How Year-Round Allergies Trigger Ear Infections
 Sep, 30 2025
Sep, 30 2025
Allergy vs. Ear Infection Quiz
This quiz helps determine whether your ear discomfort could be linked to year-round allergies rather than a typical ear infection.
1. Do you experience persistent nasal congestion or runny nose throughout the year?
2. Have you noticed increased ear fullness or pressure without fever?
3. Is there a history of seasonal allergies or exposure to indoor allergens like dust mites or pet dander?
4. Do you frequently experience itchy eyes or throat along with nasal symptoms?
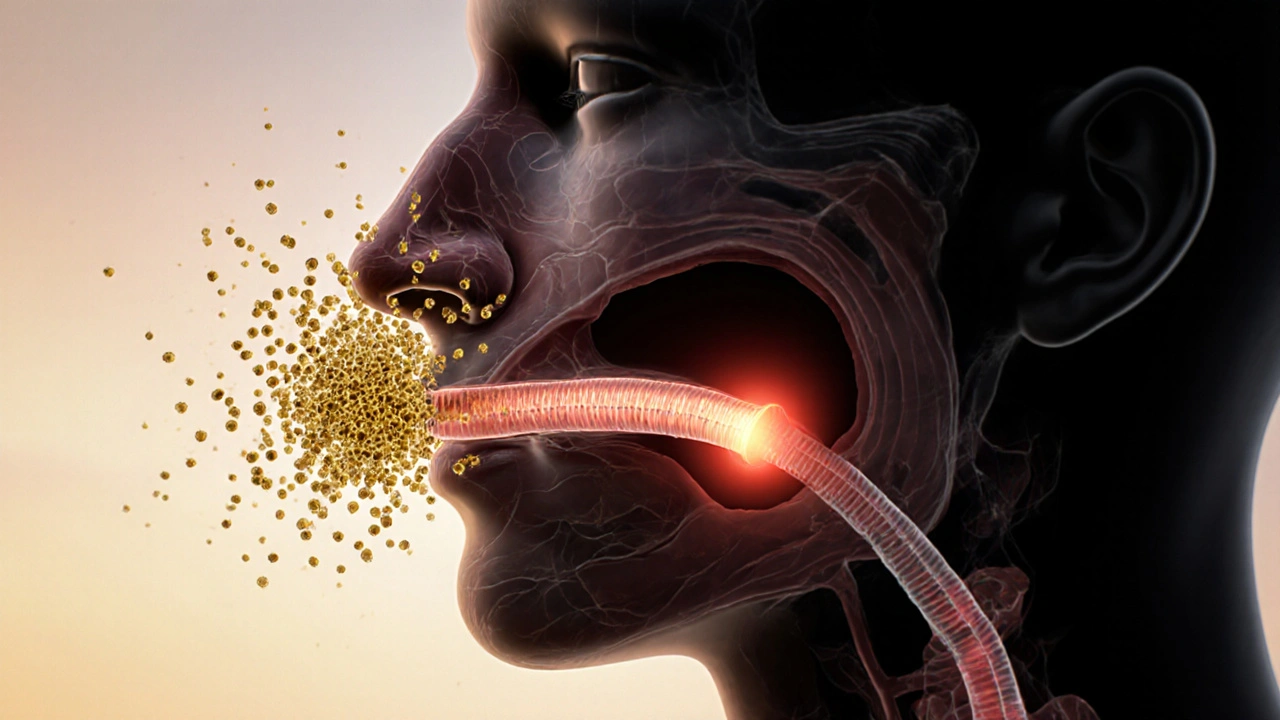
Ever wonder why you’re constantly reaching for a tissue and then, a few days later, your child’s ear starts hurting? The culprit is often the same invisible irritant that’s causing your sniffles. When nasal passages stay inflamed for months on end, the tiny tube that equalizes pressure in the ear can get clogged, paving the way for an infection. Below we’ll break down how year-round allergies set the stage for ear problems, what the warning signs are, and how you can keep both issues at bay.
Quick Take
- Allergic rhinitis keeps nasal tissue swollen, which blocks the Eustachian tube.
- Blocked tubes trap fluid, creating a perfect environment for Otitis Media (middle‑ear infection).
- Histamine spikes increase mucus production and worsen tube pressure.
- Managing allergies with nasal sprays, antihistamines, and allergy shots can cut ear‑infection risk by up to 40%.
- Seek medical care if ear pain lasts more than 48hours, you have fever, or fluid drainage appears.
What Are Year‑Round Allergies?
