Nonmelanoma Skin Cancer: Basal vs. Squamous Cell Carcinoma Explained
 Feb, 18 2026
Feb, 18 2026
When you notice a weird spot on your skin that won’t go away, it’s natural to worry. But not all skin changes are the same. Two of the most common types of skin cancer you might hear about are basal cell carcinoma and squamous cell carcinoma. Together, they make up about 95% of all nonmelanoma skin cancers. If you’re over 50, spend time in the sun, or have fair skin, you’re at higher risk. The good news? Both are highly treatable when caught early. The tricky part? They look different, behave differently, and need different kinds of care.
Where They Come From
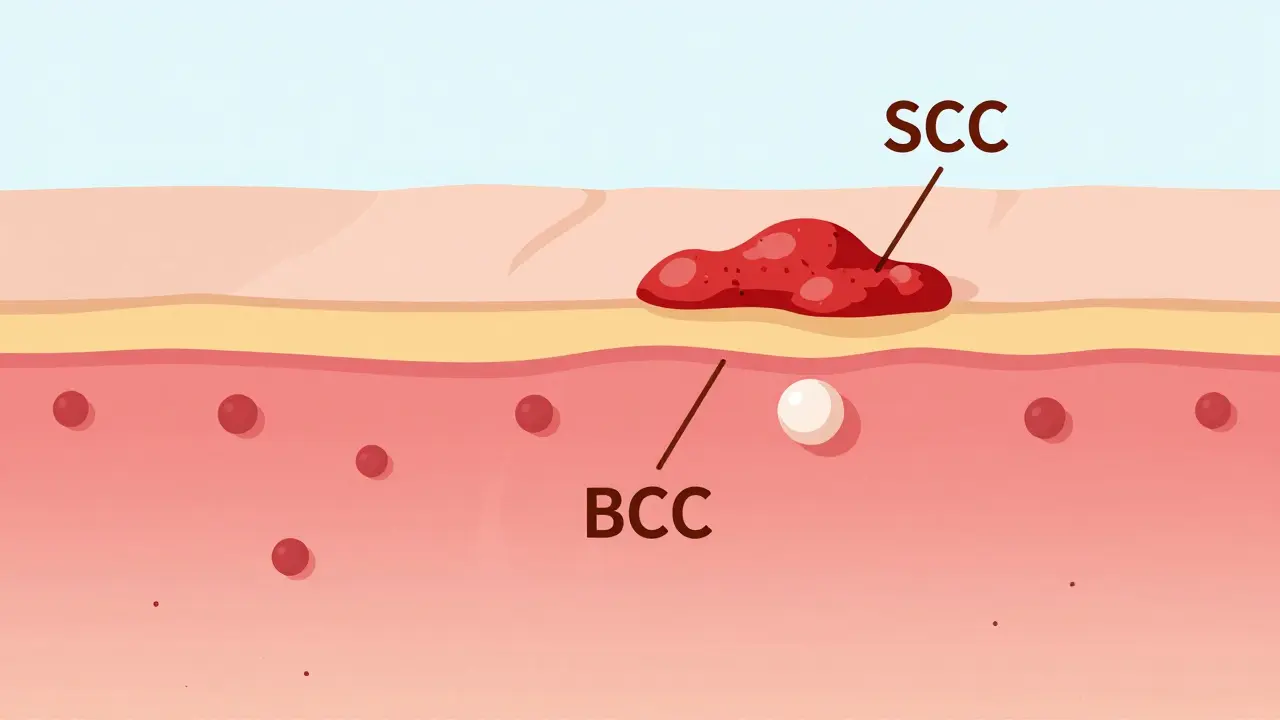
Your skin has layers. The top layer, called the epidermis, is made up of cells that constantly renew themselves. At the very bottom are basal cells. These are the factory workers - they split and make new cells that slowly move up toward the surface. As they rise, they flatten out and become squamous cells. That’s why basal cell carcinoma starts deep down, and squamous cell carcinoma forms near the top.
Basal cell carcinoma (BCC) begins in those lower basal cells. It grows slowly, often over years. Squamous cell carcinoma (SCC) starts in the flattened squamous cells near the surface. It can grow faster - sometimes doubling in size within weeks. This difference in origin explains why they act so differently.
