Lithium Interactions: NSAIDs, Diuretics, and Dehydration Risks Explained
 Dec, 19 2025
Dec, 19 2025
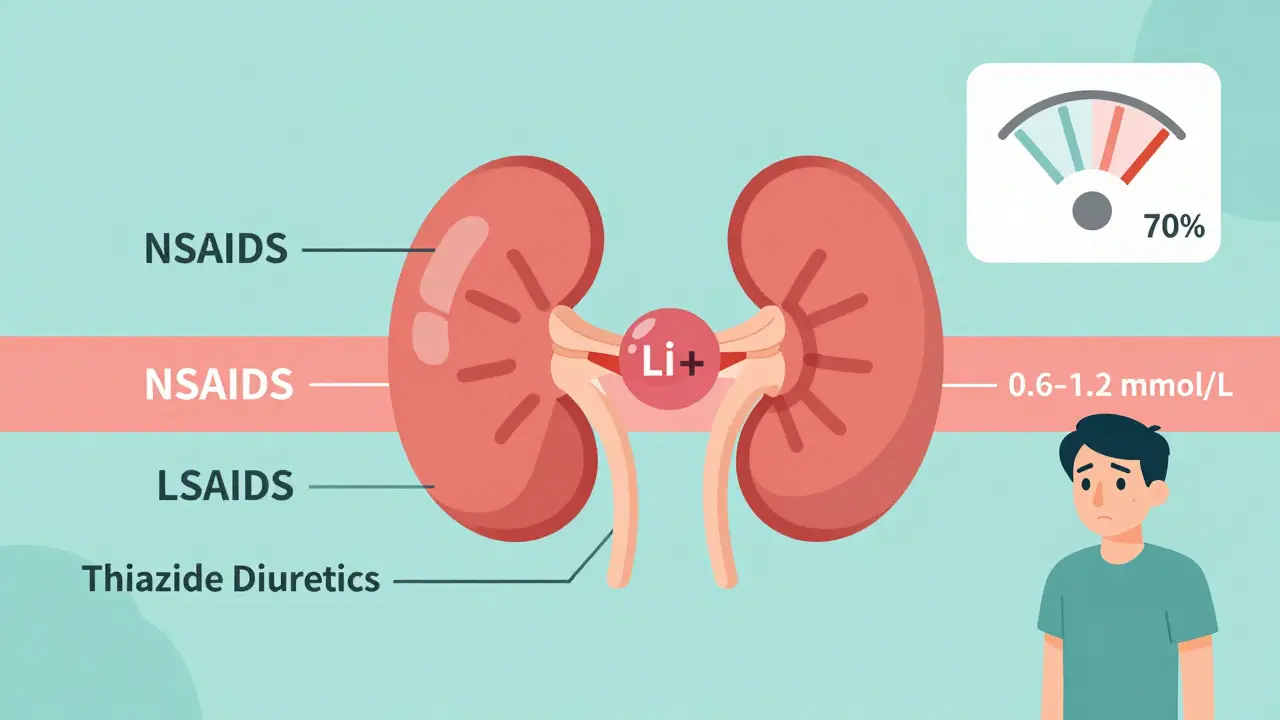
Getting prescribed lithium for bipolar disorder means you’re on a medication with very little room for error. Even small changes in your body or what you take can push lithium levels into dangerous territory. The difference between effective treatment and serious toxicity is narrow-just 0.6 to 1.2 mmol/L in your blood. That’s why knowing how NSAIDs, diuretics, and dehydration affect lithium isn’t optional. It’s life-saving.
Why Lithium Is So Sensitive
Lithium doesn’t break down in your body. About 95% of it leaves through your kidneys, unchanged. That means anything that affects how your kidneys work-like certain drugs or how much water you drink-directly changes how much lithium stays in your system. If your kidneys slow down, lithium builds up. If they flush it out too fast, your mood can become unstable. Either way, you’re at risk.This is especially true if you’re over 65, have kidney problems, heart failure, or take other medications. Older adults are 3.2 times more likely to develop lithium toxicity. It’s not just age-it’s how the body handles fluid and drugs over time.
