Diabetic Nephropathy: How ACE Inhibitors, ARBs, and Protein Control Protect Your Kidneys
 Dec, 28 2025
Dec, 28 2025
Why Diabetic Nephropathy Is a Silent Threat
One in three people with diabetes will develop kidney damage. It doesn’t come with pain, swelling, or obvious warning signs-until it’s too late. This is diabetic nephropathy: a slow, silent breakdown of the kidneys caused by high blood sugar over years. The first clue? Protein leaking into the urine. That’s not normal. Your kidneys are supposed to keep protein in your blood. When they start letting it out, it’s a red flag.
By the time symptoms like swelling in the legs or fatigue show up, the damage is often advanced. That’s why catching it early with a simple urine test matters. The goal isn’t just to manage blood sugar-it’s to protect your kidneys before they fail. And the best tools we have right now are ACE inhibitors and ARBs, paired with strict protein control.
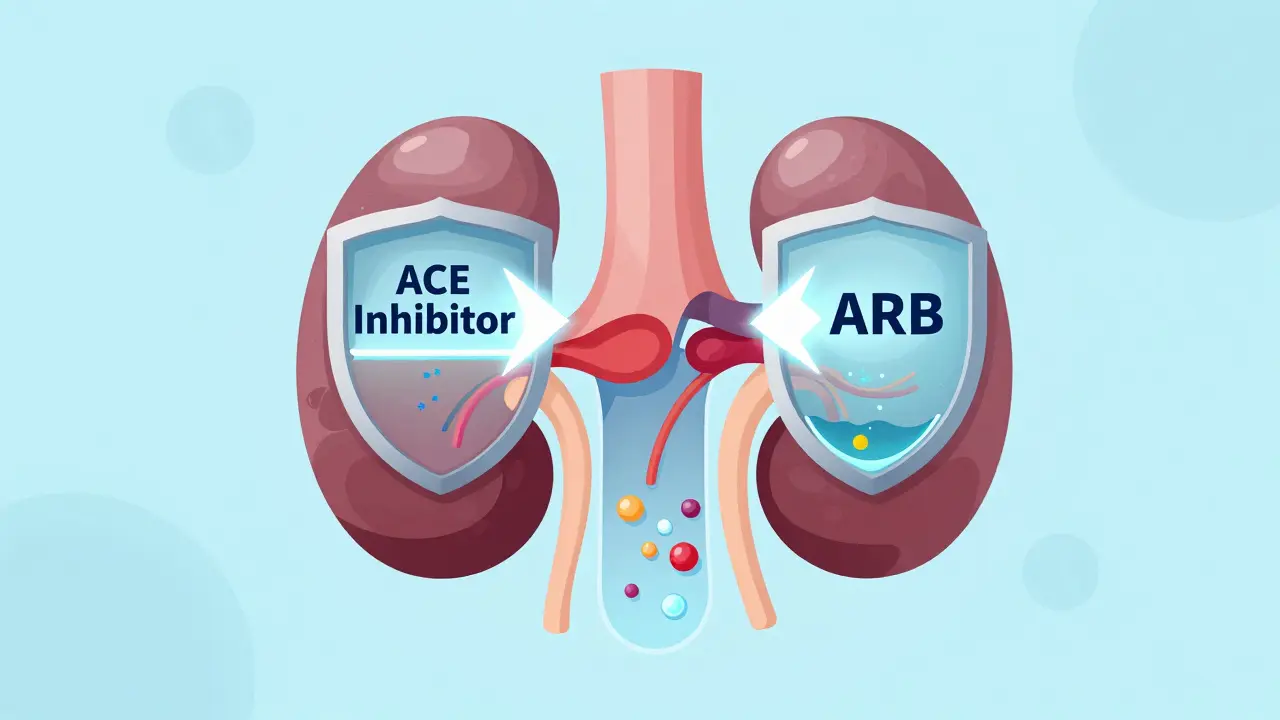
How ACE Inhibitors and ARBs Actually Work
These aren’t just blood pressure pills. They’re kidney shields. ACE inhibitors like ramipril, benazepril, and captopril block the enzyme that turns angiotensin I into angiotensin II. ARBs like losartan and irbesartan block the receptors that angiotensin II binds to. Either way, you’re shutting down the same harmful pathway-the renin-angiotensin-aldosterone system, or RAAS.
