Dose-Related vs Non-Dose-Related Side Effects: What You Need to Know in Pharmacology
 Dec, 11 2025
Dec, 11 2025
Pharmacology Side Effect Quiz
Dose-Related vs Non-Dose-Related Side Effects
Test your understanding of pharmacology concepts with this 5-question quiz. Click on your answer, then check your score at the end.
When you take a pill, you expect it to help - not hurt. But sometimes, medications cause side effects. Not all side effects are the same. Some happen because you took too much. Others strike out of nowhere, even at the lowest dose. Understanding the difference between dose-related and non-dose-related side effects isn’t just for doctors - it’s critical for anyone managing long-term medication.
What Are Dose-Related Side Effects?
Dose-related side effects, also called Type A reactions, are predictable. They happen because the drug is doing exactly what it’s supposed to do - just too well. These reactions follow the basic rule of pharmacology: more drug = more effect. If a drug lowers blood pressure, taking too much can drop it too far. If it lowers blood sugar, too much can cause fainting.Think of insulin. A person with diabetes needs just enough to keep glucose in range. Too much? Blood sugar crashes below 70 mg/dL. That’s a classic Type A reaction. Same with warfarin - the right dose thins blood to prevent clots. Too high? INR climbs above 4.0, and you risk dangerous bleeding. These aren’t accidents. They’re extensions of the drug’s intended action.
Drugs with narrow therapeutic windows are especially risky. That means the gap between a helpful dose and a harmful one is tiny. Digoxin, used for heart rhythm, has a therapeutic range of 0.5 to 0.9 ng/mL. Above 2.0 ng/mL? Toxicity. Lithium for bipolar disorder? Safe between 0.6 and 1.0 mmol/L. Go past 1.2? Tremors, confusion, even seizures. That’s why doctors monitor blood levels for these drugs.
These reactions make up 70-80% of all adverse drug reactions. And they’re the main reason older adults end up in the ER. Anticoagulants, insulin, and oral diabetes drugs cause nearly two-thirds of medication-related hospital visits in people over 65. Why? Because aging changes how the body handles drugs. Kidneys slow down. Liver metabolism drops. A dose that was fine at 40 can become dangerous at 70.
What Are Non-Dose-Related Side Effects?
Non-dose-related side effects - Type B reactions - are the opposite. They’re unpredictable. They don’t follow the dose-response curve. You can take one pill and have a life-threatening reaction. Someone else takes ten and feels fine. It’s not about how much you took. It’s about who you are.These are usually immune-driven. Your body sees the drug as an invader and reacts violently. Anaphylaxis from penicillin is a prime example. One dose, and your airways swell. It doesn’t matter if it’s 250 mg or 1,000 mg - the reaction kicks in once your immune system is sensitized. Same with Stevens-Johnson syndrome, a devastating skin reaction triggered by drugs like lamotrigine or sulfonamides. It can happen on the first dose, even when dosing is perfect.
These reactions are rare - only 15-20% of all side effects - but they’re deadly. They cause 70-80% of serious drug-related hospitalizations and account for most drug withdrawals from the market. The mortality rate? 5-10%. Compare that to Type A reactions, which have less than 1% mortality. That’s why Type B reactions scare doctors more, even though they’re less common.
