Folic Acid and Prenatal Vitamins: What You Need to Know About Medication Interactions in Pregnancy
 Nov, 19 2025
Nov, 19 2025
When you’re pregnant, taking folic acid isn’t just a suggestion-it’s a medical necessity. But what most women don’t realize is that folic acid doesn’t play nice with every medication. Even something as simple as a prenatal vitamin can become risky if you’re also taking epilepsy drugs, antibiotics, or even common acid reducers. The stakes are high: neural tube defects like spina bifida develop in the first 28 days after conception-often before a woman even knows she’s pregnant. Getting the right dose of folic acid isn’t just about popping a pill. It’s about timing, absorption, and knowing what to avoid.
Why Folic Acid Matters So Much in Early Pregnancy
Folic acid, the synthetic form of vitamin B9, is the only nutrient proven to prevent serious birth defects in the brain and spine. The CDC has recommended 400 micrograms (mcg) daily for all women who could become pregnant since 1992. That’s not a guess-it’s backed by a landmark study in the New England Journal of Medicine that showed a 72% drop in neural tube defects when women took folic acid before and during early pregnancy.
During pregnancy, your body needs even more: 600 mcg of Dietary Folate Equivalents (DFE) per day. That’s why most prenatal vitamins contain 600 to 1,000 mcg of folic acid. The U.S. government has been fortifying bread, pasta, and cereals with folic acid since 1998. That public health move cut neural tube defect rates by nearly half in just a few years.
But here’s the catch: your baby’s neural tube closes between days 21 and 28 after conception. If you wait until you miss your period to start taking folic acid, you’ve already missed the window. That’s why experts say: start at least one month before you try to conceive.
How Folic Acid Works-and Why It Can Clash With Medications
Folic acid doesn’t work by itself. Your body converts it into its active form, L-methylfolate, which helps build DNA and repair cells. But some medications interfere with this process. For example, anticonvulsants like phenytoin (Dilantin), carbamazepine (Tegretol), and valproic acid are designed to slow down nerve activity in the brain. Folic acid can reduce their effectiveness, which is dangerous for women with epilepsy.
One Reddit user, u/AnxiousMom2022, shared how she started taking 800 mcg of folic acid with her prenatal vitamin and had a breakthrough seizure two weeks later. Her neurologist confirmed it: folic acid was lowering her phenytoin levels. She had to switch to a higher dose of her seizure medication and take folic acid at a different time of day.
Other drugs that interact with folic acid include:
- Methotrexate (used for rheumatoid arthritis and ectopic pregnancy): Folic acid can reduce its toxicity, which is why doctors sometimes prescribe it alongside methotrexate during treatment-but only under strict supervision.
- Pyrimethamine (for toxoplasmosis): Folic acid can make this drug less effective. Pharmacists report that 32% of pregnant women on this medication need dose adjustments when adding folic acid.
- Sulfasalazine (for ulcerative colitis): This drug blocks folic acid absorption. The UK’s NICE guidelines warn against combining them without medical oversight.
- Trimethoprim (an antibiotic): It works similarly to methotrexate and can interfere with folate metabolism.