Here’s the key: high pressure inside the kidney’s filtering units (glomeruli) crushes them over time. RAAS activation makes that pressure worse. By blocking it, these drugs lower that internal pressure. That’s why they reduce proteinuria-sometimes by 30% to 50%. Less protein in the urine means slower kidney decline.
Studies like RENAAL and IDNT showed that ARBs cut the risk of needing dialysis by up to 28% in people with type 2 diabetes and heavy protein leakage. ACE inhibitors like captopril have similar results. It’s not magic. It’s physics-lower pressure, less damage.
When to Start These Medications
You don’t wait for kidney failure. You start when you see the first signs. According to the American Diabetes Association (2025), if you have diabetes and:
- High blood pressure AND any level of albumin in urine (even mild), or
- eGFR below 60 mL/min/1.73 m², or
- UACR above 300 mg/g creatinine (severe proteinuria)
Then ACE inhibitors or ARBs are not optional-they’re the standard of care. Even if your blood pressure is normal, if you have protein in your urine, these drugs still help. That’s because their kidney protection goes beyond lowering blood pressure.
But here’s the catch: many doctors still don’t start them early enough. Some wait until blood pressure climbs above 140/90. Others delay because they’re afraid of rising creatinine. That’s a mistake.
The Creatinine Myth: Why Rising Numbers Don’t Mean You Should Stop
It’s common to see a 20% to 30% rise in serum creatinine after starting an ACE inhibitor or ARB. Many patients panic. Some doctors stop the drug. Don’t.
This rise isn’t kidney damage-it’s a sign the drug is working. Lowering pressure inside the glomeruli reduces filtration, which temporarily raises creatinine. It’s like slowing down a clogged sink to prevent overflow. If you stop the medication because creatinine went up, you’re removing the very thing protecting your kidneys.
The ADA says clearly: if creatinine rises less than 30% and you’re not dehydrated, keep going. Maximize the dose. This isn’t theoretical. Clinical trials used high doses-captopril 25 mg three times daily, ramipril up to 20 mg daily-and that’s what delivered results. Most patients in real life get half that. That’s why so many still progress to kidney failure.
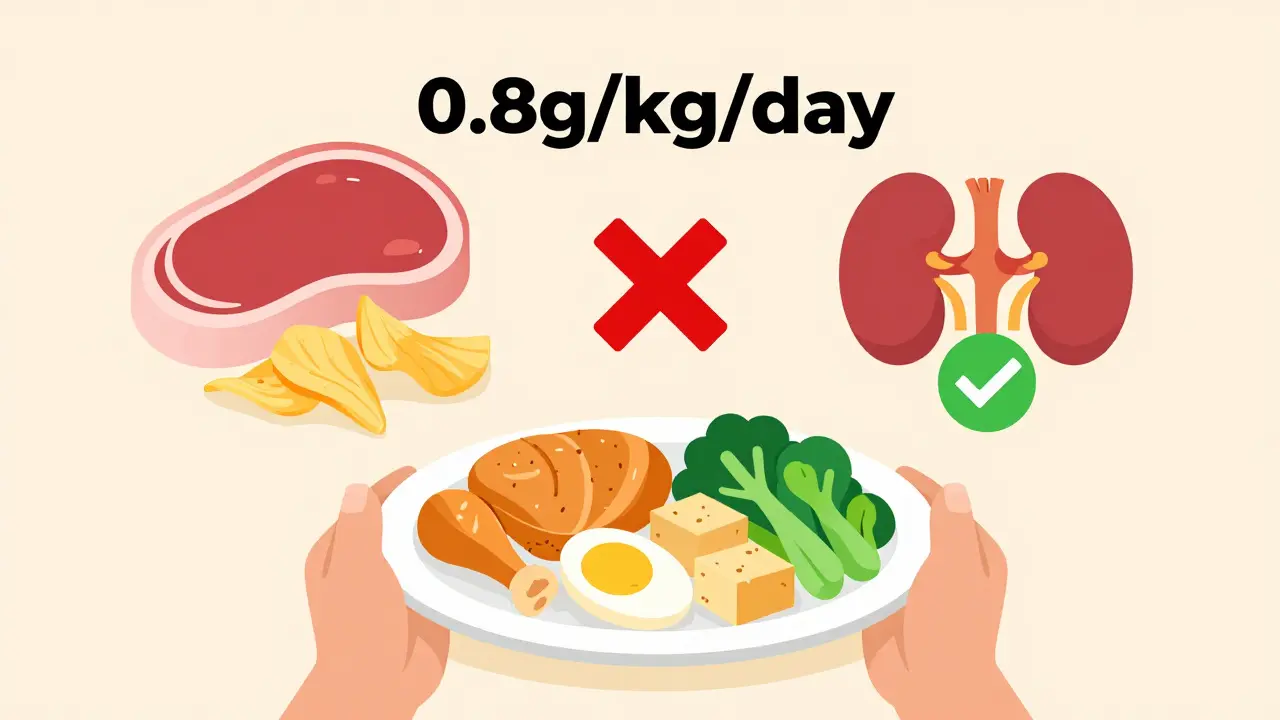
Protein Control: What You Eat Matters Just as Much
