GLP-1 Agonists for Weight Loss: Real Benefits and Common Side Effects
 Feb, 11 2026
Feb, 11 2026
When you hear about GLP-1 agonists, you might think of celebrity weight loss stories or viral TikTok videos. But behind the hype are real science, measurable results, and real risks. These aren’t magic pills. They’re powerful medications that change how your body handles hunger, food, and fat - and they come with trade-offs most people don’t talk about.
How GLP-1 Agonists Actually Work
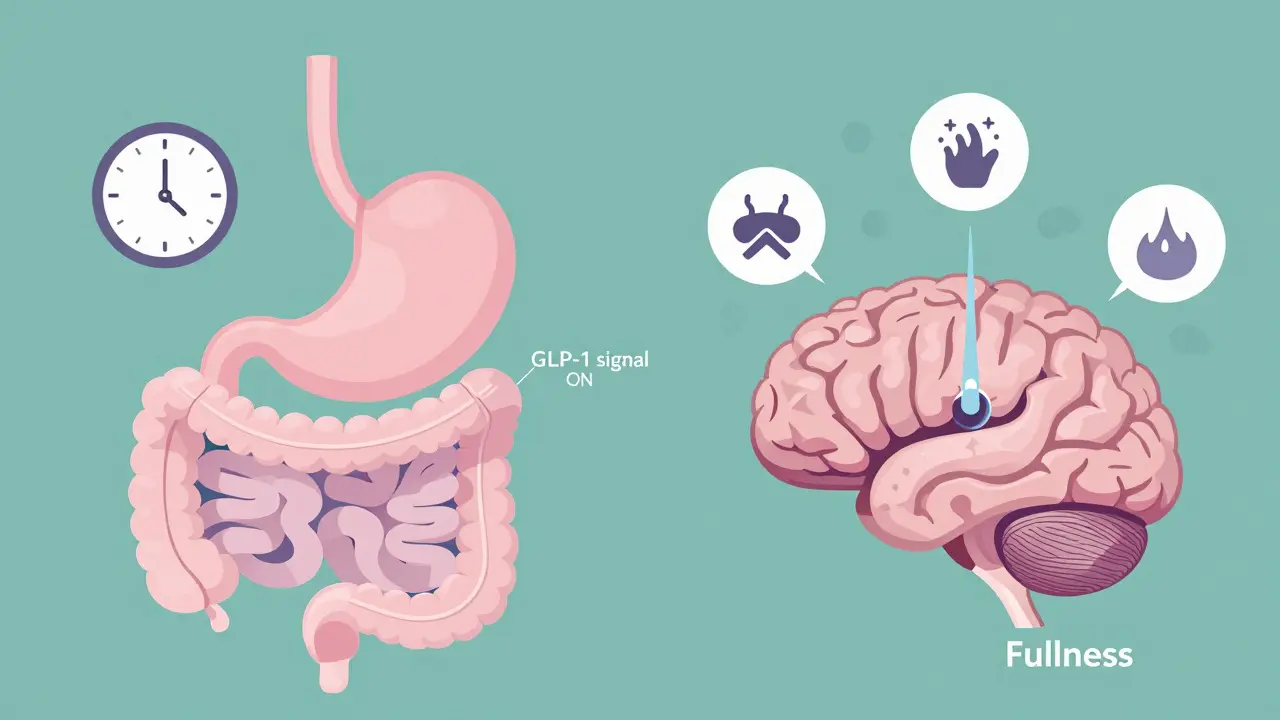
GLP-1 agonists mimic a natural hormone your gut makes after you eat. That hormone, called glucagon-like peptide-1, tells your brain you’re full, slows down how fast your stomach empties, and helps your pancreas release insulin when blood sugar rises. But in people with obesity or type 2 diabetes, this system doesn’t work well. GLP-1 agonists step in to fix that.
Think of them like a volume knob for fullness. They turn up the signal so you feel satisfied with less food. You don’t feel hungry between meals. You don’t crave snacks. You stop eating earlier because your brain finally gets the message: you’ve had enough.