NSAIDs: The Silent Lithium Boosters
If you’ve ever taken ibuprofen or naproxen for a headache or sore knee, you might not realize you’re putting your lithium levels at risk. Non-steroidal anti-inflammatory drugs (NSAIDs) block prostaglandins, chemicals your kidneys need to filter blood properly. When those are blocked, lithium clearance drops by 25% to 50%.Not all NSAIDs are the same. Indomethacin can spike lithium levels by up to 60%. Ibuprofen? Around 25-40%. Celecoxib is a bit gentler, but still risky. The change doesn’t happen overnight-it usually shows up within the first week of starting the NSAID. That’s why many people don’t connect their new dizziness or nausea to their painkiller.
Worse, combining NSAIDs with ACE inhibitors like cilazapril multiplies the danger. One fatal case in New Zealand involved a 72-year-old woman who took ibuprofen for joint pain while already on lithium and an ACE inhibitor. Her lithium levels rose unnoticed because monitoring was inconsistent. She died from toxicity.
Diuretics: The Big Three and Their Effects
Diuretics make you pee more. That sounds harmless, but for someone on lithium, it’s a minefield. The type of diuretic matters more than you think.Thiazides-like hydrochlorothiazide-are the worst offenders. They reduce how much lithium your kidneys flush out, causing levels to jump 25-50% within 7 to 10 days. This isn’t theoretical. Emergency rooms see this combo all the time in older patients being treated for high blood pressure.
Loop diuretics like furosemide (frusemide) are less dangerous but still risky. They can raise lithium levels by 10-25%. That might sound better, but if you’re already borderline, even a 15% rise can push you into toxicity.
Potassium-sparing diuretics like spironolactone? The data is mixed. Some studies show small increases, others show none. But because the risk isn’t zero, doctors still treat them as cautionary.
Then there are the oddballs: osmotic diuretics (like mannitol) and carbonic anhydrase inhibitors (like acetazolamide). These actually lower lithium levels by 15-30%. That’s not helpful-it’s dangerous too. If your lithium drops too low, your mood can crash. You might feel depressed, tired, or anxious. It’s the flip side of the same coin.
And don’t forget herbal diuretics. Many weight-loss teas, supplements, or “natural cleanses” contain ingredients like dandelion, parsley, or juniper. These aren’t regulated, and they can cause dangerous lithium spikes through dehydration-even if you think they’re “safe” because they’re plant-based.
Dehydration: The Hidden Trigger
You don’t need to be sick to be at risk. Even mild dehydration-losing just 2-3% of your body weight in water-can raise lithium levels by 15-25%. That’s the same as skipping a few drinks after a long walk, flying for hours, or sweating through a hot day.Traveling? If you’re flying to a hot country or spending time in the sun, your body loses more water. Diarrhea, vomiting, or fever? That’s a red flag. The NHS Borders guidelines are clear: drink plenty of fluids, especially in these situations. But most people don’t think of lithium when they’re just trying to recover from a stomach bug.
Sodium intake plays a big role too. If you suddenly cut back on salt-maybe you’re on a low-sodium diet for heart health-your lithium levels can rise by 10-20%. On the flip side, eating more salt can lower them. That’s why consistency matters. Don’t go from salty chips to a no-salt salad without telling your doctor. Small shifts add up.
What Lithium Toxicity Feels Like
Toxicity doesn’t always come with a siren. Early signs are easy to miss:- Diarrhea (68% of early cases)
- Lightheadedness or dizziness (52%)
- Drowsiness or confusion (47%)
- Tremors in your hands
- Blurred vision (31%)
- Ringing in the ears (tinnitus, 29%)
If you feel any of these and you’re on lithium, don’t wait. Don’t assume it’s just a virus or stress. Get your blood tested. Severe toxicity can lead to seizures, kidney damage, coma, or death. And here’s the scary part: kidney damage from lithium toxicity can be permanent-especially in older adults.
What You Should Do
You don’t have to give up all medications. But you need a plan.- Avoid NSAIDs if possible. Use paracetamol (acetaminophen) for pain instead. It doesn’t interfere with lithium.