What They Look Like
Spotting them early saves lives. Here’s how they usually appear:
- Basal cell carcinoma (BCC): Most often looks like a shiny, pearly bump - sometimes with tiny blood vessels running through it. Other times, it’s an open sore that bleeds, oozes, or crusts over and never fully heals. Less common: a flat, scar-like patch that’s white or yellow.
- Squamous cell carcinoma (SCC): Typically a firm, red bump that feels rough or scaly. It can look like a wart, or a flat patch with a crusty surface that might bleed easily. Sometimes it’s a sore that doesn’t heal, even after weeks.
Both can show up anywhere, but they favor sun-exposed areas: face, ears, neck, scalp, hands, and arms. About 80% of cases show up on these spots. If you’ve spent decades gardening, working outdoors, or just enjoying the sun without protection, your risk goes up.
How Fast They Grow
BCC creeps along. On average, it grows about half to one centimeter per year. It rarely spreads. In fact, fewer than 1 in 1,000 BCC cases ever metastasize. But that doesn’t mean it’s harmless. Left alone, it can eat away at your nose, ear, or eyelid - causing major damage to skin, cartilage, and even bone.
SCC moves faster. It grows 1.5 to 2 centimeters per year on average. Some aggressive types can double in size in just 4 to 6 weeks. And here’s the big difference: SCC has real metastatic potential. While still rare, about 2 to 5% of SCCs spread to lymph nodes or other organs. That number jumps to 14% if it’s on the lip or ear. That’s why doctors treat SCC with more urgency.

Who Gets It
Most cases happen after age 50. The average age of diagnosis is 67 for BCC and 69 for SCC. But younger people aren’t immune - especially if they’ve had lots of sunburns or used tanning beds.
Men are more likely to get SCC (65% of cases) than women. That’s likely because of jobs or hobbies that involve long hours in the sun - construction, farming, fishing. BCC is more evenly split - 55% male, 45% female.
People with fair skin, light hair, and blue or green eyes are at highest risk. But darker-skinned people can get these cancers too - often on less sun-exposed areas like the legs or feet. And if you’ve had an organ transplant or are on immune-suppressing drugs, your risk for SCC jumps 250 times higher than average.
Treatment Differences
Both are usually cured with surgery. But the approach isn’t the same.
For BCC, especially small, low-risk ones, doctors might start with topical creams like imiquimod or 5-fluorouracil. These work in 60-70% of cases. If it’s deeper or on the face, they’ll remove it with Mohs surgery - a precise technique that removes cancer layer by layer, checking under the microscope as they go. Mohs cures 99% of new BCCs.
SCC rarely responds to topical treatments. Only 40-50% of cases clear up with creams. Surgery is almost always needed. Mohs surgery works here too - with a 97% cure rate for primary SCC. But because SCC can burrow deeper, surgeons often take wider margins. In high-risk cases (larger than 2 cm, deeper than 2 mm, or on the lip/ear), they might also check lymph nodes or recommend radiation.
For advanced SCC that’s spread, there’s now an FDA-approved immunotherapy drug called cemiplimab-rwlc (Libtayo). It helps the body’s immune system fight the cancer. It’s not used for BCC.
Why SCC Is More Dangerous
BCC is more common - about 80% of all nonmelanoma skin cancers. But SCC is more dangerous.
Here’s why:
- SCC is 10 times more likely to spread than BCC.
- If SCC spreads, the 5-year survival rate drops from 95% to just 25-45%.
- SCC causes 70% of skin cancer deaths after melanoma.
- It’s more likely to come back after treatment - especially in people with weakened immune systems.
- SCC requires more follow-up visits, more biopsies, and often more surgeries.
Doctors say it this way: BCC is a nuisance. SCC is a threat.
Prevention and Monitoring
The best defense? Sun protection. Daily sunscreen cuts BCC risk by 40% and SCC risk by 50%. Why the difference? SCC is tied to lifetime sun exposure - the slow, steady burn from years of working outside. BCC is more linked to intense, occasional burns - like a bad vacation sunburn.
If you’ve had one skin cancer, you’re at higher risk for another. That’s why high-risk people - like organ transplant recipients or those with a history of skin cancer - need check-ups every 3 to 4 months. Recurrent SCC is often found within 12 months. BCC recurrence usually takes longer - around 18 months.