The most common ones are semaglutide (Wegovy, Ozempic), liraglutide (Saxenda), and tirzepatide (Zepbound, Mounjaro). Semaglutide and liraglutide are versions of the natural hormone, tweaked so they last longer in your body. Tirzepatide does something even smarter - it hits two targets at once: GLP-1 and another hormone called GIP. That’s why it often leads to more weight loss.
How Much Weight Can You Really Lose?
Let’s cut through the noise. Clinical trials show consistent results. On semaglutide (Wegovy), people lost an average of 15.8% of their body weight over 68 weeks. That’s not 5 pounds. That’s 30 pounds for someone who weighs 200. Tirzepatide? Up to 20.9% in the same timeframe. For comparison, older weight loss drugs like orlistat or phentermine-topiramate usually deliver 5-10%.
Here’s what that looks like in real life: In the STEP 4 trial, over half of people on semaglutide lost 15% or more of their weight. Only 5% of those on placebo did. That’s not a small difference. That’s life-changing. People report not just losing weight, but feeling like they can finally control their eating. One user on Reddit said, “I used to eat a whole pizza by myself. Now I stop after two slices - not because I’m trying, but because I just don’t want more.”
It’s not just about the scale. These drugs also lower blood sugar, reduce blood pressure, and improve cholesterol. In the SUSTAIN-6 trial, semaglutide cut major heart events by 26%. That’s why doctors now recommend them not just for weight, but for people with diabetes and heart disease.
The Side Effects You Can’t Ignore
Here’s the catch: most people experience side effects - and they’re not mild. Around 70-80% of users get nausea, especially in the first few weeks. About 50-60% get diarrhea. 40-50% throw up. 30-40% have stomach pain. These aren’t rare. They’re expected.
One woman in Melbourne shared her story: “Weeks 3 to 8 were hell. I was nauseous every morning. I couldn’t eat anything without feeling sick. I almost quit. But then, after I got to the 1.7 mg dose, it just… stopped. I didn’t even notice it was gone until I looked back.”
The key? Slow titration. Doctors start you at 0.25 mg once a week and slowly increase every month. Rushing the dose makes side effects worse. Waiting 4-6 weeks between increases lets your body adjust. Most people say the nausea fades after 8-12 weeks.
Other risks include gallbladder problems, low blood sugar (especially if you’re also on insulin or sulfonylureas), and rare but serious concerns like pancreatitis or gallstones. There’s also a black box warning from the FDA about thyroid tumors - seen in rats, not yet confirmed in humans. If you or a close family member has ever had medullary thyroid cancer or multiple endocrine neoplasia, you shouldn’t use these drugs.
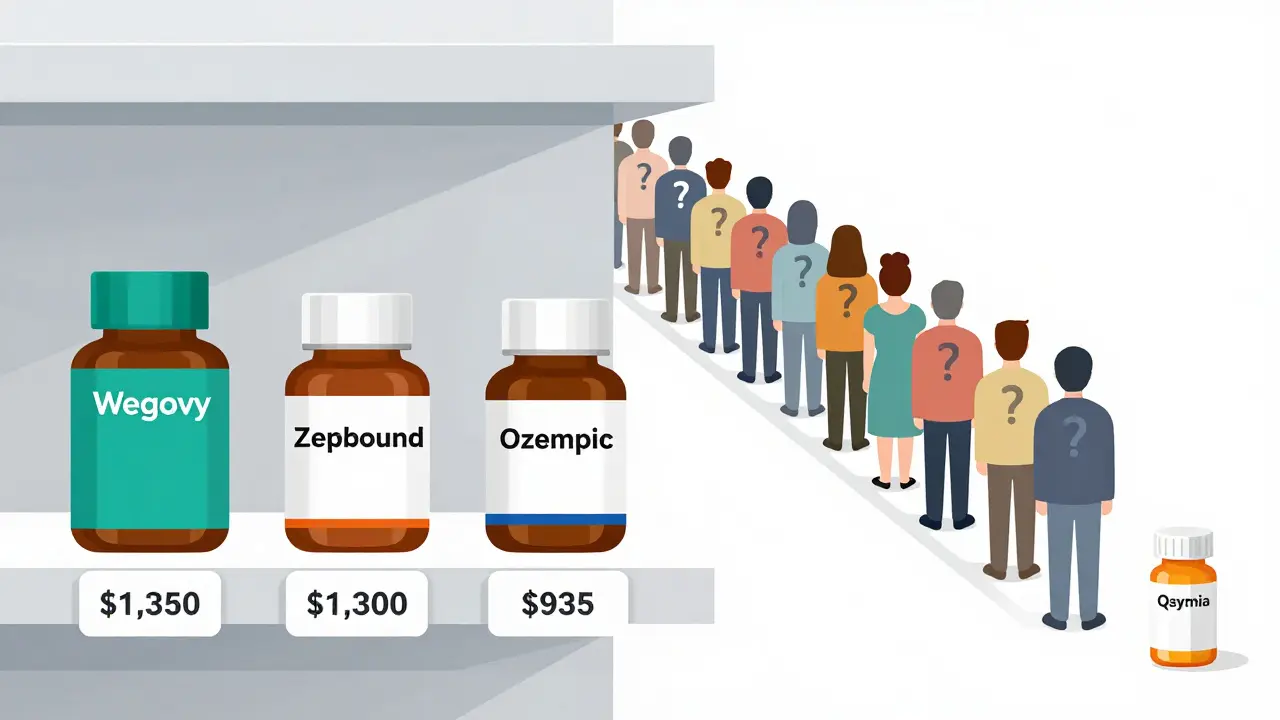