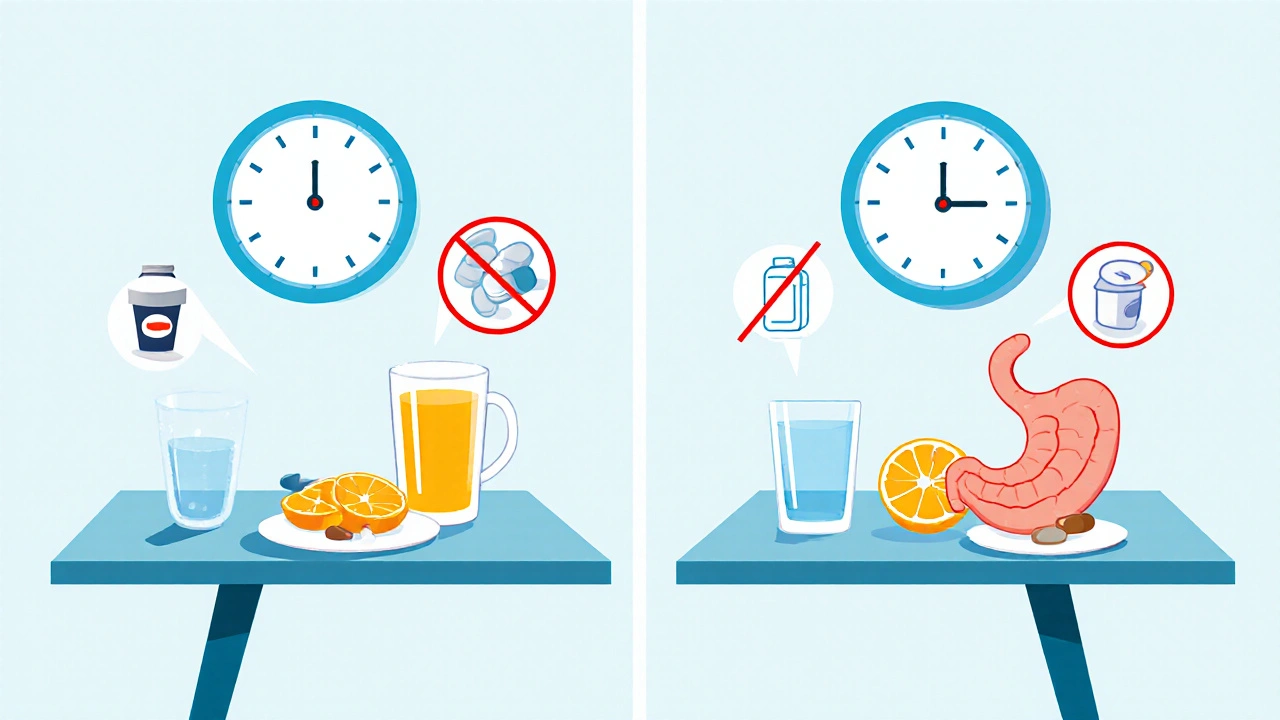
It’s not just prescription drugs. Even over-the-counter antacids can reduce folic acid absorption by up to 50%. Calcium-rich foods like milk, cheese, and yogurt can knock absorption down by 25%. That’s why experts recommend taking folic acid on an empty stomach with water-ideally first thing in the morning, before breakfast.
Iron in Prenatal Vitamins: A Hidden Problem
Most prenatal vitamins include iron because pregnancy increases your blood volume. But here’s the problem: iron and folic acid compete for absorption in your gut. A 2017 study in the American Journal of Clinical Nutrition found that taking them together reduces folic acid absorption by 20-30%.
That’s why so many women report nausea and stomach upset when taking prenatal vitamins. It’s not just the iron-it’s the combination. A 2023 survey by What to Expect found that 78% of pregnant women felt nauseous with iron-containing prenatal vitamins. Of those, 62% switched to taking folic acid separately from iron, spacing them out by at least two hours.
One solution? Take your prenatal vitamin with food to reduce nausea, and take your folic acid supplement on an empty stomach in the morning. Or, if your doctor approves, split your supplements: iron at night, folic acid in the morning.
Who Needs More Than 800 mcg of Folic Acid?
Most women are fine with 600-800 mcg daily. But some need much more.
- Women with epilepsy on carbamazepine or valproic acid: 4,000-5,000 mcg per day under a neurologist’s care.
- Women with a prior neural tube defect pregnancy: 4,000 mcg daily before conception and through the first trimester.
