Recognizing and Treating Medication-Induced Restless Legs and Akathisia
 Jan, 23 2026
Jan, 23 2026
Akathisia Symptom Checker
What is akathisia?
Akathisia is a medication-induced movement disorder characterized by an overwhelming need to move. It's often misdiagnosed as anxiety or agitation. This tool helps you assess whether your symptoms might be akathisia rather than other conditions.
Do you feel an inner need to move even when you want to sit still?
Do you shift your weight, cross and uncross your legs, or pace while sitting?
Do your symptoms worsen when you try to sit still?
When you start a new medication-especially an antipsychotic-you expect relief from your symptoms, not new ones that feel worse. But for many, a strange, unbearable urge to move takes over. Legs twitch. Feet tap. You can’t sit still. Your doctor calls it anxiety. You’re told to take more pills. Instead of getting better, you feel like you’re losing control. This isn’t anxiety. It could be akathisia-a medication-induced movement disorder that’s often misdiagnosed and dangerously under-treated.
What Is Akathisia, and How Is It Different from Restless Legs?
Akathisia isn’t just fidgeting. It’s a deep, internal torment that makes you feel like you’re trapped in your own skin. You don’t just want to move-you have to move. It’s not about discomfort like a cramp. It’s a crushing, agitated restlessness that makes sitting impossible. You might pace back and forth, cross and uncross your legs repeatedly, shift your weight constantly, or rock in place. These movements aren’t voluntary. They’re desperate attempts to quiet an inner storm. Restless Legs Syndrome (RLS) feels similar, but it’s different. RLS usually shows up at night or when you’re resting. It’s a crawling, tingling, or aching sensation in the legs that only eases when you move. Akathisia hits anytime, especially when seated, and affects your whole body-not just your legs. It’s not relieved by stretching or walking. It’s worsened by stillness. The biggest clue? Timing. Akathisia shows up within days to weeks after starting or increasing a medication like haloperidol, risperidone, or even metoclopramide. RLS has no such link to drugs-it’s often genetic or tied to low iron. If your restlessness started after a new prescription, akathisia is far more likely.Why Misdiagnosis Is Dangerous