Medications help, but your plate matters too. Eating too much protein forces your kidneys to work harder. In diabetic nephropathy, that extra load speeds up damage.
Current guidelines suggest keeping protein intake at 0.8 grams per kilogram of body weight per day. For a 70 kg person, that’s about 56 grams daily. That’s not a low-protein diet-it’s a balanced one. Think: one palm-sized portion of chicken or fish per meal, a couple of eggs, a small serving of beans or tofu, and dairy in moderation.
Don’t fall for high-protein fads. They’re dangerous here. A 2023 review in the Journal of the American Society of Nephrology showed that excessive protein intake (over 1.2 g/kg/day) accelerated decline in people with early diabetic kidney disease, even when blood sugar and blood pressure were controlled.
And don’t forget sodium. Salt raises blood pressure and makes proteinuria worse. Aim for under 2,300 mg per day. That means skipping processed foods, canned soups, and salty snacks. Cook at home. Use herbs, lemon, garlic-not salt.
Why You Shouldn’t Mix ACE Inhibitors and ARBs
You might think doubling up would help more. It doesn’t. It hurts.
Trials like VA NEPHRON-D and ONTARGET tested combining an ACE inhibitor with an ARB. The results were clear: no extra kidney protection. But the side effects? Huge. Hyperkalemia (dangerously high potassium) doubled. Acute kidney injury tripled. More hospital stays. More risks. No benefits.
The same goes for adding direct renin inhibitors like aliskiren. The ALTITUDE trial showed it increased complications without slowing disease. Stick to one RAAS blocker-either an ACE inhibitor or an ARB-but use it at the highest dose your body can handle.
What About Newer Drugs Like SGLT2 Inhibitors?
Drugs like empagliflozin and dapagliflozin have shown amazing kidney protection in recent trials. But here’s the critical detail: every major study tested them in people already on ACE inhibitors or ARBs. Not instead of them.
That means SGLT2 inhibitors are powerful add-ons-not replacements. If you can’t tolerate an ACE inhibitor or ARB due to cough, dizziness, or high potassium, then yes, an SGLT2 inhibitor becomes your first-line kidney protector. But if you can take a RAAS blocker, use it first. Then add the SGLT2 inhibitor on top.
Same goes for finerenone, a new nonsteroidal mineralocorticoid receptor antagonist. It works best when RAAS blockers are already in place. These newer drugs are upgrades, not replacements.