- Never start a diuretic without telling your prescriber. If you’re being treated for high blood pressure or swelling, your doctor needs to know you’re on lithium. They may switch you to a safer option like an ARB or calcium channel blocker.
- Stay hydrated. Drink water consistently-not just when you’re thirsty. Aim for 1.5-2 liters a day unless your doctor says otherwise. Watch for dark urine-it’s a sign you’re not drinking enough.
- Keep your salt intake steady. Don’t go on extreme low-salt diets without supervision. Your lithium level depends on balance.
- Get your lithium levels checked regularly. After starting any new drug, your doctor should check your blood within 7-10 days. For high-risk patients, weekly checks for the first month are standard.
- Know your warning signs. If you feel off, don’t wait. Call your doctor. Bring a list of everything you’re taking, including supplements and over-the-counter meds.
When You Can’t Avoid the Risk
Sometimes, you need an NSAID for arthritis or a diuretic for heart failure. In those cases, your care team must adjust your lithium dose and monitor you closely. That means:- Lowering your lithium dose before starting the other drug
- Checking lithium levels every week for the first month
- Monitoring kidney function with blood tests
- Using the lowest effective dose of the interacting drug
- Considering a specialist referral if you’re elderly or have multiple health issues
Many electronic health systems now flag these interactions automatically. But as the Medsafe case shows, alerts aren’t enough. Human oversight still matters. You need to be your own advocate.
Final Thought: It’s Not About Fear-It’s About Control
Lithium works. It saves lives. But it’s not a medication you can take on autopilot. The risks with NSAIDs, diuretics, and dehydration are real-but they’re manageable. You don’t need to live in fear. You need to be informed.Know your numbers. Know your meds. Know your body. If you’re unsure about anything you’re taking, ask. A quick blood test can prevent a hospital trip. A simple conversation with your doctor can keep you stable and safe.
Can I take ibuprofen if I’m on lithium?
It’s not recommended. Ibuprofen can raise lithium levels by 25-40%, increasing the risk of toxicity. If you need pain relief, paracetamol (acetaminophen) is a safer choice. If you must take ibuprofen, your doctor should lower your lithium dose and check your blood levels within a week.
Do all diuretics affect lithium the same way?
No. Thiazide diuretics like hydrochlorothiazide are the most dangerous-they can spike lithium levels by 25-50%. Loop diuretics like furosemide are less risky but still need caution. Potassium-sparing diuretics have unclear effects, and osmotic or carbonic anhydrase inhibitors can actually lower lithium levels, which is also dangerous. Always check with your doctor before starting any diuretic.
How much water should I drink daily while on lithium?
Aim for 1.5 to 2 liters per day unless your doctor says otherwise. This is especially important in hot weather, after exercise, during illness, or on long flights. Dark urine or feeling thirsty are signs you’re not drinking enough. Even mild dehydration (2-3% body weight loss) can raise lithium levels by 15-25%.
Can herbal supplements interact with lithium?
Yes. Many herbal weight-loss products, teas, or cleansers contain diuretic herbs like dandelion, parsley, or juniper. These aren’t regulated and can cause dangerous lithium spikes through dehydration. Always tell your doctor about any supplements you’re taking-even if you think they’re “natural.”
What should I do if I feel dizzy or have diarrhea while on lithium?
Don’t ignore it. These are early signs of lithium toxicity. Stop taking any new medications, drink water, and contact your doctor immediately. Get a blood test to check your lithium level. Early action can prevent serious complications like seizures or kidney damage.
How often should lithium levels be checked?
When you first start lithium, levels are checked weekly until stable. After that, every 3-6 months is typical. But if you start a new drug like an NSAID or diuretic, check levels within 7-10 days and continue weekly for the first month. Elderly patients or those with kidney issues may need even more frequent monitoring.
Can lithium cause permanent kidney damage?
Yes. Severe or repeated lithium toxicity can lead to permanent kidney damage, especially in older adults or those with pre-existing kidney conditions. This is why avoiding interactions and monitoring levels closely is so critical. The damage isn’t always reversible, even after stopping lithium.