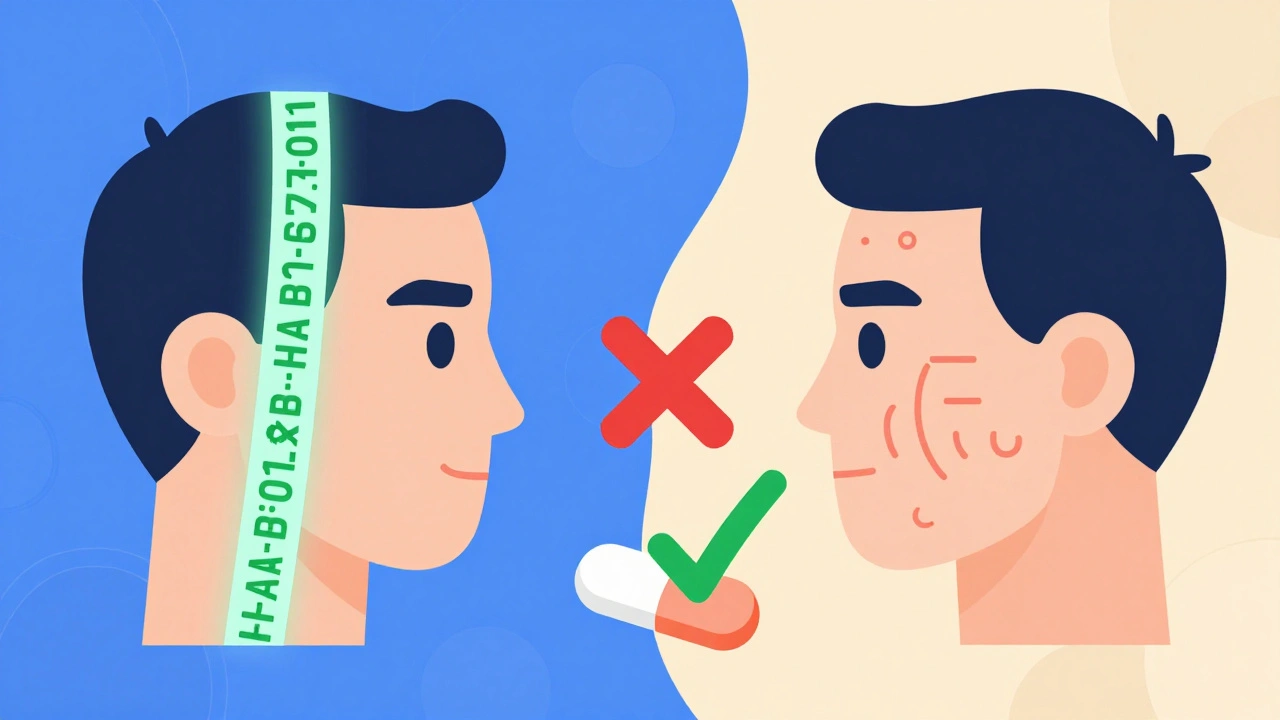
Genetics play a huge role. HLA-B*57:01 is a gene variant that makes people extremely sensitive to abacavir, an HIV drug. If you have this gene, taking abacavir can trigger a severe allergic reaction. But if you don’t have it? You’re safe. That’s why testing for HLA-B*57:01 before prescribing abacavir is now standard. The test costs $150-$300 - far cheaper than treating a life-threatening reaction.
Another example: HLA-B*15:02. Found mostly in people of Asian descent, this gene increases the risk of Stevens-Johnson syndrome from carbamazepine. Screening before starting the drug reduces cases by over 90%. That’s not luck. That’s precision medicine.
Why Do Non-Dose-Related Reactions Even Exist?
At first glance, it doesn’t make sense. If all drugs work by binding to receptors, shouldn’t more drug = more effect? Why would some reactions ignore dose entirely?Researchers like Aronson and Ferner figured it out. There are four reasons why a reaction seems non-dose-related:
- The reaction isn’t real - maybe it’s a coincidence, or misdiagnosed.
- Hypersusceptibility - your body hits maximum reaction at a tiny dose. Any more doesn’t make it worse, but even that small amount triggers it.
- Wild variation between people - one person’s threshold is 1 mg, another’s is 100 mg. In population studies, it looks random.
- Dosing errors - the patient says they took 5 mg, but they actually took 20 mg. The reaction looks non-dose-related, but it wasn’t.
So, even Type B reactions might have a dose threshold. It’s just that the threshold is different for everyone. That’s why we call them “non-dose-related” - not because dose doesn’t matter, but because you can’t predict it from the average person’s response.
How Doctors Handle Each Type
The way doctors respond depends entirely on the type.For Type A reactions, the fix is simple: adjust the dose. If someone’s INR is too high on warfarin, reduce the dose. If blood sugar drops too low on insulin, cut the amount. Therapeutic drug monitoring - checking blood levels of drugs like vancomycin, phenytoin, or lithium - helps keep doses in the safe zone. Dose reductions are also standard for kidney or liver problems. For example, if your kidneys are working at 30% capacity, your enoxaparin dose drops by half.