Here’s the scary part: doctors miss akathisia more than half the time. A 2020 review in the Journal of Clinical Psychiatry found that up to 50% of cases are labeled as anxiety, agitation, or worsening psychosis. So what happens next? The patient gets a higher dose of the very drug causing the problem. That’s like pouring gasoline on a fire. A 2017 case study from the Royal Australian College of General Practitioners followed a patient on haloperidol who developed severe inner restlessness. His doctor thought it was anxiety and doubled his dose. Within days, he became suicidal. Only after stopping the medication-and adding clonazepam-did he return to normal. That’s not rare. In fact, the American Psychiatric Association warns that untreated akathisia is linked to aggression, violence, and suicide. Patients describe it as worse than the psychosis they were being treated for. One Reddit user wrote: “My doctor kept saying it was anxiety and doubled my Seroquel dose. It made the leg bouncing and inner turmoil 10x worse.” Another told a support group: “I’d rather have the voices back than this feeling of being torn apart from the inside.”Which Medications Cause Akathisia?
Not all drugs cause it-but some are far riskier. First-generation antipsychotics like haloperidol and fluphenazine carry the highest risk because they strongly block dopamine receptors. Up to 40% of people on these meds develop akathisia. Second-generation antipsychotics like risperidone, olanzapine, and quetiapine are better but still risky. About 5-15% of users experience it. Even metoclopramide (used for nausea and acid reflux) can trigger it, especially at high doses or with long-term use. Newer drugs like lumateperone (Caplyta) have lower rates-just 3.6% in clinical trials-making them a better option for people with a history of movement side effects.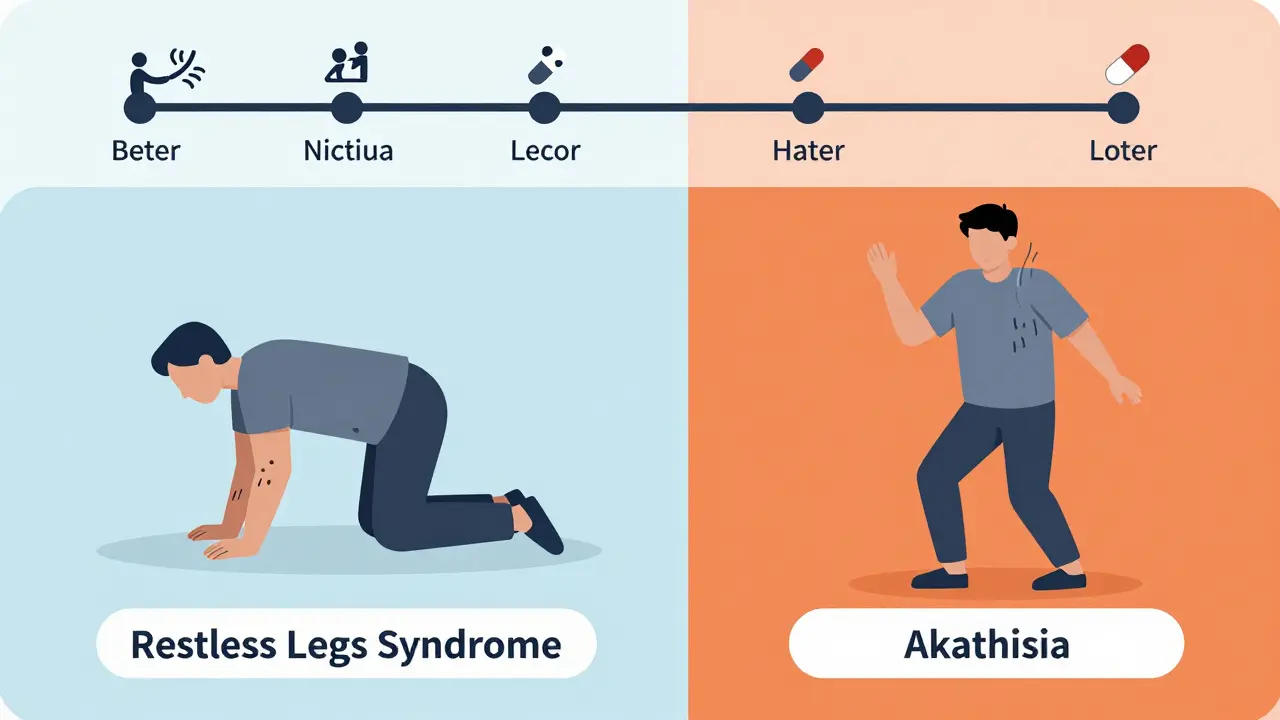
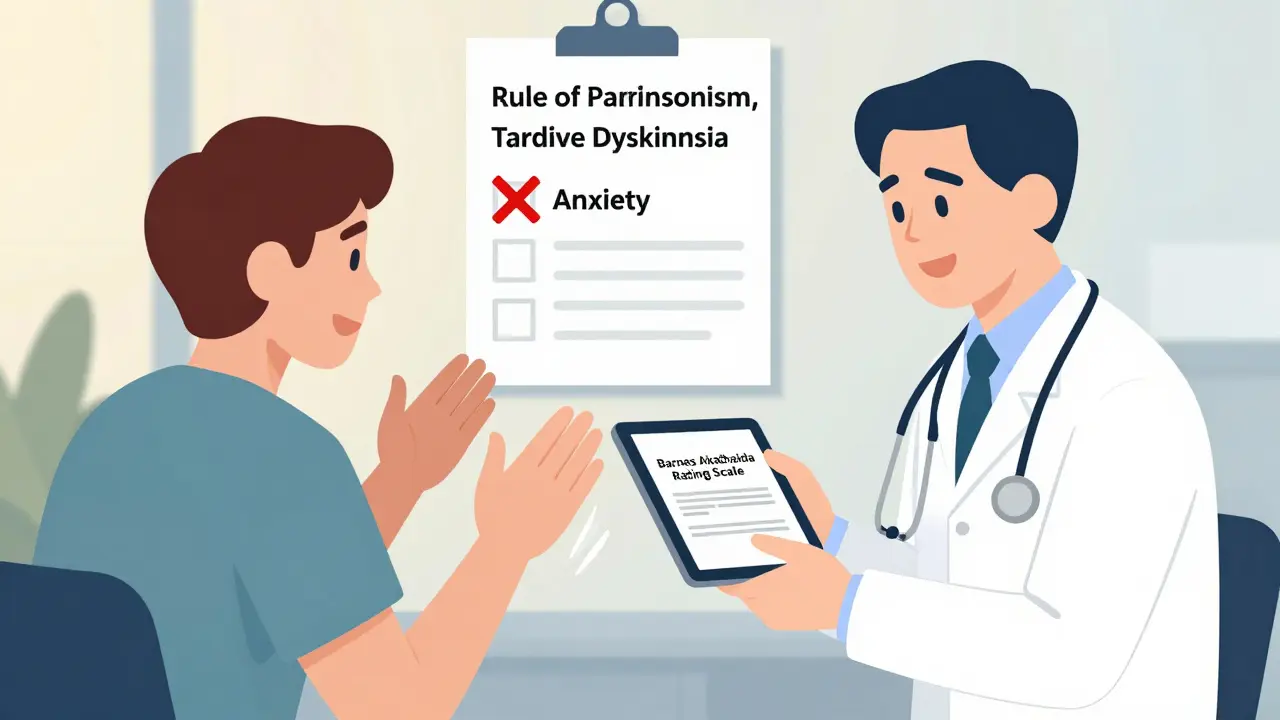
How Doctors Should Diagnose It
There’s no blood test. No scan. Diagnosis comes from asking the right questions and watching closely. The Barnes Akathisia Rating Scale (BARS) is the gold standard. It takes five minutes. It rates two things:- Subjective restlessness: “Do you feel an inner need to move? Does it feel like you can’t sit still, even if you want to?”