What to Avoid: NSAIDs, Diuretics, and Other Risks
Many people with diabetes also take ibuprofen or naproxen for joint pain. Big problem. NSAIDs reduce blood flow to the kidneys. When combined with ACE inhibitors or ARBs, that can cause sudden, severe kidney injury-especially in older adults or those with already reduced kidney function.
Diuretics like furosemide (Lasix) are sometimes needed for swelling or heart failure. But they can lower blood volume, which makes ACE inhibitors and ARBs riskier. If you’re on both, your doctor needs to monitor you closely for low blood pressure and rising creatinine.
And never start a new medication without telling your doctor you’re on an ACE inhibitor or ARB. Even over-the-counter supplements like licorice root or potassium supplements can be dangerous.
Real-World Gaps: Why So Many People Are Still at Risk
Despite decades of evidence, only about 60% to 70% of people with diabetic kidney disease are on guideline-recommended therapy. Why?
- Doctors fear creatinine spikes and stop the drug too soon.
- Patients stop because of dry cough (ACE inhibitors) or dizziness.
- Some think, “I feel fine,” so they skip the pill.
- Others are prescribed low doses because it’s cheaper or easier.
Here’s the truth: if you’re not on a maximally tolerated dose of an ACE inhibitor or ARB, you’re not getting the full benefit. That’s not just suboptimal care-it’s preventable kidney failure.
What to Do Next: A Simple Action Plan
If you have diabetes and haven’t had a urine test for albumin in the last year-get one. If you have high blood pressure and protein in your urine, ask your doctor: “Am I on the right dose of an ACE inhibitor or ARB?”
Here’s what to ask for:
- Your UACR (urine albumin-to-creatinine ratio) and eGFR numbers from your last blood and urine tests.
- The exact name and dose of your RAAS blocker.
- Whether your dose is at the maximum tolerated level.
- Whether your protein intake is in the safe range (0.8 g/kg/day).
- Whether you’re taking NSAIDs or other risky meds.
Don’t wait for symptoms. Don’t wait for dialysis. The window to protect your kidneys is now-and the tools are proven.
Final Thought: This Isn’t About Drugs Alone
Diabetic nephropathy isn’t just a kidney problem. It’s a signal that your whole system is under stress. Blood sugar control, blood pressure, diet, exercise, and medication all work together. But if you only take one action to protect your kidneys, make it this: start or optimize your ACE inhibitor or ARB at the highest dose you can tolerate-and keep it going, no matter what the creatinine says.
Because your kidneys don’t just filter waste. They keep you alive. And you’ve got the power to protect them.
Can ACE inhibitors or ARBs prevent diabetic nephropathy in people with normal kidney function?
No. Current guidelines from the American Diabetes Association and NIH state that ACE inhibitors and ARBs should not be used for primary prevention in people with diabetes who have normal blood pressure and no protein in their urine. Studies, including one with enalapril in normotensive type 1 diabetics, showed no benefit in preventing kidney damage in this group. These drugs are only recommended once early signs of kidney involvement appear-like microalbuminuria or high blood pressure.
Why do some people get a cough from ACE inhibitors but not ARBs?
ACE inhibitors block the enzyme that breaks down bradykinin, a substance that can build up and irritate the airways, causing a dry, persistent cough. ARBs don’t affect bradykinin, so they don’t cause this side effect. If you develop a cough on an ACE inhibitor, switching to an ARB is the standard solution-and you’ll still get the same kidney protection.
How long does it take for ACE inhibitors or ARBs to reduce protein in urine?
You usually see a reduction in proteinuria within 4 to 8 weeks of starting the medication. The full kidney-protective effect takes longer-often 6 to 12 months. That’s why it’s important not to stop the drug too early if you don’t feel immediate changes. The benefit is long-term, not instant.
Can I stop taking ACE inhibitors or ARBs if my blood sugar improves?
No. Even if your blood sugar is well controlled, the kidney damage from years of high glucose doesn’t reverse overnight. ACE inhibitors and ARBs work by reducing pressure inside the kidney’s filters, which continues to protect your kidneys regardless of current blood sugar levels. Stopping them increases your risk of progression to kidney failure. These medications are long-term, often lifelong, treatments for diabetic nephropathy.