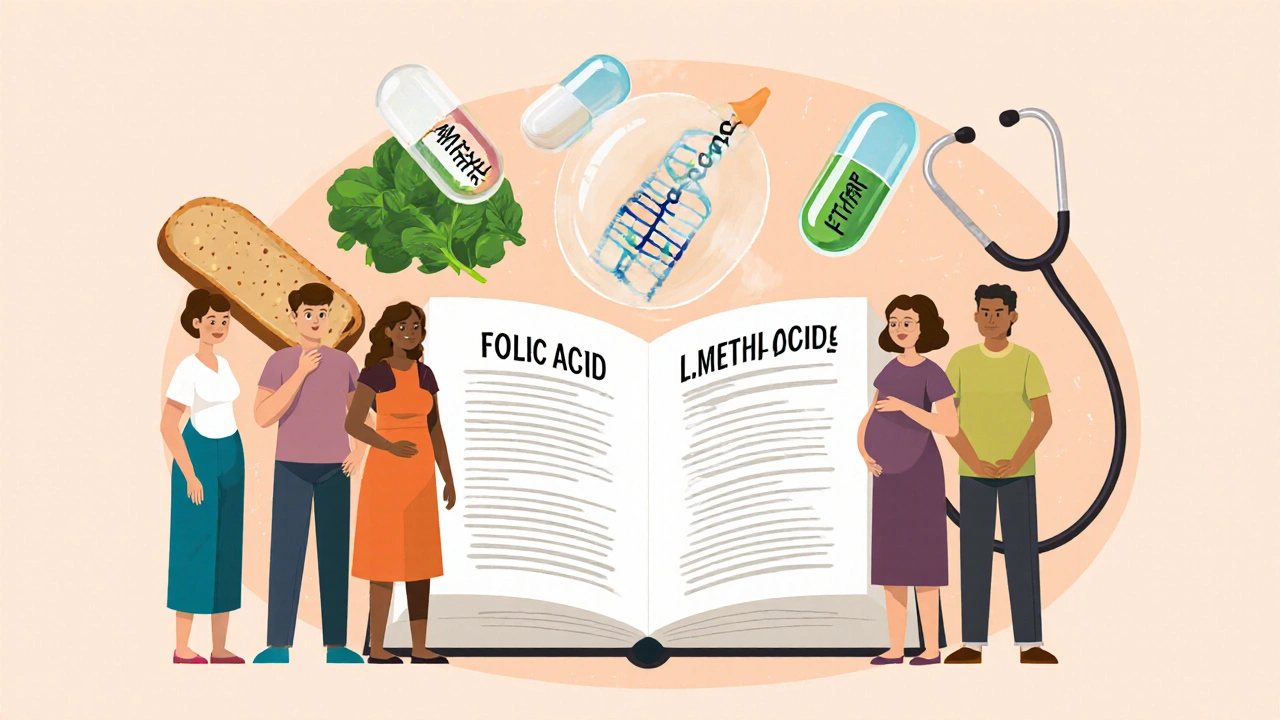
- Women with MTHFR gene mutations: About 10-15% of Caucasians and 20-25% of Hispanics have a genetic variation that makes it harder to convert folic acid into its active form. For them, L-methylfolate (like Quatrefolic®) is a better option. The FDA approved the first prenatal vitamin with this form in 2023.
- Women with diabetes, obesity, or sickle cell disease: Higher doses may be recommended, though evidence is still being studied.
Never take more than 1,000 mcg of folic acid daily unless your doctor tells you to. While the CDC says there’s no confirmed harm from excess folic acid, some researchers worry about unmetabolized folic acid building up in the bloodstream-especially with doses above 1,000 mcg. That’s why most prenatal vitamins cap out at 1,000 mcg.
