Mood Stabilizers: Lithium, Valproate, and Carbamazepine Interactions Explained
 Dec, 4 2025
Dec, 4 2025
Mood Stabilizer Interaction Checker
Check Your Medication Interactions
Select your mood stabilizer and another medication to see potential interactions and safety guidelines.
Interaction Result
Low RiskWhen you’re taking a mood stabilizer like lithium, valproate, or carbamazepine, even a simple over-the-counter painkiller can change how your medication works-sometimes dangerously. These aren’t just regular pills. They sit on a razor’s edge: too little and your mood crashes or spirals; too much and you risk tremors, confusion, seizures, or worse. The problem isn’t just the drugs themselves. It’s how they talk to everything else you take. And most people don’t realize how complex that conversation is until something goes wrong.
Lithium: The Kidney’s Responsibility
Lithium doesn’t get broken down by your liver. It doesn’t bind to proteins. It doesn’t get metabolized at all. It just passes through your kidneys and out in your urine. That makes it simple in theory-but incredibly fragile in practice. Anything that messes with your kidney function or sodium balance can send lithium levels skyrocketing.
Take NSAIDs like ibuprofen or naproxen. These are common for headaches or joint pain. But in someone on lithium, they can reduce kidney clearance by 25-30%. That means lithium builds up fast. One patient in Melbourne reported tremors and confusion after starting ibuprofen for back pain. Their lithium level jumped from 0.8 to 1.3 mmol/L in three days. That’s not just a number-it’s a warning sign. Levels above 1.2 mmol/L can cause toxicity. Above 1.5? That’s an emergency.
Diuretics are another hidden risk. Thiazide diuretics, often prescribed for high blood pressure, cause your body to hold onto sodium. That tricks your kidneys into reabsorbing more lithium. Studies show lithium levels can rise 25-40% with these drugs. Even ACE inhibitors, common for heart health, can push lithium levels up by about 25%. The fix? Don’t stop your blood pressure meds. But do check your lithium level 5-7 days after starting any new medication. Keep your levels at the lower end of safe range-0.6 to 0.8 mmol/L-when you’re on these combinations.
Hydration matters too. Dehydration from heat, illness, or not drinking enough can concentrate lithium in your blood. That’s why doctors tell you to drink water-even if you’re not thirsty. The acronym LITH helps: Level monitoring, Instruct about symptoms, Teach hydration, Hold if toxic signs appear. Coarse tremors, dizziness, nausea, or confusion? Get your level checked immediately.
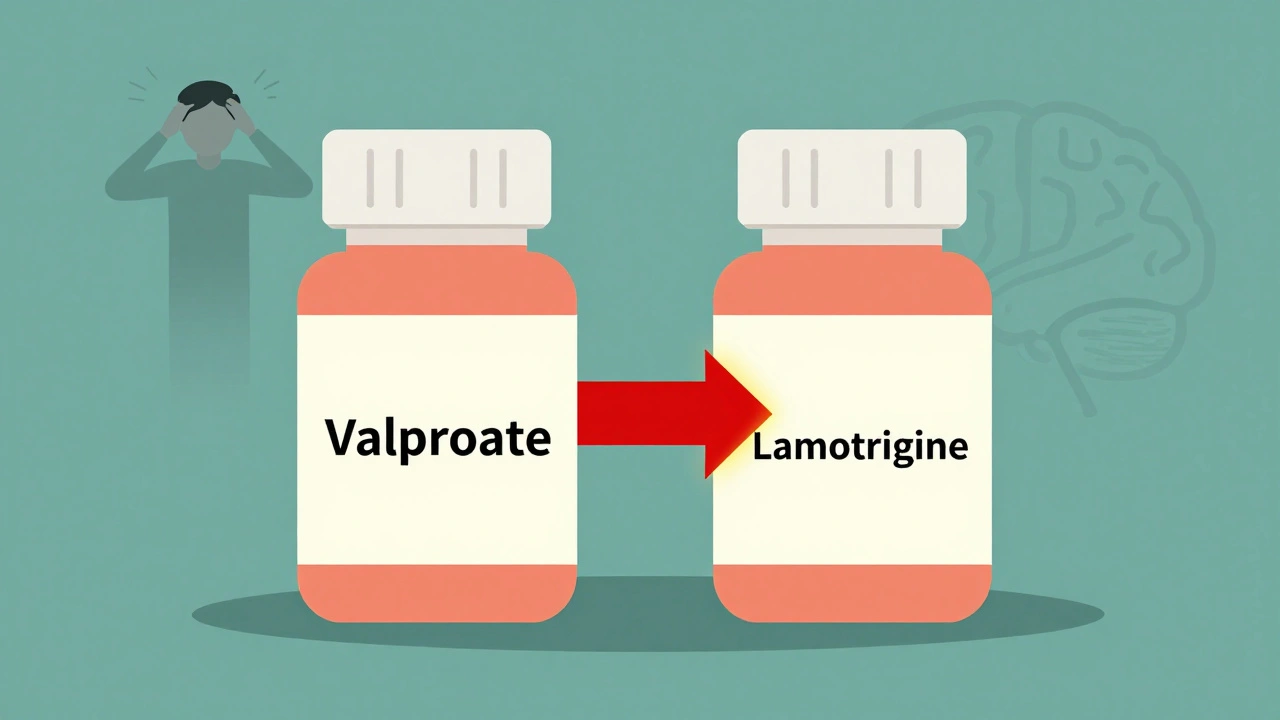
Valproate: The Double-Edged Sword
Valproate is different. It’s mostly processed by the liver through three pathways: glucuronidation, beta-oxidation, and a bit of CYP450. That gives it some buffer-if one pathway gets blocked, others can compensate. But it also binds tightly to proteins. When levels go above 100 mcg/mL, that binding becomes unpredictable. Free, active drug can spike even if total levels look fine.