For Type B reactions? Stop the drug - permanently. No second chances. If you had anaphylaxis to penicillin, you can’t take it again. Not even a tiny dose. You’ll need alternatives. And if you’ve had Stevens-Johnson syndrome from one drug, you’re likely at risk for others in the same class. Avoidance is the only strategy.
Some Type B reactions can be screened for before prescribing. Skin tests for penicillin allergy have a 50-70% positive predictive value. Genetic tests for HLA variants are even better - 99.9% negative predictive value for abacavir. That means if your test is negative, you’re almost certainly safe.
And then there’s the graded challenge - slowly reintroducing a drug under supervision. Used mostly for low-risk penicillin allergies, it works 80-90% of the time. But it’s only done in controlled settings. Never at home.
Who’s at Risk?
Type A reactions hit older adults hardest. Why? Their bodies don’t clear drugs as well. They often take multiple medications, leading to dangerous interactions. For example, clarithromycin (an antibiotic) can spike statin levels by 5-10 times, increasing muscle damage risk. Elderly patients on multiple drugs are walking time bombs for Type A reactions.Type B reactions are trickier. They can strike anyone - young or old. But certain groups are more vulnerable. People with specific genetic markers (like HLA-B*57:01 or HLA-B*15:02) are at higher risk. Those with autoimmune conditions may also be more prone. And women? They’re more likely to develop drug-induced liver injury from drugs like amoxicillin-clavulanate.
It’s not just about the drug. It’s about the person. A 72-year-old woman with kidney disease on warfarin is at high risk for bleeding. A 28-year-old man with HLA-B*15:02 starting carbamazepine is at risk for skin damage. Same drug. Different risks.
The Big Picture: Costs, Lawsuits, and Future Trends
Type A reactions cost the U.S. healthcare system $130 billion a year. They’re the reason for most medication errors, hospitalizations, and insurance claims. But Type B reactions? They’re the ones that lead to lawsuits and drug recalls. One serious reaction can wipe out a drug’s market - especially if it causes death or disfigurement.The future is moving toward personalization. The FDA now lists pharmacogenomic info on 311 drug labels. Twenty-eight drugs require genetic testing before use. The global pharmacogenomics market is projected to hit $18 billion by 2030. Machines are getting better at predicting Type A reactions - 82% accuracy using AI and electronic records. But Type B? Only 63%. That’s because they’re still largely a mystery.
But we’re getting closer. Clinical guidelines from CPIC now tell doctors exactly how to adjust doses based on genes - for both Type A and Type B reactions. And the FDA is preparing to approve software that helps doctors calculate personalized doses using age, weight, genetics, and organ function.
This isn’t science fiction. It’s happening now. And it means the days of “one-size-fits-all” dosing are ending.
What You Can Do
If you’re on long-term medication:- Know your drug’s purpose - and its common side effects. Ask your pharmacist.
- Report even small changes: dizziness, rash, nausea. Don’t wait for something “serious.”
- Ask if you need blood tests. For drugs like warfarin, lithium, or phenytoin, monitoring saves lives.
- If you’ve had a severe reaction, get tested for HLA variants - especially if you’re of Asian descent.
- Carry a medication list. Include doses and dates started. Emergency responders need this.
- Don’t assume “it’s just a side effect.” If it’s new, unusual, or scary - speak up.
Side effects aren’t always your fault. Sometimes, they’re built into the drug. Sometimes, they’re built into your genes. Understanding the difference between dose-related and non-dose-related reactions helps you take control - not just of your meds, but of your health.
Keasha Trawick
December 11, 2025 AT 17:44Okay, but have you ever seen someone go full Stevens-Johnson from a damn ibuprofen? I know a girl who got a rash from a single 200mg tablet-no prior allergies, no family history, just… poof. Her skin started peeling like a sunburn on acid. ER. ICU. Three weeks in the hospital. And the doctor just shrugged and said, ‘Weird gene thing.’ That’s not a side effect-that’s a biological betrayal. And we still don’t screen for most of these. We’re playing Russian roulette with our meds and calling it ‘standard care.’