Cost and Access: The Hidden Barrier
Wegovy costs about $1,350 a month in the U.S. without insurance. Ozempic (the same drug for diabetes) is cheaper at $935, but you can’t legally use it for weight loss unless your doctor prescribes it off-label. In Australia, it’s even harder to get - most private insurers don’t cover it for obesity. Public healthcare? Almost never.
Only 37% of U.S. commercial insurance plans cover Wegovy for weight loss as of 2023. Compare that to 89% coverage for diabetes. That means people with a BMI over 30 - who meet medical guidelines - still can’t get it because their plan says “no.”
And it’s not just cost. There’s a global shortage. Novo Nordisk, the maker of Wegovy and Ozempic, reported 18-month backorders in late 2023. Clinics are rationing doses. Patients are being put on waitlists. If you’re hoping to start soon, be prepared for delays.
What Happens When You Stop?
This is the part no one wants to talk about. If you stop taking the drug, you will regain weight. Studies show most people gain back 50-70% of the lost weight within a year of stopping.
In the STEP 4 trial, people who stopped semaglutide after 68 weeks regained an average of 11.6% of their body weight over the next 60 weeks. That’s more than half the weight they lost. It’s not failure. It’s biology. Your body fights to return to its old set point. Without the drug, hunger returns. Cravings come back. The brain doesn’t remember how to feel full.
That’s why experts say these aren’t short-term fixes. They’re long-term treatments - like blood pressure or cholesterol meds. You don’t stop taking statins after six months. You don’t stop insulin. You keep going. And if you can’t afford it or access it long-term, the benefits vanish.
How It Compares to Other Weight Loss Drugs
| Medication | Typical Weight Loss | Dosing | Common Side Effects | Cost (Monthly, USD) |
|---|---|---|---|---|
| Semaglutide (Wegovy) | 15.8% | Weekly injection | Nausea, diarrhea, vomiting | $1,349 |
| Tirzepatide (Zepbound) | 20.9% | Weekly injection | Nausea, diarrhea, constipation | $1,300-$1,400 |
| Liraglutide (Saxenda) | 6.4% | Daily injection | Nausea, constipation | $1,000-$1,200 |
| Phentermine-Topiramate (Qsymia) | 7-10% | Daily pill | Cognitive fog, dry mouth, tingling | $150-$200 |
| Orlistat (Xenical) | 5-10% | Daily pill | Oily stools, frequent bowel movements | $100-$150 |
Notice something? The most effective drugs are injections. The cheapest are pills. But the pills come with their own problems - brain fog, dry mouth, or embarrassing bowel issues. And none of them match the metabolic benefits of GLP-1 agonists.
What You Need to Do Before Starting
Don’t just ask your doctor for a prescription. Ask these questions:
- Do I have a personal or family history of medullary thyroid cancer or MEN2? (If yes, don’t use it.)
