Fluoroquinolones and Tendon Rupture: What You Need to Know About the Risk
 Nov, 13 2025
Nov, 13 2025
Fluoroquinolone Tendon Risk Calculator
Calculate Your Risk
This tool estimates your risk of tendon damage when taking fluoroquinolone antibiotics based on FDA and MHRA guidelines. Results are for informational purposes only.
Your Risk Assessment
Fluoroquinolones Can Cause Tendon Rupture-Even After You Stop Taking Them
You take an antibiotic because you’re sick. You trust it. You expect it to fix the infection, not break your body in a different way. But for some people, common antibiotics like ciprofloxacin, levofloxacin, and moxifloxacin can lead to something far worse than a stomach upset: a sudden, painful tear in a tendon-often the Achilles tendon in the heel. This isn’t rare. It’s not a one-in-a-million fluke. It’s a well-documented, serious risk that doctors are now told to take seriously.
The U.S. Food and Drug Administration (FDA) put a black-box warning on these drugs in 2008-the strongest possible alert. The UK’s MHRA followed in 2019, restricting their use to only the most serious infections when nothing else works. Why? Because the evidence is overwhelming: fluoroquinolones can damage tendons, sometimes within days, sometimes months after you’ve stopped taking them.
Which Fluoroquinolones Are Most Likely to Cause Tendon Damage?
Not all fluoroquinolones are the same when it comes to tendon risk. Data from VigiBase, a global drug safety database, shows clear patterns:
- Levofloxacin: 50.04% of reported tendon cases
- Ciprofloxacin: 38.41%
- Moxifloxacin: 5.16%
That means if you’re prescribed one of these, you’re not just getting “an antibiotic.” You’re getting a drug with a known, measurable risk. And the Achilles tendon-the thick cord connecting your calf to your heel-is the most vulnerable. It’s involved in nearly 90% of all reported cases. In half of those cases, both heels are affected.
It’s not just the drug itself. It’s how your body reacts to it. Fluoroquinolones interfere with collagen, the protein that gives tendons their strength. They trigger cell death in tendon tissue, increase inflammation-causing chemicals like nitric oxide, and disrupt the energy production in your tendon cells by damaging mitochondria. In short, they weaken tendons from the inside out.
When Does the Damage Happen?
Most people assume side effects show up while they’re still taking the medicine. That’s not always true with fluoroquinolones.
The median time between starting the drug and the first sign of tendon pain is just 6 days. About 85% of cases occur within the first month. But here’s what scares doctors: up to half of tendon injuries happen after you’ve finished the course. One patient might feel fine after 10 days of pills, then tear their Achilles while walking to the mailbox a week later.
There are even reports of tendon rupture starting within two hours of taking the first dose. In one documented case, a 68-year-old man collapsed while walking-his Achilles had snapped after just one pill.

Who’s at the Highest Risk?
This isn’t a risk that affects everyone equally. Some people are far more vulnerable.
- Age 60 and older: Your tendons naturally lose elasticity with age. Add fluoroquinolones, and the risk jumps 6.4 times for those 60-79. For those over 80? The risk is more than 20 times higher.
- Corticosteroids: If you’re taking prednisone, dexamethasone, or any steroid-whether for asthma, arthritis, or an autoimmune condition-the risk of rupture increases by 46 times. This combination is a recipe for disaster.
- Diabetes: Poor blood flow and nerve damage from diabetes make tendons more fragile.
- Kidney problems: Fluoroquinolones are cleared by the kidneys. If your kidneys aren’t working well, the drug builds up in your system, increasing toxicity.
- Previous tendon injury: If you’ve had a torn tendon before, you’re at higher risk of another one.
Women also show slightly higher rates of tendon issues than men, though the reason isn’t fully understood. It might be hormonal, anatomical, or related to how the drugs are metabolized.
What Are the Warning Signs?
Tendon rupture doesn’t always come with a loud pop. Often, it starts quietly.