- Objective movement: “Do you shift your weight, cross and uncross your legs, or pace while sitting?”
- Parkinsonism: Slowed movement, stiff muscles, tremors
- Tardive dyskinesia: Involuntary lip-smacking, tongue protrusion, or chorea (jerky movements)
Treatment: Stop the Drug-or Add a Shield
The best fix? Stop the medication causing it. But that’s not always possible. If someone needs the antipsychotic for severe psychosis, reducing the dose too fast can trigger relapse. So doctors often use add-on treatments:- Propranolol (10-60 mg daily): A beta-blocker that calms the nervous system. Works for about 60% of patients.
- Clonazepam (0.5-2 mg nightly): A benzodiazepine that reduces inner tension. Fast-acting, but risk of dependence.
- Cyproheptadine (4 mg daily): An antihistamine with serotonin-blocking effects. Less common, but helpful in stubborn cases.
What Patients Should Do
If you’re on an antipsychotic and feel restless, don’t wait. Don’t assume it’s “just anxiety.”- Write down when the symptoms started and what you were doing when they hit.
- Track whether movement helps-or makes it worse.
- Bring up akathisia by name. Say: “I think this might be akathisia. Can we check?”
- Ask if the Barnes Scale has been used.
- If your doctor dismisses you, ask for a referral to a movement disorder specialist or psychiatrist experienced in side effects.
The Future: Better Tools, Fewer Mistakes
Progress is happening. In 2023, the International Parkinson and Movement Disorder Society launched an Akathisia Recognition and Management App that helps clinicians screen patients in real time. Researchers are testing new treatments. A 2023 trial found pimavanserin (Nuplazid), a drug used for Parkinson’s hallucinations, reduced akathisia by 62%. Early studies at Harvard are exploring transcranial magnetic stimulation to calm overactive brain circuits. Even AI is stepping in. Stanford’s 2024 pilot study used video analysis to detect akathisia movements during telehealth visits-with 89% accuracy. That could make diagnosis faster and more reliable. But until these tools are everywhere, the most powerful tool remains awareness. If you’re a patient, know your symptoms. If you’re a provider, ask the right questions.When to Seek Help Immediately
Akathisia isn’t just uncomfortable-it’s life-threatening. Go to the ER or call your doctor right away if you experience:- Thoughts of self-harm or suicide
- Uncontrollable aggression or rage
- Overwhelming panic or feeling like you’re losing your mind
Final Thoughts
Akathisia is not rare. It’s not imaginary. It’s not anxiety. It’s a real, measurable, and treatable side effect of common medications. Too many people suffer needlessly because no one recognizes it. But you can change that. If you’re on an antipsychotic and feel like you can’t sit still-if you’ve been told it’s “just nerves”-ask for the Barnes Scale. Ask about alternatives. Ask for help. Your restlessness isn’t weakness. It’s a signal. Listen to it.Can akathisia go away on its own?
Sometimes, yes-but only if the triggering medication is stopped or reduced. Akathisia doesn’t resolve with time if the drug is still being taken. In fact, it often gets worse. If symptoms start within weeks of a new medication, stopping or lowering the dose usually leads to improvement within days to weeks. Some cases, especially chronic or tardive akathisia, may require ongoing treatment with propranolol or clonazepam.
Is akathisia the same as ADHD or anxiety?
No. ADHD involves difficulty focusing and impulsivity, not a compelling need to move due to inner distress. Anxiety may cause restlessness, but it’s usually tied to worry, not physical torment. Akathisia is defined by an overwhelming, involuntary urge to move that isn’t relieved by distraction or calming techniques. People with akathisia often describe it as a physical ache or burning sensation-not just mental stress.