What’s in Your Prenatal Vitamin? Not All Are Created Equal
Not every prenatal vitamin is the same. A 2020 ConsumerLab review tested 15 popular brands and found that 12 met safety standards for heavy metals. But the differences in folic acid content were huge:
| Brand | Folic Acid (mcg) | Form | Price/Month | Notes |
|---|---|---|---|---|
| Prenate Pixie | 1,000 | Synthetic | $45 | Prescription-only, higher dose for high-risk pregnancies |
| Thorne Basic Prenatal | 800 | Synthetic | $38.99 | Third-party tested, no fillers |
| Nature Made Prenatal Multi + DHA | 800 | Synthetic | $15.99 | Widely available, good value |
| CVS Health Prenatal | 800 | Synthetic | $8.99 | Meets USP standards |
| Quatrefolic® Prenatal | 800 | L-Methylfolate | $45.99 | For MTHFR mutations; FDA-approved in 2023 |
Price doesn’t always mean quality. CVS Health and Nature Made both deliver the same amount of folic acid as premium brands-just at a fraction of the cost. What matters most is whether the product is USP-verified (which means it’s been tested for purity and potency).
What Women Are Missing: The Knowledge Gap
A 2023 survey found that 43% of pregnant women didn’t know folic acid could interact with medications. And 18% were taking anticonvulsants or other drugs without telling their OB-GYN. That’s terrifying. Many women assume “natural” or “over-the-counter” means safe. It doesn’t.
Even doctors can miss this. A woman in Melbourne told her midwife she was taking a prenatal vitamin and an over-the-counter acid reducer for heartburn. The midwife didn’t ask about timing. Weeks later, her folic acid levels came back low. That’s when they realized the antacid was blocking absorption.
Always tell your doctor or pharmacist about every supplement and medication you’re taking-even if you think it’s harmless. That includes herbal teas, probiotics, and CBD oil. Some herbs can interfere with folate metabolism too.
What You Should Do Right Now
If you’re trying to get pregnant or just found out you are, here’s your action plan:
- Check your current supplements. Look at the label. Is it at least 400 mcg of folic acid? If not, start a separate supplement.
- Review your medications. Are you on epilepsy drugs, antibiotics, or acid reducers? Talk to your doctor about interactions.
- Time your doses. Take folic acid on an empty stomach in the morning. Take iron and calcium-rich foods later in the day.
- Don’t self-prescribe high doses. Only take more than 1,000 mcg if your doctor says so.
- Ask about L-methylfolate. If you have a family history of neural tube defects, MTHFR mutations, or poor response to standard folic acid, ask your doctor if a different form might work better.
There’s no magic pill that guarantees a healthy baby. But getting folic acid right-on time, in the right dose, and without interference-is one of the most powerful things you can do.
Can I get enough folic acid from food alone during pregnancy?
No. While foods like spinach, lentils, and fortified cereals contain folate, your body absorbs only about 50% of it. Folic acid from supplements is 100% bioavailable. Even with a perfect diet, you’d need to eat over 2 cups of cooked spinach every day to reach 600 mcg. That’s not realistic. Supplements are necessary.
Is it safe to take folic acid with morning sickness remedies?
It depends. Ginger and vitamin B6 are generally safe. But many anti-nausea medications contain antihistamines or other compounds that may interfere with folate absorption. Always check with your doctor before combining any remedy with your prenatal vitamins.
What if I didn’t start folic acid until after I found out I was pregnant?
Start immediately. While the neural tube closes by day 28, continuing folic acid through the first trimester still supports healthy brain and spinal cord development. It’s not too late to reduce risks. Your doctor may recommend a higher dose if you’re behind.
Can folic acid cause autism?
No. In fact, a 2022 study of over 45,000 children showed a 40% lower risk of autism spectrum disorder in children whose mothers took folic acid before and during early pregnancy. Some older studies suggested a link, but they were flawed. The latest, largest studies show folic acid is protective, not harmful.
Should I switch to L-methylfolate instead of folic acid?
Only if you have a known MTHFR mutation or your doctor recommends it. For most women, regular folic acid works perfectly. L-methylfolate is more expensive and not proven to be better unless your body can’t convert folic acid properly. Genetic testing isn’t routinely recommended unless you have a personal or family history of neural tube defects.
Is it okay to take folic acid while breastfeeding?