Is it safe to travel while on lithium?
Yes, but plan ahead. Heat, long flights, and illness can cause dehydration and raise lithium levels. Drink plenty of water, avoid alcohol, and carry a note from your doctor explaining your medication. If you get sick while traveling, get your lithium level checked as soon as possible.
Janelle Moore
December 20, 2025 AT 06:34Lithium is just another tool the pharmaco-corporate complex uses to keep you dependent-why do you think they don’t want you drinking more water? It’s cheaper to keep you on meds than fix your gut health. I’ve been off lithium for 3 years and my moods are better than ever. They don’t tell you about the kidney damage because they’re making billions.
Erica Vest
December 20, 2025 AT 20:33NSAIDs and lithium interactions are well-documented in clinical pharmacology literature. Thiazide diuretics reduce renal lithium clearance by inhibiting sodium reabsorption in the distal tubule, which indirectly decreases lithium excretion. The 25–50% increase in serum lithium concentration is consistent across multiple peer-reviewed studies. Always monitor levels within 7–10 days of initiating these agents.
Chris Davidson
December 21, 2025 AT 02:18People don’t read the fine print anymore. Take ibuprofen with lithium and you’re playing Russian roulette. No one blames the drug. They blame the system. But it’s simple. Don’t mix them. Period. Your doctor told you. You ignored it. Now you’re in the ER. Don’t be that person.
Glen Arreglo
December 21, 2025 AT 03:23I appreciate how thorough this is. I’ve been on lithium for 12 years and I never realized how much dehydration could affect me. I used to skip water when I traveled. Now I carry a bottle everywhere-even on short flights. Small changes matter. Thanks for the clarity.
Ashley Bliss
December 22, 2025 AT 09:42This isn’t just about medication-it’s about control. The system wants you afraid. It wants you to believe you’re broken and need chemicals to survive. But what if your sadness isn’t a disorder? What if it’s a response to a world that’s collapsing? Lithium silences the scream. But maybe the scream is the only thing keeping you human.
I’m not saying stop the meds. I’m saying ask why you’re on them in the first place. Who decided your pain needed fixing? Not you. Not your soul. Someone in a lab coat with a profit margin.
Allison Pannabekcer
December 24, 2025 AT 04:39I’m so glad someone finally explained this in plain language. My mom is on lithium and was prescribed hydrochlorothiazide for her blood pressure. No one warned her. She ended up in the hospital with tremors and confusion. It took weeks to stabilize. Please, if you’re on lithium, keep a list of every pill-even the ones from the grocery store. And tell your doctor about every herbal tea you drink. They’re not just harmless ‘natural’ things-they’re pharmacologically active.
Sarah McQuillan
December 25, 2025 AT 01:15Actually, in Sweden they use way less lithium because they focus on therapy and social support. America just druggifies everything. You think this is science? It’s capitalism with a stethoscope. Why not fix housing, food, and loneliness instead of dosing people into compliance? We’re treating symptoms of a broken society like they’re individual medical failures.
Henry Marcus
December 26, 2025 AT 19:21Did you know? NSAIDs don’t just affect lithium-they’re part of a secret government program to monitor kidney function via pharmaceutical telemetry! The pills have microchips embedded in the coating that send data to the FDA through your urine! That’s why they push hydration-it’s to dilute the signal! And don’t get me started on the diuretics-they’re designed to trigger false positives in lithium tests so they can justify higher doses! You’re being watched. Always.
Frank Drewery
December 26, 2025 AT 21:25This is exactly the kind of info I wish I’d had when I started lithium. I felt so alone. I thought I was the only one scared to take a painkiller. Thank you for laying it out so clearly. You’re not just saving lives-you’re giving people peace of mind.
Danielle Stewart
December 27, 2025 AT 21:59Thank you for writing this. I’m a nurse and I see this every week. One patient came in with lithium toxicity after taking Advil for a week. She didn’t know it was dangerous. We need more posts like this. Please keep sharing. And if you’re reading this-don’t wait for a crisis. Talk to your doctor. Write down your meds. Drink water. You’ve got this.