Cost vs Benefit: When Expensive Medications Make Sense Despite Side Effects
 Dec, 17 2025
Dec, 17 2025
Medication Cost-Benefit Calculator
Determine if expensive medications make sense for your situation. Based on the article's framework, this calculator assesses whether a drug's benefits outweigh its costs using standard healthcare value metrics.
Results
When a drug costs more than your car payment - or your rent - it’s natural to ask: is this worth it? Especially when the side effects are bad, the insurance won’t cover it fully, and you’re left choosing between medicine and groceries. But sometimes, the answer isn’t simple. For some people, taking a $500,000 gene therapy or a $10,000-a-month biologic isn’t a luxury. It’s the only thing standing between them and death, disability, or years of unbearable pain.
Why Do Some Drugs Cost So Much?
Not all expensive drugs are created equal. The most costly ones usually fall into three buckets: cancer treatments, rare disease therapies (called orphan drugs), and cutting-edge biologics like CAR-T cell therapy. These aren’t just fancy versions of old pills. They’re often designed for tiny groups of people - sometimes fewer than 1,000 in the whole country. That means the manufacturer has to recoup billions in research costs from just a few hundred patients.
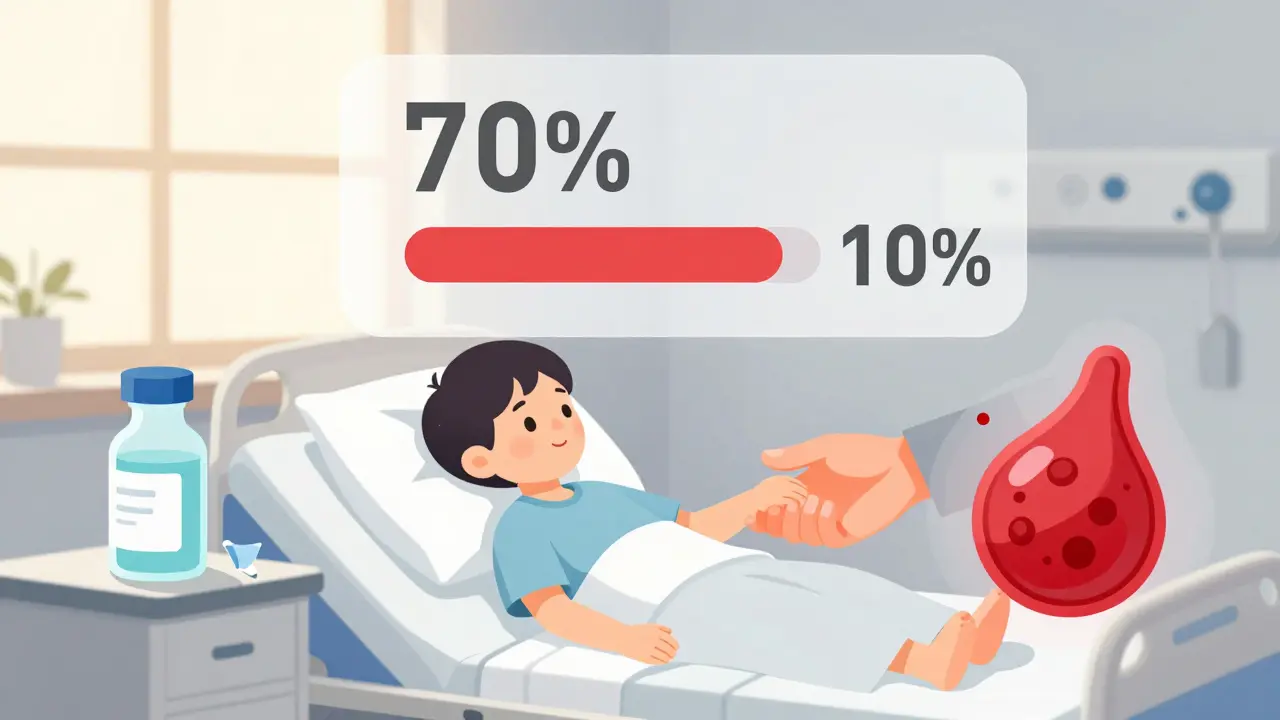
Take tisagenlecleucel, a CAR-T therapy for certain types of leukemia. At $475,000 per treatment, it’s one of the priciest drugs in the world. But for kids who’ve run out of chemo options, it can mean a 70% chance of long-term remission. Compare that to the old standard: more rounds of toxic chemotherapy, hospital stays, and a 10% survival rate. The cost is staggering, but so is the difference it makes.
Then there’s hepatitis C drugs like Harvoni. In 2016, a full course cost over $80,000. But before Harvoni, treatment meant weekly injections, months of flu-like symptoms, and only a 50% cure rate. Harvoni cured 95% of patients in just 12 weeks - with almost no side effects. Even at that price, it saved money long-term by preventing liver failure, transplants, and cancer.