When most people think of allergies, they picture spring pollen or summer grass. Allergic Rhinitis (persistent inflammation of the nasal lining caused by allergens like dust mites, pet dander, or mold spores) is the medical term for those sneezing, itchy‑eye bouts that never seem to end. Unlike seasonal allergies that flare only a few months a year, this form sticks around all year, keeping the nasal passages in a constant state of irritation.
The immune system releases Histamine (a chemical that triggers itching, swelling, and mucus production) every time an allergen is detected. Histamine makes blood vessels leaky, leads to swelling of the nasal lining, and ramps up mucus output. Over time, the chronic swelling narrows the opening of the Eustachian Tube (the narrow canal that links the middle ear to the back of the throat), which is vital for equalizing pressure and draining fluid from the middle ear.
How Ear Infections Develop
Otitis Media (infection of the space behind the eardrum) usually starts when fluid builds up behind the eardrum and bacteria or viruses seize the opportunity to multiply. In healthy ears, the Eustachian tube opens briefly when you swallow or yawn, letting air in and liquid out. If that tube is blocked, fluid stays trapped, creating a warm, moist pocket-exactly what germs love.
When the fluid becomes infected, you’ll notice ear pain, a feeling of fullness, sometimes fever, and in children, tugging at the ear. Untreated, the infection can spread, cause hearing loss, or lead to more serious complications like mastoiditis.
The Biological Bridge: From Allergies to Ear Infection
Three key processes link allergic rhinitis to otitis media:
- Swelling of the nasal mucosa - Chronic exposure to allergens inflames the lining of the nose and nasopharynx. This swelling extends to the opening of the Eustachian tube, narrowing it.
- Increased mucus and histamine - Histamine prompts excess mucus that can spill into the tube. The sticky mucus further blocks airflow.
- Reduced immune clearance - The inflamed tissue hampers the ear’s natural ability to clear pathogens, letting bacteria take hold.
Research from the Australian Institute of Health (2023) showed that children with diagnosed perennial allergic rhinitis were 1.8times more likely to develop recurring middle‑ear infections than their non‑allergic peers. Adults aren’t immune either; a 2022 meta‑analysis found that 45% of adults with chronic sinusitis (often allergy‑driven) reported at least one ear infection in the past year.

Who’s Most at Risk?
The risk profile isn’t uniform. Here’s who should keep a closer eye on the connection:
- Kids under 7 - Their Eustachian tubes are shorter and more horizontal, making blockage easier.
- People with indoor allergens - Dust‑mite infestations, pet dander, or mold in homes amplify year‑round exposure.
- Smokers and those exposed to secondhand smoke - Smoke irritates the airway, worsening both allergy and tube function.
- Individuals with structural nasal issues - Deviated septum or enlarged adenoids can compound the blockage.
Prevention & Management Strategies
Stopping the cycle early can keep your ears clear. Below are practical steps backed by clinical guidelines:
- Allergen control: Use HEPA filters, wash bedding in hot water weekly, and keep humidity below 50% to deter dust mites.
- Medicated nasal sprays: Nasal Corticosteroid Spray (anti‑inflammatory spray that reduces nasal swelling) is first‑line for persistent rhinitis. Use as directed for 2‑4weeks before expecting relief.
- Antihistamines: Oral agents like cetirizine block histamine receptors, lowering mucus production.
- Allergy immunotherapy: For those who can’t avoid triggers, a series of allergy shots or sublingual tablets can modify the immune response over time, cutting infection rates.
- Jaw‑opening exercises: Simple yawning or chewing gum encourages the Eustachian tube to open, especially during colds.
- Stay hydrated: Thin mucus is easier to clear, reducing blockage risk.
When an ear infection does occur, doctors may prescribe a short course of antibiotics if bacterial involvement is likely, but they’ll also address the underlying allergy to prevent recurrence.
Signs It’s More Than a Cold
Distinguishing an allergic flare from an emerging ear infection can be tricky. Look for these red flags:
- Sharp, throbbing pain that doesn’t improve with decongestants.
- Fever over 38°C (100.4°F) lasting more than 24hours.
- Fluid draining from the ear (clear or pus‑colored).
- Sudden hearing loss or a “plugged” sensation.
If any of these appear, book an appointment. Prompt treatment can prevent fluid from hardening into a chronic condition called otitis media with effusion.