- Pain or swelling in the heel, shoulder, or hand
- Stiffness that doesn’t go away with rest
- Tenderness when you press on the tendon
- Difficulty walking, climbing stairs, or lifting your arm
Dr. Grace K. Kim, a dermatology researcher, pointed out that tendonitis symptoms often appear two weeks before a full rupture. That’s your window to act. If you feel any of these while taking a fluoroquinolone-or even within months after stopping-stop the drug and see a doctor immediately. Don’t wait for pain to turn into a snap.
Why Do Some Studies Say There’s No Risk?
It’s confusing. You might read a study from Japan that says fluoroquinolones aren’t linked to tendon rupture. How can that be?
That 2022 study analyzed 504 patients with Achilles tears and found no clear link with third-generation fluoroquinolones. But here’s the catch: it was a small group, and it used a different method-comparing patients to themselves over time, rather than comparing users to non-users. Other studies, like the massive UK analysis of 6.4 million people and Taiwan’s 357,000-patient cohort, found clear, statistically significant increases in rupture risk.
Regulatory agencies don’t rely on single studies. They look at the whole picture: millions of patient records, thousands of adverse event reports, decades of clinical data. The FDA, EMA, and MHRA all agree: the risk is real. The Japanese study doesn’t erase that. It just shows we still don’t understand all the factors.
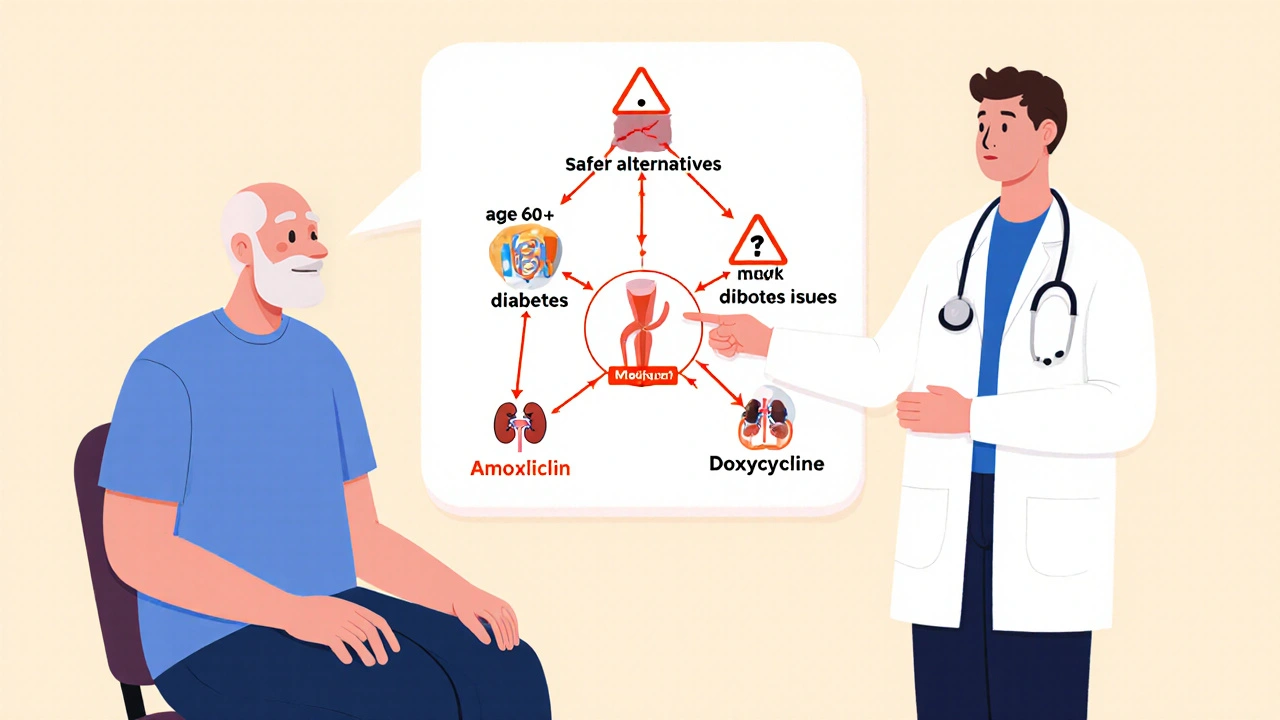
What Should You Do If You’re Prescribed a Fluoroquinolone?