- Am I pregnant or planning to get pregnant? (These drugs aren’t safe during pregnancy.)
- Can I afford this long-term? (What happens if insurance drops coverage?)
- Am I ready to stick with it for years? (Weight comes back if you stop.)
- Can I tolerate nausea and stomach issues for 2-3 months?
Also, don’t expect miracles without lifestyle changes. These drugs work best with a modest calorie deficit - around 500 fewer calories a day. You still need to eat balanced meals. You still need to move. The drug doesn’t replace behavior. It just makes it easier.
The Future: What’s Next?
Oral versions are coming. Novo Nordisk is testing an oral semaglutide for weight loss - if it works, it could change everything. Pfizer has a similar pill in phase 2 trials. If you hate needles, that’s huge news.
Also, more insurance coverage is likely. As data piles up showing heart benefits, insurers may start paying. In Australia, the PBS (Pharmaceutical Benefits Scheme) is reviewing Wegovy for obesity - no decision yet, but pressure is growing.
For now, GLP-1 agonists are the most effective weight loss drugs we’ve ever had. They’re not perfect. They’re not cheap. They’re not easy. But for people struggling with obesity, they offer something no diet ever could: real, lasting, measurable change.
Can GLP-1 agonists be used long-term?
Yes, they’re designed for long-term use. Obesity is a chronic condition, and these drugs work like blood pressure or cholesterol meds - they manage the condition but don’t cure it. Stopping usually leads to 50-70% weight regain. Doctors recommend continuing treatment indefinitely if it’s working and tolerated.
Is Wegovy better than Ozempic for weight loss?
Wegovy and Ozempic contain the same drug - semaglutide - but at different doses. Wegovy is approved for weight loss at 2.4 mg weekly. Ozempic is approved for diabetes at 1 mg or 0.5 mg. Doctors sometimes prescribe Ozempic off-label at higher doses for weight loss, but it’s not officially approved for that. Wegovy is the only version legally labeled for chronic weight management.
Do GLP-1 agonists cause muscle loss?
Some weight loss from these drugs includes muscle, but studies show they preserve more muscle than traditional diets. In clinical trials, about 30-40% of weight lost was fat mass, and the rest was water and some lean mass. Combining the drug with resistance training and adequate protein intake helps protect muscle. It’s not perfect, but better than dieting alone.
Why do GLP-1 agonists cause nausea?
They slow gastric emptying - meaning food stays in your stomach longer. That’s good for fullness, but it can cause nausea, bloating, and vomiting. The effect is strongest when you start or increase the dose. Most people adapt within 8-12 weeks. Eating smaller, low-fat meals and staying hydrated helps reduce symptoms.
Are there alternatives if I can’t afford GLP-1 agonists?
Yes, but none match their effectiveness. Phentermine-topiramate (Qsymia) is cheaper and oral, but carries risks like cognitive side effects and birth defects. Orlistat (Xenical) is available over-the-counter, but causes oily stools and only helps with 5-10% weight loss. Lifestyle changes - diet, sleep, stress management, and movement - remain the foundation. Medication helps, but doesn’t replace them.
If you’re considering GLP-1 agonists, talk to a specialist - not just your GP. Endocrinologists, obesity medicine doctors, or bariatric clinics have the most experience. Don’t rush. Don’t compare your journey to someone else’s. This isn’t a quick fix. It’s a tool. Use it wisely.
Jim Johnson
February 13, 2026 AT 02:49Man, I started Wegovy last year and holy crap, the nausea hit me like a truck. First two weeks I was basically just lying on the couch, sipping ginger tea and crying. But after week 6? Magic. I went from eating 3 meals + 2 snacks to just 2 meals and feeling full. Lost 42 lbs. No magic, just biology. Still take it every week. Worth it.
Jonathan Noe
February 13, 2026 AT 16:31Everyone’s acting like GLP-1s are some revolutionary breakthrough. Newsflash: we’ve had appetite suppressants for decades. The only difference now is Big Pharma finally found a way to charge $1,300/month for something that just makes you feel sick while you eat less. Same old scam, new injection pen.