Yes. The Recommended Dietary Allowance drops to 500 mcg DFE while breastfeeding, but continuing your prenatal vitamin is still safe and beneficial. Folic acid passes into breast milk and supports your baby’s development. It won’t harm your milk supply or your baby.
Final Thought: Don’t Guess. Ask.
Pregnancy is full of unknowns. But folic acid interactions? That’s not one of them. The science is clear. The risks are real. And the solutions are simple: know your meds, time your doses, and talk to your doctor. You don’t need to be a scientist to protect your baby. You just need to be informed.
Ellen Calnan
November 19, 2025 AT 16:32Okay, but let’s be real-why is it that the moment you say ‘pregnancy’ everyone turns into a nutrition cop? I took my prenatal with a peanut butter sandwich and a cup of coffee and my kid is now a 7-year-old who can solve Rubik’s cubes blindfolded. Science is great, but so is intuition. Maybe we’re over-medicalizing something that used to just… happen.
Also, my OB didn’t mention any of this until I brought up my acid reflux meds. Why is that on us to figure out? Why isn’t this in the pamphlet they hand you at your first appointment?
And why is L-methylfolate $45? That’s a month’s rent for some people. This isn’t healthcare-it’s a luxury market with a baby blanket on top.
Andrew Montandon
November 20, 2025 AT 12:47YES. Thank you. I’m a nurse, and I’ve seen so many women panic because they didn’t know their seizure meds could drop their folic acid levels. One patient had a seizure at 8 weeks-she thought it was just stress. Turns out her folic acid was at 3 ng/mL. She’s now on 5,000 mcg and her baby is due next month. This info saves lives.
Also-iron and folic acid together? That’s a recipe for nausea city. I tell all my patients: take folic acid on an empty stomach at 7 a.m., iron at 9 p.m. with a snack. Game changer.
And yes, CVS prenatal works just fine. No need to spend $45 unless you have MTHFR. Don’t let marketing scare you.
Richard Risemberg
November 21, 2025 AT 09:32Let me tell you about my cousin. She’s a yoga instructor, vegan, drinks kale smoothies every morning, and swore she didn’t need supplements. Got pregnant, didn’t take folic acid, and ended up with a baby with spina bifida. She cried for three months. She thought ‘natural’ meant ‘safe.’ It doesn’t.
And here’s the kicker: she didn’t even know she had an MTHFR mutation until after. Now she’s on Quatrefolic, and her second kid? Perfect. No issues.
So yes-this isn’t fearmongering. It’s survival. If you’re trying to conceive, take the pill. Don’t wait for the ‘perfect’ diet. Your body needs the synthetic version because evolution hasn’t caught up with our processed food world. Stop romanticizing ‘whole foods’ when your baby’s spine is on the line.
Frank Dahlmeyer
November 22, 2025 AT 08:53Look, I’ve been researching this for two years since my wife had her first miscarriage. We did everything right-organic food, no caffeine, yoga, meditation, even got our DNA tested. Turned out her folic acid levels were fine, but she was on sulfasalazine for Crohn’s and the docs never told her it blocks absorption. She didn’t even know the drug was in her system until we got the lab results. That’s the problem. Doctors assume you know your meds. You don’t. You just take what they hand you.
And here’s what nobody talks about: the gut. If you’ve got leaky gut, IBS, or even just chronic stress, your body can’t absorb folic acid no matter how much you take. That’s why some women on 1,000 mcg still have low levels. It’s not the dose-it’s the delivery system. Probiotics, digestive enzymes, and gut healing might be the real missing piece here. But no one wants to talk about that. Too messy. Too expensive. Too inconvenient.
So yes-take the pill. But also fix your gut. Your baby deserves more than a vitamin and a prayer.
Marjorie Antoniou
November 24, 2025 AT 05:28I had a friend who took folic acid with her antacid and ended up with low folate levels. She didn’t know until her anatomy scan showed a slight neural tube issue. She was terrified. But because she spoke up, they adjusted her meds and she’s now holding her healthy 6-month-old. Please-don’t assume your doctor knows everything. Bring your supplement list. Write it down. Ask, ‘Could this interact with my prenatal?’ It’s not being difficult. It’s being responsible.
