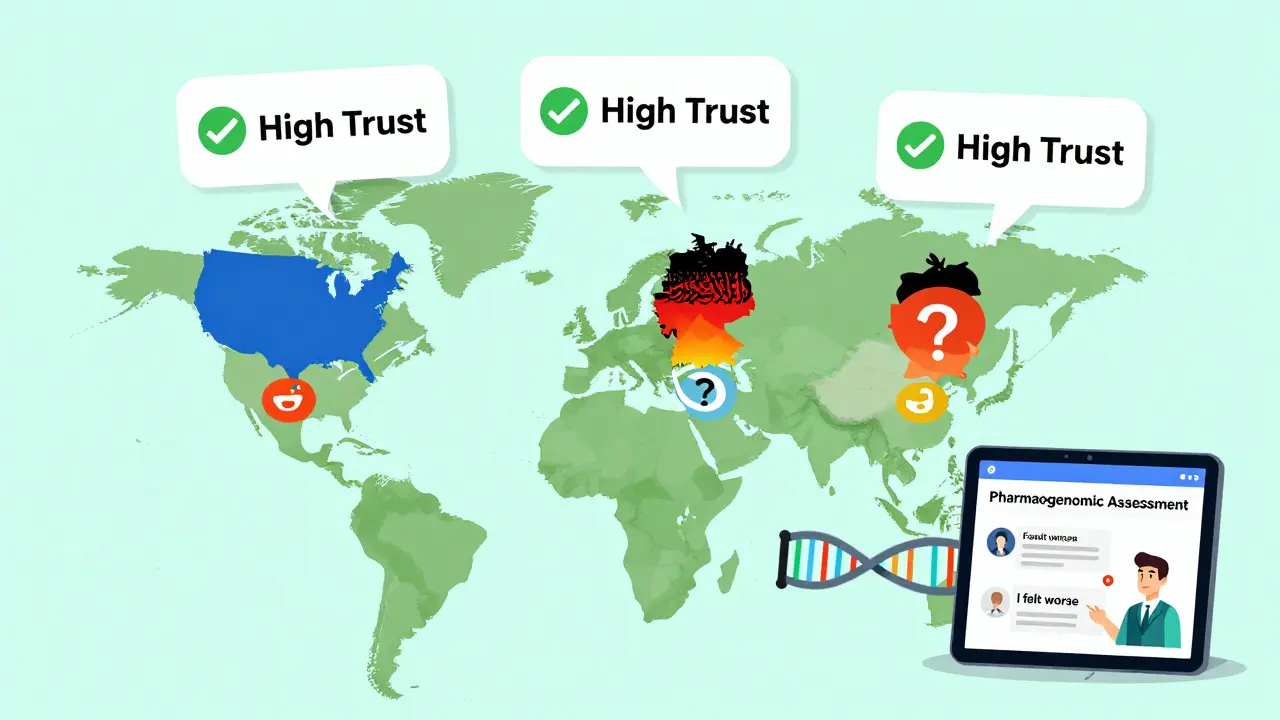
Global Differences in Perception
It’s not just about the patient. It’s about the culture.
A 2020 Journal of Cross-Cultural Psychology study found satisfaction scores were 32% higher in collectivist cultures (like Japan or Saudi Arabia) than in individualist ones (like the U.S. or Germany). Why? In collectivist societies, people trust authority figures - doctors, pharmacists, regulators - more. In individualist cultures, people dig deeper. They Google. They read Reddit. They compare reviews.
And then there’s regulation. The European Medicines Agency requires stricter testing for complex generics than the FDA. That’s why European patients report 12.4% higher satisfaction with generics like insulin or biologics. They’ve been tested harder. They’ve been proven more. And patients notice.
What’s Changing Now?
Researchers aren’t just asking patients to fill out surveys anymore. They’re using AI.
The European Commission is analyzing 500,000 social media posts across 28 languages to find patterns in how people talk about generics. Are they angry? Confused? Grateful? The language matters. Words like "I felt worse" or "It didn’t work" show up more often than "I saved money."
Meanwhile, the Mayo Clinic is testing something even more advanced: pharmacogenomic-informed satisfaction assessments personalized tools that use a patient’s DNA to predict how they’ll respond to a generic drug. Early results? 28.7% more accurate than traditional methods. Imagine a future where your doctor says, "Based on your genes, you’re more likely to notice a difference with this generic. Let’s stick with the brand." Or, "Your body handles generics perfectly. We can switch you and save you $200 a month."