Luke Trouten
February 15, 2026 AT 07:43It’s fascinating how we’ve reduced a complex metabolic condition to a single pharmacological solution. Obesity isn’t simply a matter of appetite regulation-it’s a symphony of hormonal, psychological, environmental, and socioeconomic factors. To treat it as if a weekly injection is the answer is dangerously reductive. The real issue is food deserts, chronic stress, sleep deprivation, and the normalization of hyper-palatable foods. Medication helps, yes-but only if we stop pretending it fixes the root causes.
Kristin Jarecki
February 17, 2026 AT 00:25As a registered dietitian with over 12 years in clinical obesity management, I want to emphasize that GLP-1 agonists are not substitutes for nutritional counseling or behavioral therapy. They are adjuncts. Patients who combine them with structured meal planning, protein prioritization, and resistance training retain significantly more lean mass and experience better long-term outcomes. The drug opens the door-but lifestyle determines whether you walk through and stay.
Skilken Awe
February 17, 2026 AT 05:26Oh wow, so now we’re telling people to just accept lifelong injections because their bodies are ‘broken’? Meanwhile, Big Pharma is quietly lobbying to remove all non-pharmaceutical weight loss coverage from Medicare. This isn’t medicine. It’s a subscription model disguised as healthcare. And don’t get me started on the shortage-manufacturers are artificially limiting supply to jack up prices. Classic capitalism.
Ernie Simsek
February 19, 2026 AT 03:23Just dropped 35 lbs on tirzepatide. My knees don’t crack anymore. I can fit in airplane seats. My wife says I look like a different person. 🤯 Also, nausea lasted 3 weeks. Now I just feel… calm. Like my brain finally stopped screaming for carbs. Worth every penny. Even if I have to sell my Tesla to afford it next year.
Sonja Stoces
February 20, 2026 AT 19:33Wait, so you’re seriously saying people who gain weight back after stopping are ‘failing’? That’s not biology-that’s punishment. Why isn’t anyone talking about how we demonize fat people and then act shocked when they can’t maintain a drug they can’t afford? This isn’t treatment. It’s conditional acceptance. You lose weight? You’re worthy. You gain it back? You’re lazy. Toxic.
Steve DESTIVELLE
February 21, 2026 AT 02:16The truth is simple. The body is not a machine. It is a living organism shaped by centuries of evolution. When we force it into submission with synthetic hormones we do not understand fully we create new imbalances. The nausea is not a side effect. It is the body screaming. The weight regain is not failure. It is wisdom. Nature remembers. We forget. We are not meant to be forever dependent on pharmaceuticals to eat less. We are meant to live in harmony with our instincts. But capitalism has replaced instinct with algorithms. And now we pay for our disconnection with monthly injections.
Neha Motiwala
February 21, 2026 AT 17:51Did you know that the FDA approved these drugs based on studies where participants were mostly white, middle-class, college-educated people? What about the 40% of Americans who work two jobs, can’t afford healthy food, and have zero access to specialists? This isn’t a solution. It’s a privilege. And now they’re trying to make it a requirement for insurance to cover diabetes care unless you’re on GLP-1s? This is eugenics with a prescription pad.
Jack Havard
February 22, 2026 AT 10:5915.8% weight loss? That’s a 300-lb person losing 47 lbs. But what about the 70% who lose less than 10%? Or the 20% who drop out because they can’t tolerate nausea? The headline numbers are cherry-picked. And don’t get me started on the ‘heart benefits’-those trials were funded by Novo Nordisk. Conflict of interest much?
Autumn Frankart
February 22, 2026 AT 19:38GLP-1s are just the beginning. Next they’ll inject microchips into the drugs to track your eating habits. Then insurance companies will penalize you if you eat carbs. Then the government will require a BMI scan before you can buy groceries. This is how they control the population. You think this is about health? It’s about control. Wake up.
Joanne Tan
February 24, 2026 AT 19:08Just wanna say to anyone scared to start this: you’re not weak for needing help. I was terrified of needles. I cried the first time I injected. But now? I feel like myself for the first time since I was 18. The nausea sucked. The waiting sucked. But the result? Worth it. You got this. 💪