Alvin Montanez
December 12, 2025 AT 16:04Look, I’m not one to mince words, but this whole pharmacogenomics movement is just another way for Big Pharma to charge more while pretending they care. They’ll sell you a $300 genetic test so you can avoid a drug they just patented last year-while the generic version that’s been around since the 70s still causes the same reactions in 1 in 10,000 people. Meanwhile, your grandma’s warfarin dose is still being adjusted by a nurse with a paper chart and a prayer. We’re not advancing medicine-we’re just adding layers of bureaucracy and profit margins to the same old mistakes. If you want to save lives, stop selling tests and start fixing dosing protocols for the elderly. That’s where the bodies are piling up.
And don’t get me started on how we treat Type A reactions like they’re just ‘user error.’ No, it’s system failure. Doctors don’t adjust for renal decline. Pharmacies don’t flag interactions. Insurance won’t pay for monitoring. So when Mr. Johnson gets hospitalized for a lithium level of 1.8, it’s not his fault-it’s the system’s. But we blame the patient because it’s easier than fixing the machine.
And yes, I know the FDA says they’re moving toward personalized medicine. But if you look at the actual adoption rates in community clinics, less than 12% of primary care docs even know what HLA-B*57:01 means. This isn’t the future-it’s a marketing brochure with a few real studies tucked in.
And let’s not pretend that AI is going to solve this. Algorithms trained on biased datasets will just keep recommending higher doses to white patients and lower doses to Black patients under the guise of ‘precision.’ We’ve done this before with kidney function equations. We’re not building better tools-we’re automating our prejudices.
So yes, the science is fascinating. But until we fix the infrastructure, the billing codes, the training, and the profit motives, this is all just academic theater. Real change doesn’t come from gene panels. It comes from forcing hospitals to hire clinical pharmacists. And no one wants to pay for that.
Donna Hammond
December 13, 2025 AT 19:06Thank you for writing this so clearly. As a nurse who’s seen patients get sent home with dangerously high INRs because their doctor didn’t check labs for six weeks, I can’t tell you how refreshing this is. Too many people think side effects are just ‘part of taking medicine’-but they’re not. They’re red flags. And we need to treat them like emergencies, not annoyances.
One thing I always tell my patients: if you notice something new-even if it seems small-write it down. Dizziness? Rash? Unusual fatigue? Don’t wait for it to get worse. Call your provider. Bring your pill bottles. I’ve saved lives just by catching a drug interaction before it turned into a hospital stay.
And yes, genetic testing isn’t perfect, but if you’re of Asian descent and about to start carbamazepine? Get tested. It’s a simple blood draw. $150 could save you from months in the burn unit. That’s not optional-it’s essential.
Also, if you’re on multiple meds, especially over 65? Ask for a med review. Most pharmacies offer it for free. A pharmacist can spot interactions your doctor missed. Don’t be shy. You’re not bothering them-you’re protecting yourself.
We’re not powerless here. We just have to speak up, stay informed, and demand better. You deserve to take your meds without fear.
Sheldon Bird
December 14, 2025 AT 07:58Big respect to the OP for breaking this down so clearly. 🙌 I used to think side effects were just ‘bad luck’-now I get why my uncle had to stop his blood pressure med after one pill. Not because he took too much… but because his body just said ‘nope.’
My mom’s on lithium and we do monthly blood draws like clockwork. It’s annoying, yeah-but it’s also the only thing keeping her stable. I wish more people knew how crucial monitoring is. It’s not micromanaging-it’s self-care.
Also, if you’ve ever had a rash from a new med? Don’t brush it off. I almost lost my cousin to a delayed reaction because she thought ‘it’ll go away.’ It didn’t. Please, speak up. You’re not overreacting. You’re being smart.