This isn’t sci-fi. It’s happening now.
What Should Patients Do?
If you’re on a generic and feel fine? Keep taking it. The science is clear: it’s just as safe and effective.
If you feel worse after switching? Talk to your doctor. Don’t assume it’s "all in your head." Ask: Could it be the inactive ingredients? Is there a different generic version available? Could we try the brand for a month to compare?
And if you’re a caregiver, pharmacist, or provider? Don’t assume patients know the facts. Explain. Simply. Clearly. "This is the same medicine. The only difference is the price."
Because satisfaction isn’t about the pill. It’s about the story behind it. And right now, too many stories are wrong.
Are generic drugs really as effective as brand-name drugs?
Yes. By law, generic drugs must contain the same active ingredients, in the same strength, and work the same way as their brand-name counterparts. The FDA requires them to be bioequivalent - meaning they deliver the same amount of medicine into your bloodstream within the same timeframe. Studies show they work just as well for the vast majority of patients. The difference is in the inactive ingredients (like fillers or dyes), which rarely affect how the drug works - but can affect how patients feel about it.
Why do some patients feel worse after switching to a generic?
It’s often not the drug itself. It’s the change. When a pill looks different - different color, shape, or size - the brain can interpret that as a change in effectiveness. Some patients report side effects because they expect them (the nocebo effect). Others may be reacting to different inactive ingredients. For drugs with narrow therapeutic windows - like thyroid meds or seizure drugs - even tiny variations in absorption can feel noticeable. If you feel worse, talk to your doctor. You may need a different generic brand or to stay on the original.
Do doctors and pharmacists influence patient satisfaction with generics?
Absolutely. Studies show that when healthcare providers explain that generics are equivalent and safe, patient satisfaction increases by over 30%. Patients trust their doctors. If the doctor says, "This is the same medicine," patients are far more likely to accept it. If the provider stays silent, patients assume the worst. Communication is the most powerful tool we have to improve generic acceptance.
Which generic medications have the lowest patient satisfaction?
Antiepileptics, antidepressants, and thyroid medications like levothyroxine consistently show the lowest satisfaction rates. This is because they have narrow therapeutic windows - small changes in dosage can lead to noticeable effects. Patients are also more sensitive to changes in these drugs because they’re managing serious, chronic conditions. Online forums show the most complaints around these classes, often tied to perceived changes in mood, energy, or seizure control.
Is there a way to measure patient satisfaction with generics accurately?
Yes. Tools like the Generic Drug Satisfaction Questionnaire (GDSQ) are validated and widely used. It measures effectiveness, convenience, and side effects across 12 questions. More advanced methods include discrete choice experiments (DCE), where patients choose between options, and machine learning models that predict acceptance based on behavior and demographics. The key is using the right tool for the context - surveys alone can miss deeper attitudes. The FDA and European regulators are now funding AI tools that analyze social media and patient reviews to capture real-world sentiment.
Suzette Smith
February 10, 2026 AT 04:52I switched my generic lisinopril last month and my blood pressure actually dropped lower than it ever did on the brand. Funny how people swear the generic doesn't work when they never even checked their numbers first. I'm not saying everyone's lying, but maybe stop blaming the pill and start blaming your own confirmation bias.
Autumn Frankart
February 11, 2026 AT 14:01Let’s be real - the FDA doesn’t test generics like they claim. Big Pharma owns the regulators. They let companies use cheap fillers like talc and magnesium stearate that mess with absorption. You think your thyroid meds are the same? Think again. There’s a whole underground network of pharmacists who know which generics are actually counterfeit. You’re being manipulated. And they’re laughing all the way to the bank.
Pat Mun
February 12, 2026 AT 18:51Okay, I’ve been on generic levothyroxine for five years now, and honestly? I didn’t notice a thing. But I also had my pharmacist sit down with me for 20 minutes and explain exactly what’s in it - the dyes, the binders, why the pill looks different. She showed me the FDA’s bioequivalence charts. I didn’t just accept it - I understood it. And that made all the difference. I think we’re so quick to panic about pills because we’re not taught how to talk to our doctors. We’re just handed a script and told to shut up and swallow. No wonder people freak out. If you’re worried, ask. Really ask. Not just ‘is this okay?’ but ‘why is this okay?’