Here’s the twist: valproate doesn’t just get affected-it affects others. It’s a powerful inhibitor of liver enzymes. When you add valproate to lamotrigine, lamotrigine levels can double or even triple. That’s why people switching from carbamazepine to valproate often need to cut their lamotrigine dose in half. One Reddit user described going from 400mg to 200mg overnight after the switch. That’s not a coincidence-it’s science.
But valproate also gets knocked down by other drugs. Carbamazepine, for example, speeds up valproate’s breakdown through glucuronidation. Studies show valproate levels can drop by 30-50% when taken with carbamazepine. That’s dangerous. If your mood stabilizer isn’t working, it might not be your illness-it’s the drug interaction.
And then there’s the bigger issue: pregnancy. Valproate carries a 10.7% risk of major birth defects-more than four times the background rate. It’s also linked to lower IQ in children exposed in utero. Since 2013, the FDA has required a boxed warning. In Australia and the U.S., prescriptions for women of childbearing age have dropped by 65%. Many now avoid it entirely unless there’s no other option.
Carbamazepine: The Metabolic Dynamo
Carbamazepine doesn’t just interact-it rewires your liver. It’s an inducer. That means it tells your body to make more of the enzyme CYP3A4, which breaks down drugs. At first, it has a half-life of 35-40 hours. After three to five weeks, that drops to 12-17 hours because your liver is working overtime. That’s why doses often need to be increased over time-unless you’re on something that blocks it.
That’s where valproate comes in. Valproate doesn’t slow down carbamazepine itself. It slows down the cleanup crew. Carbamazepine turns into an active metabolite called carbamazepine-epoxide (CBZ-E). Normally, your body breaks that down quickly. But valproate blocks the enzymes that do that job. So CBZ-E builds up-by 40-60%. That’s the real problem. CBZ-E causes dizziness, ataxia, nausea. It’s the main reason people feel off on this combo, even if carbamazepine levels look normal.
Doctors now monitor both carbamazepine and CBZ-E levels. The target for CBZ-E is under 3.5 mcg/mL. If it’s higher, you’re at risk for neurotoxicity. The fix? Reduce the carbamazepine dose by 25% when starting valproate. And keep checking levels every few weeks until things stabilize.
Carbamazepine also wrecks other meds. Oral contraceptives? Levels can drop by 50-70%. That’s why birth control fails in women on carbamazepine. Antidepressants like sertraline, antipsychotics like risperidone, even some antibiotics? All get broken down faster. That’s why some people say their meds “stopped working”-they didn’t. Their liver just started working too hard.
The Big Picture: Why These Interactions Matter
These three drugs are the OG mood stabilizers. But their use is changing. In 2012, lithium was prescribed in 35% of new cases. By 2022, that dropped to 15%. Valproate fell from 55% to 40%. Carbamazepine held steady at 10%. Why? Newer drugs like lamotrigine and lurasidone have fewer interactions. They’re safer with other meds. They don’t need weekly blood tests. And they don’t carry the same pregnancy risks.
But here’s the catch: these older drugs still work. Lithium reduces suicide risk by nearly half. Valproate is fast-acting in acute mania. Carbamazepine helps when others fail. So we don’t abandon them-we manage them smarter.
Therapeutic drug monitoring isn’t optional. It’s essential. Lithium levels? Check every 3-6 months, or after any new med. Valproate? Check monthly at first, then every 3-6 months. Carbamazepine and CBZ-E? Check together, especially when starting or stopping another drug.