Quick Comparison: Allergy vs. Ear Infection Symptoms
| Symptom | Allergic Rhinitis | Otitis Media |
|---|---|---|
| Nasality | Runny or stuffy nose, post‑nasal drip | Often present if infection follows a cold |
| Ear pain | Rare, usually mild pressure | Sharp, throbbing, may worsen at night |
| Fever | Uncommon | Common, especially in children |
| Itching | Eyelids, throat, ears | Absent |
| Hearing loss | Usually none | Temporary muffled hearing due to fluid |
Next Steps if You Suspect a Link
1. Track your symptoms. Keep a simple diary noting allergy triggers, nasal spray usage, and any ear discomfort.
2. Schedule an ENT or allergist visit. Bring your diary; it helps clinicians pinpoint the cause.
3. Ask about a referral for allergy testing (skin prick or blood IgE panel) to identify specific indoor allergens.
4. Follow a treatment plan that tackles both the nose and the ear-often a combination of nasal steroids and a short‑term antibiotic if an infection is confirmed.
5. Review your environment. Replace carpets, wash curtains, and use dust‑mite‑proof pillowcases.

Frequently Asked Questions
Can allergies cause ear infections in adults?
Yes. While children are more prone because of their anatomy, adults with chronic allergic rhinitis can develop middle‑ear fluid buildup that leads to infection, especially if they have sinus congestion or smoke.
Do antihistamines help prevent ear infections?
Antihistamines reduce mucus production and can keep the Eustachian tube clearer, lowering infection risk. They work best when combined with a nasal corticosteroid for inflammation control.
How long should I use nasal steroids before seeing results?
Most patients notice reduced congestion within 2-4weeks, but full anti‑inflammatory benefits can take up to 6weeks. Consistency is key; skipping doses slows improvement.
Is ear tube surgery an option for allergy‑related infections?
Ventilation tubes can help children with recurrent infections, but they don’t treat the underlying allergy. Doctors usually recommend addressing the allergen first; tubes become necessary only when infections persist despite optimal allergy management.
What home remedies can I try while waiting for a doctor’s appointment?
Warm compresses over the ear, steam inhalation to loosen mucus, and gentle jaw‑opening exercises (yawning or chewing gum) may relieve pressure. Keep your head elevated while sleeping to encourage drainage.
Landmark Apostolic Church
September 30, 2025 AT 12:41Allergies are the silent culprits behind most ear aches.
Matthew Moss
October 2, 2025 AT 20:14It is incumbent upon us, as responsible citizens, to recognize that chronic allergic rhinitis is not merely a nuisance but a genuine health hazard that predisposes individuals to otitis media. The persistent inflammation of the nasal mucosa creates a cascade of physiological events that ultimately impair the function of the Eustachian tube. Consequently, the middle ear becomes a breeding ground for pathogens. One cannot dismiss the data from recent epidemiological studies which demonstrate a clear correlation between year‑round allergen exposure and increased incidence of ear infections. Therefore, proactive management of indoor allergens, alongside appropriate pharmacotherapy, is essential to mitigate this risk.
Antonio Estrada
October 5, 2025 AT 03:48I totally agree that keeping the indoor environment clean can make a real difference. Simple steps like washing bedding in hot water weekly, using HEPA filters, and maintaining low humidity can reduce dust‑mite loads. When the nasal passages stay less inflamed, the Eustachian tube is less likely to get clogged, which means fewer ear infections for both kids and adults.
Andy Jones
October 6, 2025 AT 21:28Oh sure, because everyone’s got a PhD in immunology and can instantly tell you the exact mechanism by which histamine blocks the Eustachian tube. It’s not like the article already laid that out in plain English. Maybe next time you’ll add a diagram with arrows and glitter.
Kevin Huckaby
October 9, 2025 AT 05:01Yo, the whole "just use a nasal spray" thing is oversimplified 🌪️. If you’ve got mold spores thriving behind your walls, no amount of antihistamine will fix that. You need a full‑blown remediation plan, folks-air purifiers, de‑humidifiers, and maybe a professional inspection.
Brandon McInnis
October 10, 2025 AT 22:41While I understand the urgency, let’s keep the conversation respectful. Managing allergies does require a balanced approach-pharmacologic treatment paired with environmental control. Over‑the‑top claims can scare people away from seeking proper medical advice.
Aaron Miller
October 13, 2025 AT 06:14In truth, the elite medical discourse often glosses over the socioeconomic dimensions of allergy‑related ear infections-namely, the fact that low‑income families are disproportionately affected due to substandard housing conditions; consequently, any comprehensive solution must address both clinical and environmental justice concerns!!!