Sophia Nelson
February 12, 2026 AT 20:05Why are we even having this conversation? The system is rigged. You think your doctor cares if you take a $4 pill or a $40 one? They get paid by volume. They don’t care if you feel weird - as long as you’re not complaining loudly enough to get them audited. And don’t get me started on insurance companies forcing switches. It’s not about health. It’s about profit. Period.
Skilken Awe
February 14, 2026 AT 14:29Let’s cut through the jargon. The bioequivalence threshold is 80-125% - meaning a generic can deliver 25% less or 25% more of the active ingredient and still be deemed ‘equivalent.’ That’s not science. That’s a statistical loophole. You’re telling me a patient on 50mg of a drug is fine when their blood level fluctuates by ±12.5mg? That’s not bioequivalence. That’s Russian roulette with your endocrine system. And don’t even get me started on the fact that manufacturers aren’t required to disclose inactive ingredients beyond the FDA’s minimal checklist. You’re not just taking a drug - you’re taking a cocktail of unregulated fillers. Welcome to modern pharmacology.
andres az
February 15, 2026 AT 20:40AI analyzing social media? Please. You think people on Reddit know what a therapeutic window is? They say ‘I felt worse’ and you call that data? It’s noise. The real issue isn’t perception - it’s the fact that generic manufacturers aren’t held to the same quality control standards as brand-name companies. No one checks their production lines. No one audits their storage conditions. And yet we’re supposed to trust a pill that might’ve sat in a warehouse in India for six months before it got shipped to Walmart? Yeah right.
Steve DESTIVELLE
February 17, 2026 AT 13:49When the body receives a pill it does not see chemistry it sees ritual the color the shape the imprint the texture of the tablet are not incidental they are symbolic the body remembers the brand not because it is better but because it is known the mind constructs meaning from form and when form changes the meaning collapses even if the substance remains unchanged this is not irrational this is human
Stephon Devereux
February 18, 2026 AT 14:23Here’s what nobody talks about: the placebo effect works both ways. If you believe a generic is inferior, your brain literally changes how your body responds to it. That’s not just psychology - it’s neurobiology. The same neural pathways that activate when you expect relief are the ones that amplify side effects when you expect failure. That’s why counseling works. Not because it changes the pill - but because it changes your brain’s expectation. And here’s the kicker: if your doctor says, ‘This is the same,’ and you believe them, your body responds like it’s the brand. It’s not magic. It’s biology. We’ve got the tools to fix this - we just need to stop treating patients like they’re dumb and start treating them like they’re human.
steve sunio
February 19, 2026 AT 17:15generic drugs are a scam plain and simple the fda is corrupt and big pharma owns them you think they care about you? they care about profit. i switched to generic and got worse i went to my doctor and they said ‘its all in your head’ lol no its in your wallet. they dont want you to know that the inactive ingredients are toxic and cause inflammation. i read a blog once that said 70% of generic users have higher crp levels. dont trust anyone who says its the same
Frank Baumann
February 20, 2026 AT 13:18I’m not even mad - I’m disappointed. We’ve got AI, DNA testing, real-time health tracking… and we’re still arguing about whether a blue pill is the same as a white one? This isn’t about science. It’s about fear. Fear of change. Fear of losing control. Fear of being told you’re wrong. But here’s the truth: your body doesn’t care about labels. It cares about absorption, metabolism, clearance. If your thyroid levels are stable, your BP is under control, your mood is steady - then stop obsessing over the imprint on the pill. The real crisis isn’t the generic - it’s our refusal to trust science, our addiction to narratives, and our refusal to have honest conversations with our providers. We’re not patients. We’re consumers with anxiety disorders.
John McDonald
February 22, 2026 AT 00:53My grandma takes generic metformin and she says it works fine. She doesn’t know what bioequivalence means. She just knows she’s not broke. And she’s alive. Maybe the answer isn’t more surveys or AI. Maybe it’s just talking to people. Not experts. Not studies. Just real humans who’ve been on these meds for 15 years and are still here. If you’re worried, talk to your pharmacist. Ask them what they take. Ask them if they’ve switched. You’ll be surprised how many say, ‘Oh yeah, I’ve been on the generic for years - no problems.’