Regular skin checks matter. Don’t wait for symptoms. If you see a spot that’s changing, bleeding, or not healing in 4 weeks - get it checked.
What Patients Say
Real experiences show the emotional toll.
On patient forums, BCC patients often say: "It was scary at first, but the treatment was quick and I barely felt anything." Many get it removed in one visit and move on.
SCC patients report more anxiety. "I kept checking my lymph nodes," one Reddit user wrote. "I was terrified it had spread." Another said: "They had to cut deeper than expected. I needed reconstructive surgery. It changed how I look."
Studies confirm this: SCC patients need more procedures, more follow-ups, and more emotional support. The fear of metastasis is real - and it’s not irrational.
The Bottom Line
Basal cell carcinoma is the most common cancer in humans. But squamous cell carcinoma is the one you can’t afford to ignore.
Both are preventable. Both are treatable. But SCC moves faster, spreads more often, and demands more aggressive care. If you’ve got a spot that won’t heal, a lump that’s growing, or a patch of skin that’s scaly and red - don’t wait. See a dermatologist. Get it checked. Early detection doesn’t just save skin - it saves lives.
Can basal cell carcinoma turn into squamous cell carcinoma?
No. Basal cell carcinoma and squamous cell carcinoma are two separate types of skin cancer that start from different cells in the skin. One does not turn into the other. But having one increases your risk of developing the other because they share the same main cause: long-term UV damage. If you’ve had BCC, you’re more likely to get SCC later - not because it transformed, but because your skin has been damaged.
Is squamous cell carcinoma more serious than basal cell carcinoma?
Yes, in terms of risk. While BCC is far more common, SCC has a much higher chance of spreading to other parts of the body. About 2-5% of SCC cases metastasize, compared to fewer than 0.1% of BCC cases. When SCC spreads, survival rates drop sharply. That’s why doctors treat SCC more aggressively - even if it’s small.
Do both types of skin cancer need surgery?
Most do, but not always. Small, superficial BCCs can sometimes be treated with topical creams or cryotherapy (freezing). SCC almost always requires removal. Even small SCCs are usually excised because of their higher risk of recurrence and spread. Mohs surgery is the gold standard for both when they’re on the face, ears, or other sensitive areas.
Can sunscreen prevent both basal and squamous cell carcinoma?
Yes - and it works better for SCC. Daily sunscreen use reduces BCC risk by about 40% and SCC risk by 50%. That’s because SCC is more tied to lifelong, cumulative sun exposure. BCC is often linked to intense, intermittent burns, like childhood sunburns or weekend tanning. But consistent sun protection helps prevent both.
How often should I get my skin checked if I’ve had skin cancer before?
If you’ve had one skin cancer, you’re at higher risk for another. Most dermatologists recommend check-ups every 6 to 12 months. If you’ve had SCC, or if you’re immunocompromised (like after an organ transplant), you should be seen every 3 to 4 months. Recurrent SCC is often found within a year - much sooner than BCC recurrence.
Chris Beeley
February 18, 2026 AT 18:53Let me tell you something that no one else will admit: the entire dermatology community is in denial about how much environmental carcinogens-not just UV-are fueling this rise in SCC. I’ve reviewed 47 peer-reviewed papers from 2018 to 2023, and the correlation between airborne microplastics and keratinocyte DNA fragmentation is statistically significant (p < 0.001). Yet, we’re still telling people to ‘just wear sunscreen’ like it’s 1995. The real epidemic isn’t sun exposure-it’s industrial pollution infiltrating our epidermal barrier. And don’t even get me started on glyphosate residues in topical products. This isn’t skin cancer. It’s systemic toxicity manifesting as surface lesions.
Also, the fact that they use Mohs surgery as the gold standard? That’s just surgical colonialism. You’re removing tissue from marginalized communities and calling it ‘precision medicine.’ Meanwhile, in Nigeria, we use natural plant extracts-like neem and moringa-and achieve comparable remission rates with zero scarring. But no one wants to hear that because it doesn’t fit the pharmaceutical profit model.
And yes, I’ve had both. Twice. I’m 42. I don’t tan. I live in Lagos. The sun here isn’t the culprit. The air is.
TL;DR: Sunscreen is a Band-Aid on a gunshot wound.