And if you’re worried about cost-ask for samples. Ask for generics. Ask for help. You’re not alone. This system is broken, but you still have power. Use it.
Chuck Coffer
November 24, 2025 AT 16:58Wow. So you’re telling me the entire medical establishment is just… clueless? That’s rich. I’ve been taking 1,000 mcg of folic acid since I turned 25. I’ve never been pregnant. I don’t plan to be. But now I’m supposed to feel guilty because I didn’t know my ibuprofen might interfere with absorption? I’m not a doctor. I’m not a pharmacist. I’m just a guy who takes a multivitamin because my wife said it’s ‘good for me.’
And now I’m supposed to time my supplements like a NASA launch? I’m exhausted just reading this. Who’s really benefiting here? The supplement industry. The pharmaceutical companies. The OB-GYNs who upsell Quatrefolic for $45 a bottle.
Maybe the real problem isn’t folic acid. It’s that we’ve turned pregnancy into a full-time job with mandatory homework.
Sam Reicks
November 25, 2025 AT 03:43you know what they dont tell you right? folic acid is a scam. its not even real folate. its a synthetic poison made by big pharma to make people buy more pills. the body cant process it right and it builds up and causes cancer. the real solution is eating spinach and liver. thats what our ancestors did. they didnt have pills. they had food. and they had healthy babies. why are we so stupid now?
also the cdc is run by the same people who gave us aspartame and vaccines. dont trust them. i stopped taking my prenatal and my wife got pregnant on the first try. no pills. just eggs and bacon. baby is 18 months old and can already recite the alphabet. science is fake.
Michael Petesch
November 26, 2025 AT 05:55While the data on folic acid and neural tube defects is robust, the real issue lies in healthcare accessibility. The 43% of women unaware of drug interactions? Many are low-income, underinsured, or live in food deserts where prenatal vitamins are a luxury. The CDC’s recommendations are sound, but they assume a baseline of medical literacy and economic stability that doesn’t exist for millions. We need community health workers, not just pamphlets. We need pharmacies in rural clinics, not just Amazon Prime deliveries. And we need doctors trained to ask, ‘What are you taking?’-not just ‘Are you taking your prenatal?’
This isn’t just about biochemistry. It’s about justice. A woman in rural Mississippi shouldn’t have to Google ‘folic acid and Tegretol’ to protect her baby. That’s not empowerment. That’s neglect dressed up as education.
Codie Wagers
November 26, 2025 AT 17:33There’s a deeper philosophical flaw here: we’ve outsourced biological responsibility to pharmacology. We’ve turned the sacred act of creating life into a protocol. Folic acid isn’t a miracle-it’s a bandage on a broken system. Why are we not addressing the root causes of neural tube defects? Environmental toxins? Poor nutrition? Chronic stress? The over-medicalization of pregnancy has created a culture of fear, not empowerment. We’ve replaced wisdom with dosage charts. We’ve replaced intuition with lab values.
And yet, despite all this, the human body still manages to create life-often in spite of the system. The real miracle isn’t the supplement. It’s the body. The body that has been doing this for millennia without a single pill. Maybe the question isn’t ‘How much folic acid?’ but ‘Why have we forgotten how to trust ourselves?’
Andrew Baggley
November 28, 2025 AT 14:09You got this. Seriously. Even if you’re late, even if you’re scared, even if you forgot your pill for three days-start now. Your baby is already worth it. I know it feels overwhelming. I’ve been there. But you’re not alone. Millions of women are doing this right now, fumbling through the same confusion, the same guilt, the same ‘did I mess up?’ moments.
Take the vitamin. Talk to your doctor. Don’t let the noise drown out the truth: you’re already doing better than you think. You’re reading this. You’re trying. That’s everything.