And don’t forget the human factor. A 2019 survey of 853 psychiatrists found that 74% considered carbamazepine-valproate interactions “moderately to severely problematic.” One in two patients on this combo reported dizziness or balance issues. That’s not just side effects-it’s a sign of toxicity.
What to Do If You’re on One of These Drugs
- Never start or stop any medication without talking to your doctor. That includes herbs, supplements, and OTC painkillers.
- Keep a list of everything you take. Write down doses and why you take them. Bring it to every appointment.
- Know your numbers. Ask for your last lithium, valproate, or carbamazepine level. Don’t assume it’s fine.
- Watch for warning signs. For lithium: tremors, frequent urination, confusion. For valproate: nausea, drowsiness, swelling. For carbamazepine: dizziness, blurred vision, unsteadiness.
- Hydrate. Avoid NSAIDs. Check pregnancy status. These are non-negotiable if you’re on lithium or valproate.
There’s no magic bullet. But with awareness, monitoring, and communication, you can stay stable-and safe.
Can I take ibuprofen if I’m on lithium?
No, not without medical supervision. Ibuprofen and other NSAIDs can reduce lithium clearance by 25-30%, causing toxic buildup. If you need pain relief, talk to your doctor about alternatives like acetaminophen (paracetamol), which doesn’t affect lithium levels. Always check your lithium level 5-7 days after starting any new medication.
Why does valproate make lamotrigine levels go up?
Valproate inhibits the liver enzyme UGT1A4, which is responsible for breaking down lamotrigine. This can increase lamotrigine levels by 100-200%. If you’re switching from carbamazepine to valproate, your lamotrigine dose will likely need to be cut in half to avoid side effects like rash or dizziness. Never adjust your dose without your doctor’s guidance.
Is carbamazepine safe during pregnancy?
Carbamazepine carries a moderate risk of birth defects-around 5-7%-and is classified as pregnancy category D. It’s less risky than valproate (10.7% risk) but still dangerous. If you’re pregnant or planning pregnancy, talk to your doctor about switching to a safer option like lamotrigine. Never stop carbamazepine abruptly-it can trigger seizures or severe mood episodes.
How often should I get my blood tested on mood stabilizers?
For lithium: every 3-6 months if stable, or within 5-7 days after starting a new drug. For valproate: monthly at first, then every 3-6 months. For carbamazepine: check levels and its active metabolite (CBZ-E) when starting, after dose changes, or if you feel unwell. Always test before and after any medication change.
Why is lithium still used if it has so many interactions?
Because it’s one of the most effective drugs for preventing suicide and long-term mood episodes in bipolar disorder. The STEP-BD study showed it prevents manic episodes in 47% of patients. No other mood stabilizer has the same long-term evidence. The key is careful monitoring and avoiding interactions-not avoiding lithium entirely.
Can I drink alcohol while on these mood stabilizers?
Alcohol can worsen side effects like dizziness, drowsiness, and poor coordination. It can also increase the risk of liver damage with valproate and carbamazepine. With lithium, alcohol can dehydrate you, raising your levels. It’s best to avoid alcohol or limit it to very small amounts. Always check with your doctor.
Deborah Jacobs
December 5, 2025 AT 01:41I’ve been on lithium for 12 years and no one ever told me how fragile it is until I got sick from ibuprofen. I thought it was just a headache pill. Turns out, my kidneys were screaming. Now I keep acetaminophen in my medicine cabinet and a note on my fridge: ‘NO NSAIDS.’ My doctor says I’m lucky I didn’t end up in the ER. Seriously, if you’re on this stuff, treat it like live ammo.
Hydration isn’t optional. I drink water like it’s my job. Even when I’m not thirsty. Even when it’s cold. Even when I’m lazy. Because my brain doesn’t work right when lithium creeps up. And I’ve seen what that looks like. Not pretty.
Also, the LITH acronym? Genius. I printed it and taped it to my pill organizer. My mom even started using it when she checks in on me. Small things save lives.
And yeah, I still get mad when people say ‘just take less lithium.’ Like it’s a dial you turn. It’s not. It’s a minefield with a heartbeat.
Jennifer Patrician
December 5, 2025 AT 16:54They’re lying to you. All of them. Lithium? It’s not just a drug-it’s a tracking chip disguised as medicine. The FDA, the pharma giants, the psychiatrists-they all want you dependent. Why? Because blood tests cost money. Because monitoring keeps you in the system. Because if you knew how easy it is to die from a simple Advil, you’d stop trusting them.
And valproate? That’s worse. They say it causes birth defects but they don’t tell you the real reason they push it: it’s cheaper than the ‘new’ drugs. The ones with no side effects? They’re not safer. They’re just more profitable.
Carbamazepine induces enzymes? Sure. But who benefits? The labs selling the enzyme tests. The clinics charging for ‘monitoring.’ The cycle never ends. You’re not being treated. You’re being monetized.