Side Effects Aren’t Always the Deal-Breaker
Let’s be honest: most expensive drugs come with baggage. Cytokine release syndrome from CAR-T therapy can land you in the ICU. Biologics for rheumatoid arthritis can leave you vulnerable to infections. Some drugs cause nausea, fatigue, or nerve damage. But here’s the thing - side effects aren’t always worse than the disease itself.
Think about emicizumab, a drug for severe hemophilia. Before it came along, patients needed IV infusions three times a week to stop bleeding. Many ended up with joint damage, chronic pain, and limited mobility. Emicizumab is a weekly injection. Side effects? Mild bruising or headaches. But the benefit? Almost zero spontaneous bleeding. Patients went from wheelchairs to hiking. The monthly cost? Around $15,000. But the cost of not using it? Lifelong disability.
For someone with advanced multiple sclerosis, a $12,000-a-month drug might cause dizziness and fatigue. But if it stops new brain lesions from forming and keeps them walking, working, and caring for their kids - the trade-off isn’t just acceptable. It’s life-changing.
How Do You Know If It’s Worth It?
There’s no universal rule. But there are three questions that help cut through the noise:
- Is this drug actually better than what’s already available? Many new drugs are barely better - just slightly more effective or slightly safer. In 2023, Prescrire International found only 7 out of 100 new drugs offered real progress. If your doctor is pushing a new $10,000 drug and the old one works fine, ask why.
- What’s the long-term impact? A drug that costs $200,000 but prevents a $1 million organ transplant? That’s a win. A drug that extends life by two months with heavy side effects? Maybe not.
- What happens if you don’t take it? For some, the answer is death. For others, it’s worsening pain, loss of independence, or hospitalization. If skipping the drug means losing your ability to live - not just survive - then the cost isn’t just financial. It’s personal.
There’s also data to back this up. In the U.S., the typical threshold for “value” is $50,000 to $150,000 per quality-adjusted life year (QALY). That’s a fancy way of saying: how much does it cost to give someone one more year of healthy life? If a drug costs $300,000 but adds five healthy years? That’s $60,000 per year - within the range many experts consider reasonable. But if it costs $300,000 and adds only six months? That’s $600,000 per year - hard to justify.
Insurance, Copays, and the Hidden Costs
Even if a drug makes clinical sense, the out-of-pocket cost can be crushing. Medicare Part D patients without financial help spent up to $5,700 a year just for drugs like ruxolitinib. Some patients skip doses. Others choose between medicine and food. In 2022, nearly 7 out of 10 people taking drugs over $10,000 a month admitted to cutting back because of cost.
But help exists. Manufacturer patient assistance programs cover an average of 40% of out-of-pocket costs for commercially insured patients. Foundations like the Chronic Disease Fund gave over $2 billion in aid in 2022. Specialty pharmacies often assign case managers who spend hours negotiating with insurers - something you don’t have to do alone.
And don’t assume the sticker price is the real price. Most drugs have secret discounts and rebates that insurers get - but patients never see. That’s why a drug listed at $10,000 might actually cost the insurer $4,000. You still pay your copay based on the high list price, though. That’s broken. But knowing it exists helps you ask the right questions.
When to Push Back
Not every expensive drug deserves a yes. If your doctor says, “This is the newest option,” but doesn’t explain how it’s better than what you’re on - push back. Ask for data. Ask for comparisons. Ask what happens if you wait or try a cheaper alternative first.
Some drugs are approved based on small studies with weak evidence. In Europe, 56% of the most expensive drugs were rated as having low benefit by health agencies. The U.S. doesn’t have that kind of review. So you have to be your own advocate.
Ask: “Is this drug proven to help people live longer, feel better, or avoid hospital stays?” If the answer is “it shrinks tumors” but doesn’t extend life - that’s not enough for most people. Tumor shrinkage sounds good, but if you’re still dying in six months, it’s not a win.

What’s Changing in 2025?
For the first time, Medicare is starting to negotiate prices for 10 of the most expensive drugs in 2026. That’s a big deal. But only 4% of ultra-expensive drugs qualify right now. Most are excluded because they’re too new, too rare, or too profitable for manufacturers.
Meanwhile, the EU is rolling out a new system that requires all new drugs to be assessed across multiple countries before approval. That means better data, fewer overpriced duds, and more transparency.
But until those systems catch up, the burden still falls on patients and families. You’re not just paying for a pill. You’re paying for hope. And sometimes, that’s worth everything.
Real Stories, Real Choices
One woman in Ohio, 58, with aggressive lymphoma, had tried six rounds of chemo. Nothing worked. Her oncologist offered CAR-T. The cost? $475,000. Her insurance covered most of it, but she’d still owe $25,000. She sold her car. Took out a second mortgage. Said she’d rather die broke than die sick. Two years later, she’s cancer-free.