Roshin Ramakrishnan
October 14, 2025 AT 23:54Indeed, the intersection of housing quality and health outcomes cannot be ignored; mitigation strategies should include community‑level interventions such as subsidized remediation programs, tenant education, and stricter building codes to reduce indoor allergen loads.
Todd Peeples
October 17, 2025 AT 07:28From a pathophysiological standpoint, the chronic up‑regulation of Th2 cytokines in perennial allergic rhinitis perpetuates mucosal edema, thereby compromising the patency of the cartilaginous portion of the Eustachian tube. This mechanistic insight underscores the rationale for employing intranasal corticosteroids as a first‑line anti‑inflammatory agent.
Chris Smith
October 19, 2025 AT 15:01Wow, look who's trying to sound smart. News flash: not everyone has a chemistry degree, so keep it simple.
Leonard Greenhall
October 21, 2025 AT 08:41The article's data aligns with meta‑analyses showing a 45% comorbidity rate between chronic sinusitis and otitis media, indicating that the link is statistically significant and not merely anecdotal.
Abigail Brown
October 23, 2025 AT 16:14Reading through this, I couldn't help but feel a surge of hope mixed with a dash of urgency. Imagine a world where we treat the root cause-those sneaky indoor allergens-before they spiral into full‑blown ear infections. First, we must become detectives in our own homes, tracking down the hidden dust‑mites, the silent mold colonies, the tiniest strands of pet dander that flutter in the air like invisible confetti. When we spot these culprits, we take action: washing bedding in water hotter than a summer sidewalk, vacuuming with HEPA‑equipped machines, and ensuring humidity never climbs above fifty percent. Next, we embrace the power of modern medicine-nasal corticosteroid sprays that soothe inflamed mucosa, antihistamines that calm the histamine storm, and, for the brave, immunotherapy that re‑educates the immune system over months. Yet, science alone isn’t enough; lifestyle habits matter. Staying hydrated keeps mucus thin, yawning and chewing gum keep the Eustachian tube yawning open, and avoiding secondhand smoke stops further irritation. For families with children, regular ear checks become a ritual, catching fluid buildup before it seals the door on hearing. In the grand tapestry of health, each thread-environment, medication, habit-intertwines, creating a safety net that catches the ear before it falls prey to infection. So, let us not dismiss these simple steps as mundane chores; they are indeed the frontline soldiers in a battle that protects our ability to hear, talk, and connect. And when the battle does flare, prompt medical attention-whether antibiotics for a bacterial invasion or ENT referral for chronic issues-can turn a potential disaster into a manageable episode. Remember, the goal isn’t just to treat symptoms, but to rewrite the narrative from chronic misery to resilient wellness.
Crystal Slininger
October 25, 2025 AT 09:54While the optimism is refreshing, let’s not ignore the possibility that pharmaceutical companies might be downplaying the role of environmental toxins to push meds. Some of the “standard” treatments could be part of a larger agenda to keep us dependent on prescriptions.
Camille Ramsey
October 27, 2025 AT 16:28Honestly, the whole “just sniff some spray” line is a lazy excuse for not addressing real air quality problems. Get your facts straight and stop feeding the pharma machine.
Ben Poulson
October 30, 2025 AT 00:01Thank you for this thorough overview; the integration of environmental and pharmacologic strategies is commendable.
Raghav Narayan
October 31, 2025 AT 17:41It is my pleasure to expand upon the points raised. In practice, successful management often begins with a detailed environmental audit-identifying sources of dust mites, pet dander, and mold, followed by targeted interventions such as encasing mattresses, employing UV air purifiers, and maintaining indoor humidity below 45%. Concurrently, a stepped‑care pharmacologic regimen, beginning with a intranasal corticosteroid for anti‑inflammatory effect, supplemented by an oral antihistamine as needed, yields the best outcomes. Moreover, patient education on techniques to equalize middle‑ear pressure-like the Valsalva maneuver and regular chewing-further reduces infection risk. Regular follow‑up appointments enable clinicians to adjust therapy based on symptom progression, ensuring that both the allergic component and any emergent otologic issues are addressed promptly.
Tara Phillips
November 3, 2025 AT 01:14In light of the evidence presented, let us strive for comprehensive care that tackles both allergen exposure and ear health.
Jarrod Benson
November 5, 2025 AT 08:48Yo, this info is solid-definitely gonna start checking my bedroom for dust and maybe grab an air purifier. Also, gonna talk to my doc about trying a nasal spray before the next cold hits.
Liz .
November 7, 2025 AT 02:28Great rundown! i'm gonna share this with my fam so we can all stay ahead of those pesky ear infections.