Are there any natural alternatives to ACE inhibitors or ARBs for kidney protection?
There are no proven natural alternatives that match the kidney-protective effects of ACE inhibitors or ARBs in diabetic nephropathy. While lifestyle changes like low-sodium diets, regular exercise, and avoiding processed foods help, they don’t replace these medications. Supplements like omega-3s or antioxidants have not been shown to reduce proteinuria or slow kidney decline in robust clinical trials. Relying on them instead of proven drugs puts your kidneys at serious risk.
Aliza Efraimov
December 29, 2025 AT 05:53I was diagnosed with type 2 diabetes five years ago and didn’t even know my kidneys were at risk until my nurse pulled me aside after a routine check-up. I had microalbuminuria-just barely-but my doctor wanted to wait. I pushed back. Read this post. Went in with printouts. They started me on losartan that week. Two years later, my UACR is half what it was. This isn’t theory. It’s my life.
And no, I don’t care if my creatinine went up 25%. I know what that means now. I’m not stopping.
Also, I cut out processed snacks. Swapped bread for cauliflower rice. Lost 30 pounds. My A1c’s 5.9. But the ARB? That’s what saved my kidneys. Not the diet alone. Not the exercise. The drug.
If you’re hesitating? Stop. Just start. Your future self will thank you.
PS: I cry every time I take my pill now. Not because it’s hard. Because I know what it’s protecting.
Nisha Marwaha
December 29, 2025 AT 07:55From a nephrology fellow in Mumbai: this is textbook, but let me reinforce the clinical nuance. The RENAAL and IDNT trials established ARBs as first-line in T2DM with macroalbuminuria, but the real paradigm shift came with the CREDENCE trial-where canagliflozin added benefit on top of ACEi/ARB. That’s the new standard: dual-pathway protection.
Protein restriction at 0.8 g/kg/day remains evidence-based, but in resource-limited settings, we prioritize RAAS blockade over dietary perfection. A patient on optimal ARB with 1.2 g/kg protein still has better outcomes than one on subtherapeutic ARB with perfect protein intake.
And yes-NSAIDs are the silent killers in diabetic nephropathy. We see it every month. One ibuprofen for a headache, then AKI in 48 hours. Always ask about OTCs.
Tamar Dunlop
December 30, 2025 AT 08:58As a Canadian with type 1 diabetes since age 12, I’ve watched my kidneys slowly deteriorate over two decades. I was on captopril for 15 years-until the cough became unbearable. Switched to irbesartan. No cough. Same protection. Same peace of mind.
I want to thank the author for emphasizing that this isn’t about feeling better-it’s about preventing dialysis. My brother started dialysis at 41. He didn’t believe the ‘silent’ part until it was too late. I carry his story with me every time I take my pill.
Also, please don’t let anyone tell you that ‘natural remedies’ can replace this. I’ve seen too many people turn to herbal teas and detoxes while letting their UACR climb. It’s heartbreaking.
To those reading this: your kidneys don’t scream. They whisper. Listen. Now.
With deep gratitude,
Tamar
Emma Duquemin
December 31, 2025 AT 03:02Okay, I’m not a doctor, but I’m a data nerd who survived diabetic nephropathy because I refused to be passive. I tracked my UACR like it was my Netflix rating. I set alarms to take my benazepril. I made a spreadsheet of every meal to hit 0.8g/kg protein (yes, I weighed my chicken).
And guess what? My creatinine spiked 28% after starting the med. I panicked. Called my nephrologist at 11pm. She laughed. Said, ‘Good. That means it’s working.’
Then I found out SGLT2 inhibitors were an add-on, not a replacement. So I asked for empagliflozin. Now I’m on both. My eGFR’s stable. My proteinuria’s down 40%.
If you’re not doing this? You’re playing Russian roulette with your kidneys. And no, ‘I feel fine’ is not a valid medical strategy.