Stop taking their pills. Go holistic. Go ketogenic. Go off-grid. The system doesn’t want you well. It wants you compliant.
Carole Nkosi
December 6, 2025 AT 00:00There’s a deeper truth here: we treat mood like a chemical equation, but the soul doesn’t balance on millimoles per liter. Lithium doesn’t stabilize emotion-it suppresses it. Valproate doesn’t cure mania-it drowns it in sedation. Carbamazepine doesn’t restore equilibrium-it rewires your biology to serve a corporate algorithm.
We’ve turned human suffering into a pharmacological spreadsheet. And we call it science.
What if the problem isn’t your brain chemistry but your life? Your isolation? Your wage slavery? Your trauma buried under five prescriptions and a 7 AM blood draw?
They want you to think the answer is in a pill. But the answer is in connection. In silence. In not being told what’s wrong with you every time you blink.
Maybe we’re not broken. Maybe we’re awake.
And they’re terrified of that.
Krishan Patel
December 6, 2025 AT 12:05Let me be perfectly clear: if you are taking any of these medications without regular therapeutic drug monitoring, you are not managing your illness-you are gambling with your neurological integrity. The data is unequivocal. Lithium toxicity is preventable. Valproate-lamotrigine interactions are documented in peer-reviewed journals since 1998. Carbamazepine-epoxide accumulation is measurable and clinically significant.
Yet I see people on Reddit casually discussing NSAIDs like they’re harmless. This is not ignorance. This is negligence. You are not a rebel. You are a statistic waiting to happen.
And for the love of all that is rational, stop conflating anecdotal experience with medical fact. One person’s ‘I felt better off carbamazepine’ does not negate 40 years of pharmacokinetic research.
Respect the science. Or die trying. Your choice.
sean whitfield
December 7, 2025 AT 09:43So let me get this straight. You take a pill that needs a blood test every 3 months just to not die from ibuprofen. And you call that treatment? Wow. What a system. We’re basically just playing Russian roulette with a lab report.
Meanwhile, the new drugs cost 10x more and don’t need blood tests. Coincidence? Or just capitalism being capitalism?
Also, why does everyone act like lithium is some ancient wisdom? It’s just the first drug they found that kinda-sorta worked. Like using a hammer to fix a watch.
And valproate causing lower IQ in kids? Cool. So now we’re poisoning the next generation to keep adults from crying in public. Real progress.
Just sayin’. We’re all just lab rats with insurance.
Stephanie Bodde
December 8, 2025 AT 14:45YOU ARE NOT ALONE 💙
I’ve been on lithium for 8 years and I used to feel so guilty when I needed help. Like I was broken. Like I was failing. But reading this? It’s like someone finally said what I’ve been screaming into the void.
Hydration. No ibuprofen. Check your levels. Write down everything you take. I do it all now. I even have a little calendar on my phone with reminders for blood tests.
And when I feel shaky or weird? I don’t panic. I check. I call my doctor. I drink water. I breathe.
You’re not weak for needing meds. You’re brave for staying alive with them.
Love you all. Keep going. You’re doing better than you think. 🌱
Philip Kristy Wijaya
December 8, 2025 AT 16:05Interesting how the entire narrative hinges on biochemical reductionism while ignoring systemic neglect. You speak of lithium levels and enzyme induction as if they are neutral facts rather than constructs of a medical industrial complex that profits from perpetual monitoring. The fact that you accept the necessity of monthly blood draws as a given reveals your complicity in the machinery. Why not ask why these drugs were ever approved without universal baseline genomic screening? Why not question why the FDA allows NSAID-lithium interactions to remain unmarked on OTC packaging? The answer is not science. It is economics. And you are feeding it.
Every time you say ‘check your levels’ you reinforce the illusion of control. There is no control. Only surveillance.
And yet I still take my lithium. Because I am a prisoner of the system. Just like you.
luke newton
December 9, 2025 AT 03:13People who take mood stabilizers are just lazy. They’d rather pop pills than fix their lives. You think your brain is broken? Maybe you just need to stop being a victim. Get a job. Move out of your parents’ basement. Stop scrolling Reddit all day. Exercise. Eat real food. Stop blaming lithium for your bad choices.
I’ve never taken a psychiatric drug in my life. I’m 42. I’ve never been hospitalized. I don’t need a blood test to know I’m not depressed. I just live right.
You want stability? Stop being a drama queen. Get off the couch. Stop complaining. The world doesn’t owe you chemical balance. You owe it to yourself to be responsible.
And if you’re pregnant and on valproate? You’re not a patient. You’re a danger to your child. And you know it.
Just sayin’. You’re not sick. You’re selfish.