Can antidepressants cause akathisia?
Yes. While antipsychotics are the most common cause, certain antidepressants-especially SSRIs like fluoxetine (Prozac) and sertraline (Zoloft)-can trigger akathisia, particularly when started or increased. It’s less common than with antipsychotics, but still well-documented. If restlessness begins after starting an antidepressant, akathisia should be considered.
Why don’t doctors know more about akathisia?
Medical training often focuses on diagnosing psychiatric conditions, not medication side effects. Many doctors aren’t taught to recognize akathisia as a distinct disorder. A 2022 report found only 37% of U.S. psychiatric facilities routinely screen for it. Even when symptoms are present, they’re mistaken for anxiety, agitation, or non-compliance. The result? Underdiagnosis and dangerous treatment errors.
Are there natural remedies for akathisia?
There’s no proven natural cure. Supplements like magnesium or vitamin B6 may help with restless legs syndrome, but they don’t reliably treat akathisia. The most effective approach is medical: adjusting the medication or using proven drugs like propranolol or clonazepam. Trying unproven remedies can delay proper treatment and worsen symptoms.
Shanta Blank
January 23, 2026 AT 17:59This is why I stopped taking SSRIs cold turkey-no doctor ever warned me about the inner screaming. I thought I was losing my mind until I read about akathisia on Reddit. My legs felt like they were on fire and I was pacing my apartment for 12 hours straight. They called it anxiety. I called it torture. And now I’m off all meds and still breathing. 🤯
Josh McEvoy
January 25, 2026 AT 17:30bro i had this after my first dose of risperidone… i thought i was having a panic attack but it wasnt anxiety it was like my bones were begging me to move. i told my dr and he just upped my dose. i almost jumped off my balcony. i still have nightmares about that week. 🫠
Alexandra Enns
January 27, 2026 AT 06:50Oh please. This is just woke medicine nonsense. Everyone’s too fragile now to handle a little discomfort. Back in my day, we took our meds like adults and didn’t whine about ‘inner torment.’ If you can’t sit still, maybe you need to get a job and stop being a hypochondriac. This isn’t a movie script. It’s pharmacology. Stop dramatizing everything. 🤦♀️
Marie-Pier D.
January 28, 2026 AT 11:03To Alexandra-please stop. This is real suffering. I’ve seen friends spiral because doctors dismissed this as ‘anxiety.’ One of them tried to end it all because she thought she was broken. She wasn’t. The drug was. Please don’t shame people for surviving. 💛 You don’t have to understand it to believe it. And if you’re a doctor? Please, just ask the Barnes Scale. Five minutes could save a life.
Sawyer Vitela
January 28, 2026 AT 20:37Propranolol works. Clonazepam works. Stopping the drug works. Everything else is noise. You don’t need a 3000-word essay. You need to stop the dopamine blocker. Done.
Heather McCubbin
January 29, 2026 AT 20:26They call it akathisia but really its the system failing people again. Big Pharma doesn’t want you to know this happens. They profit off the cycle. You get the drug. You get the side effect. You get a higher dose. You get suicidal. You get hospitalized. They get your insurance money. Its not medicine its a money machine. And your doctor? They’re just a cog. 💔
Tiffany Wagner
January 29, 2026 AT 22:17i never knew this had a name… i thought i was just weird. i started sertraline and suddenly i couldnt sit through a movie without pacing. i told my therapist and she said ‘maybe try yoga?’ i cried in the parking lot. thank you for putting this out there. i feel less alone now
Chloe Hadland
January 30, 2026 AT 06:04thank you for writing this. i’ve been too scared to speak up because everyone says ‘just relax’ or ‘you’re overreacting.’ but this? this is exactly what i felt. i didn’t know i was supposed to ask for the barnes scale. i’m going to print this out and take it to my next appointment. you gave me courage
Himanshu Singh
February 1, 2026 AT 05:27as someone from india where psych meds are handed out like candy, i’ve seen this too many times. doctors don’t even know what akathisia is. they say ‘take more’ and move on. this article is a gift. please share it with every clinic, every pharmacy, every family member who’s on antipsychotics. we need to change this. 🙏
Helen Leite
February 1, 2026 AT 16:36you know who really controls this? The Illuminati. They want you restless so you’ll take more pills. The Barnes Scale? Fake. The whole thing’s a psyop to keep you dependent. They’ve been doing this since the 50s. Look up MKUltra. They don’t care if you die. They just want your brain wired. 🕵️♀️👁️