Don’t refuse antibiotics if you need them. But do ask questions.
Before you take one, ask your doctor:
- Is this the best option? Could I use amoxicillin, doxycycline, or another antibiotic instead?
- Am I in a high-risk group? (Age? Steroids? Kidney issues?)
- What are the signs of tendon damage I should watch for?
- What should I do if I feel pain?
If you’re over 60, on steroids, or have diabetes-push back. Fluoroquinolones are now considered third-line treatments by the Infectious Diseases Society of America. That means they’re only for serious infections like complicated UTIs, pneumonia in hospitalized patients, or anthrax exposure. They’re not for sinus infections, ear infections, or simple bronchitis.
What If You Already Took One and Feel Fine?
Good. But don’t assume you’re safe.
Because tendon damage can show up months later, you should still be alert for the next 3-6 months. If you feel any unusual stiffness, pain, or swelling in your tendons-especially your heels-don’t ignore it. Stop physical activity, rest, and get it checked. Early intervention can prevent a full rupture.
And if you’ve had a tendon rupture after taking a fluoroquinolone, tell your doctor. Report it to your country’s drug safety agency. These reports help regulators understand how common and severe the problem really is.
Bottom Line: Don’t Panic, But Don’t Be Complacent
Fluoroquinolones save lives. They’re powerful tools against deadly infections. But they’re not harmless. Their risks are real, predictable, and preventable-if you know what to look for.
If you’re prescribed one, don’t take it blindly. Ask if it’s truly necessary. Know the warning signs. Watch your body. And if you feel pain in a tendon, treat it like an emergency-because it might be.
Can fluoroquinolones cause tendon rupture even after I stop taking them?
Yes. While most tendon issues appear within the first month of taking fluoroquinolones, symptoms-including rupture-can occur weeks or even months after stopping the medication. The UK MHRA and FDA both warn that tendon damage may be delayed, making it harder to link the drug to the injury. If you’ve taken a fluoroquinolone and later feel sudden tendon pain, seek medical attention immediately.
Which fluoroquinolone has the highest risk of tendon damage?
Levofloxacin carries the highest reported risk, accounting for over half of all tendon-related adverse events in global drug safety databases. Ciprofloxacin is second, with about 38% of cases. Moxifloxacin is less commonly linked, but still carries risk. The risk isn’t just about which drug-it’s about your personal factors like age, steroid use, and kidney function.
Is it safe to take fluoroquinolones with steroids?
No. Combining fluoroquinolones with corticosteroids increases the risk of tendon rupture by up to 46 times. This combination is considered extremely dangerous. If you’re on prednisone or another steroid, your doctor should avoid prescribing a fluoroquinolone unless there’s no alternative-and even then, only with extreme caution.
What should I do if I feel tendon pain while taking a fluoroquinolone?
Stop taking the antibiotic immediately and contact your doctor. Do not wait for the pain to get worse. Tendonitis can progress to a full rupture within days. Your doctor will likely recommend rest, immobilization, and possibly imaging like an ultrasound or MRI. Never ignore tendon pain while on these drugs-it’s a medical red flag.
Are there safer alternatives to fluoroquinolones for common infections?
Yes. For most common infections like sinusitis, bronchitis, or uncomplicated UTIs, antibiotics like amoxicillin, doxycycline, nitrofurantoin, or trimethoprim-sulfamethoxazole are safer and equally effective. Fluoroquinolones are now reserved for serious infections like pyelonephritis, hospital-acquired pneumonia, or anthrax. Always ask your doctor if a less risky option is available.
Chris Ashley
November 14, 2025 AT 07:40kshitij pandey
November 15, 2025 AT 23:40Brittany C
November 16, 2025 AT 13:35Sean Evans
November 18, 2025 AT 06:29Anjan Patel
November 19, 2025 AT 23:23Scarlett Walker
November 21, 2025 AT 12:05Hrudananda Rath
November 23, 2025 AT 09:08Brian Bell
November 24, 2025 AT 22:28