Also-stop eating salt. Your taste buds will survive. Your kidneys won’t.
Kevin Lopez
January 1, 2026 AT 18:55RAAS blockade = standard of care. No debate. If you’re not on max-dose ACEi/ARB with proteinuria, you’re getting substandard care. Period.
NSAIDs = contraindicated. SGLT2i = adjunct. Not replacement.
Protein restriction >1.2g/kg accelerates decline. Evidence level 1.
Stop listening to influencers. Start listening to guidelines.
Duncan Careless
January 2, 2026 AT 19:34Thanks for this. Really helpful. I’ve been on ramipril for 3 years now. My creatinine went up a bit at first-I was terrified. But my GP told me to wait. And now, after 2 years, it’s stable. I didn’t know about the 30% rule-glad I didn’t quit.
Also, I didn’t realize salt made proteinuria worse. I’ve been eating a lot of canned soups. Gonna switch to homemade. Maybe I’ll try garlic and lemon like you said.
Appreciate the clarity. I feel less alone now.
Samar Khan
January 4, 2026 AT 10:30OMG I’m crying rn 😭😭😭
I thought my kidney thing was just ‘normal’ for diabetics. I didn’t know it was preventable. I’ve been on low-dose lisinopril for 2 years but never got it checked. My UACR is 600. I’m 34. I have a 3-year-old. I’m so scared.
My doctor said ‘maybe increase the dose’ but I didn’t push. Now I feel so guilty.
Can I still fix this? I’ll do anything. Please tell me I’m not too late. 😭😭😭
Also, I eat like a garbage fire. I’m so sorry. 😭
Russell Thomas
January 5, 2026 AT 07:39Oh wow. Another ‘kidney protection’ post. Let me guess-you’re also going to tell me to stop eating bread and take pills I don’t need? Because my ‘creatinine went up’? That’s not protection, that’s pharmaceutical propaganda.
I’ve been on ACE inhibitors for 10 years. My kidneys are fine. I don’t need your lecture. I don’t need your protein math. I don’t need your ‘max dose’ nonsense.
My grandma lived to 92 eating bacon and donuts. You think your lab values matter more than real life?
Also, ‘no natural alternatives’? What about turmeric? Apple cider vinegar? I’ve seen videos. You’re just scared people will stop buying pills.
Go sell your meds somewhere else, doc.
Joe Kwon
January 6, 2026 AT 00:24I appreciate all the perspectives here. Samar, you’re not alone in feeling scared-your reaction is valid. And Russell, I get why you’re skeptical, but the data is overwhelming: RAAS blockade reduces ESRD risk by 30%. That’s not marketing. That’s life-saving.
For those asking if it’s too late: no. Even if you’re at UACR 600, starting max-dose ARB + SGLT2i can still slow progression dramatically. I’ve seen it.
And Nicole? You’re right to be frustrated. The system fails people every day. Doctors delay. Patients don’t know. But this post? It’s a tool. Use it to ask better questions.
One step. One pill. One meal. That’s how you rebuild trust-with your body, your doctor, yourself.
💙
Nicole K.
January 6, 2026 AT 00:53This whole post is just a scam to sell drugs. People have been getting by for centuries without these pills. Now everyone’s scared of their own kidneys. You’re making people paranoid. Just eat less sugar and pray. That’s what my grandma did. She lived to 95.
Also, why do you always say ‘don’t stop’? What if I want to stop? Why can’t I make my own choices?
You people act like medicine is the only answer. It’s not. It’s control. And control is evil.
Aliza Efraimov
January 6, 2026 AT 13:57To Samar: you’re not too late. I was at 580 too. Started losartan 150mg + empagliflozin 10mg. My UACR is now 210. I’m not cured. But I’m not dying. You can do this. One pill at a time.
To Russell: I get it. You think this is all corporate. But my brother died on dialysis at 41. He didn’t take the pills. He didn’t change his diet. He thought ‘natural’ was enough. He’s gone.
This isn’t about control. It’s about not losing the people you love.
I’m not selling anything. I’m just sharing what saved me.