And hey-if you’re into this stuff, check out CPIC guidelines. They’re free, they’re real, and they actually help. 🤓
Karen Mccullouch
December 14, 2025 AT 22:57Oh here we go again with the ‘genetics’ excuse. You know what really causes these reactions? The government letting Big Pharma poison us with untested crap because they’re too busy taking bribes to care. I’ve seen it-my cousin got SJS from a generic antibiotic that was approved in 2018 with ZERO long-term studies. And now? They’re selling it in every Walmart. Meanwhile, the FDA is busy approving new weight-loss drugs that cause suicidal ideation. This isn’t science. It’s corporate warfare. And you’re all just sitting here talking about HLA variants like it’s a TED Talk. Wake up. This is deliberate. They want you dependent. They want you scared. They want you paying for tests so you don’t question why the drug was approved in the first place.
STOP FOCUSING ON GENES. START FOCUSING ON THE CORPORATIONS THAT PROFIT FROM YOUR SUFFERING.
Michael Gardner
December 16, 2025 AT 00:57Interesting take, but let’s flip this: what if Type B reactions aren’t ‘non-dose-related’ at all? What if we just haven’t measured the dose correctly? Maybe it’s not the milligrams-it’s the timing. Or the food you ate. Or your gut microbiome. Or your sleep cycle. We’ve been measuring drugs like they’re static, but the human body is a dynamic, ever-shifting ecosystem. We’re using 1950s tools to analyze 2024 biology. Of course it looks random.
And let’s be real-most ‘non-dose-related’ reactions are just cases where the patient lied about what they took. ‘I only took one pill’-but they took three because they were desperate for relief. We call it ‘non-dose-related’ because we refuse to admit people don’t follow instructions.
Also, if you’re going to blame the system for Type A reactions, why not blame the patient for Type B? We’re not helpless victims. We’re participants. And if we want better outcomes, we need to own our role in them-not just blame the FDA.
Willie Onst
December 16, 2025 AT 22:52Man, this post hit different. 🌱 I’ve been on antidepressants for 12 years, and honestly? I used to think my weird side effects were just ‘me being dramatic.’ But now I get it-some of it’s my liver processing things slower. Some of it’s my genes. And some of it? Probably just bad luck.
I love that we’re finally starting to see medicine as a conversation between the drug and the person-not just a script. Like, my doc actually asked me about my ancestry before prescribing carbamazepine. I’m half Filipino, and he said, ‘We’re gonna test you.’ That felt… human.
It’s not magic. It’s not conspiracy. It’s just science finally catching up to how complicated we are. And that’s kind of beautiful, you know? We’re not broken machines. We’re living, evolving, genetically unique beings. And maybe, just maybe, medicine is learning to treat us that way.
Keep sharing this stuff. We need more of it.
Ronan Lansbury
December 18, 2025 AT 03:04Of course they call it ‘non-dose-related.’ That’s the official narrative. But have you ever considered that these reactions are triggered by chemtrails? Or 5G? Or the glyphosate in your water? The pharmaceutical industry doesn’t want you to know that these ‘genetic’ reactions are actually caused by environmental toxins they’ve been dumping for decades. HLA-B*57:01? A convenient distraction. The real culprit is the sodium fluoride in your toothpaste. You think they test for that? No. They test for genes because genes can’t sue them.
And don’t believe the ‘FDA-approved’ lie. The FDA is a revolving door for ex-pharma execs. That’s why they approve drugs that kill. That’s why they ignore the real causes. You think this is science? It’s a controlled experiment-and you’re the lab rat.
Jennifer Taylor
December 18, 2025 AT 15:19Okay, so I just got diagnosed with HLA-B*15:02 and now I can’t take carbamazepine? But my cousin took it for 10 years and had zero issues? So what’s the point of the test if it doesn’t work for everyone? And why didn’t my doctor tell me this before I started the med? I had a rash for three weeks and they called it ‘allergic reaction’-no test, no warning. Now I’m terrified of every new pill. What if the next one kills me? And why is this only tested in Asians? What about me? I’m mixed race-half Mexican, half Irish. Do I get tested? Who decides? I feel like my body is a minefield and no one gave me a map.
Also, can we talk about how expensive this all is? My insurance won’t cover the genetic test unless I’m already hospitalized. So I have to wait until I’m almost dead to get the test? That’s not prevention. That’s punishment.