A man in Texas with Crohn’s disease spent 12 years on steroids and infusions. His joints were destroyed. His weight dropped to 110 pounds. His new biologic cost $14,000 a month. He got a grant from a nonprofit. Within three months, he gained 30 pounds. He started walking again. He went back to work. He says the side effects - occasional headaches - are the price of being alive.
These aren’t rare cases. They’re the reality for thousands. The question isn’t whether the drug is expensive. It’s whether not taking it is more expensive - in pain, in time, in life.
Are expensive medications always worth the cost?
No. Many high-cost drugs offer only small improvements over cheaper alternatives. The key is to ask: Does this drug significantly improve survival, quality of life, or prevent serious complications? If it only shrinks a tumor without extending life, or replaces one set of side effects with another, it may not be worth it. Always compare it to existing treatments.
What if I can’t afford the medication even with insurance?
You’re not alone. Many manufacturers offer patient assistance programs that can reduce your out-of-pocket costs by 40% or more. Nonprofits like the Chronic Disease Fund and Patient Access Network Foundation provide grants. Specialty pharmacies often assign case managers who help navigate coverage. Don’t give up - ask your doctor or pharmacist for help finding these programs.
Do side effects make expensive drugs unsafe?
Not necessarily. Side effects are part of the trade-off. For example, CAR-T therapy can cause dangerous inflammation, but for patients with no other options, it’s often the only path to remission. The real question is: Are the side effects worse than the disease? If your condition causes chronic pain, disability, or early death, then the drug’s side effects may be a fair exchange.
Why are some drugs so much more expensive in the U.S. than in other countries?
The U.S. doesn’t negotiate drug prices like most other countries. In Europe and Canada, health agencies review a drug’s value before approving it for public use. If the price is too high for the benefit, they refuse to pay. The U.S. lets manufacturers set prices with little oversight. That’s why the same drug can cost 3-5 times more here.
Can I ask my doctor to try a cheaper drug first?
Absolutely. Many insurance plans require you to try cheaper options first (called step therapy). Even if your doctor recommends an expensive drug, ask: “Is there a proven, lower-cost alternative?” Sometimes the answer is yes. And if not, they should explain why the expensive option is truly necessary - not just new.
How do I know if a new drug is actually better or just heavily marketed?
Look beyond the ads. Check independent reviews from groups like Prescrire International or the Institute for Clinical and Economic Review (ICER). These organizations analyze real-world data and rate drugs on actual benefit, not hype. If a drug was approved based on a small trial with no long-term results, be skeptical. Ask your doctor for the evidence - not the sales pitch.
What to Do Next
If you’re considering an expensive medication:
- Ask your doctor for a written comparison: how does this drug compare to others in effectiveness, side effects, and cost?
- Call your insurer and ask for the net cost after rebates - not the list price.
- Search for patient assistance programs using your drug’s name + “patient assistance.”
- Ask if your pharmacy has a specialty case manager - they can help with appeals and funding.
- Don’t rush. If it’s not an emergency, take time to research. Many drugs have waiting lists for financial aid.
There’s no shame in asking for help. The system is broken. But you don’t have to navigate it alone. The goal isn’t to pay less - it’s to get better. And sometimes, that means paying more. But only when it truly matters.
Mark Able
December 19, 2025 AT 04:59I don't care how much it costs - if it keeps me alive, I'll sell my damn kidney. My cousin took that CAR-T stuff, lost all her hair, spent two weeks in the ICU, but she's hiking in Colorado now. That's not a drug, that's a second chance. Why are we even debating this?
Chris Clark
December 19, 2025 AT 22:37lol at people actin like $500k is a lot for a cure. i had a friend get treated for hep c back in 2016 - same price, 12 weeks, no side effects, 95% cure rate. now he’s got a liver that works. the real ripoff is when you pay $10k a month for a drug that just slows you down a lil. not all expensive shit is magic, yk?
Dorine Anthony
December 21, 2025 AT 06:46I just want to say thank you for writing this. My mom’s on that emicizumab for hemophilia. We thought we were gonna lose her to bleeding out by 40. Now she dances at my wedding. The side effects? Mild bruising. The cost? We cried the first month. But we’re not crying anymore. This isn’t about money - it’s about being there.
William Storrs
December 21, 2025 AT 09:21You’re not alone in this. If you’re reading this and scared about affording treatment - reach out. There are programs. There are people who will help. You don’t have to fight this alone. I’ve seen people go from wheelchairs to walking again. Don’t give up. Ask for help. It’s out there. You deserve to live.
James Stearns
December 22, 2025 AT 10:35It is an incontrovertible fact that the current pharmaceutical pricing paradigm in the United States constitutes a systemic failure of market regulation, predicated upon the exploitation of vulnerable patient populations through the strategic manipulation of intellectual property rights and the absence of centralized price negotiation mechanisms. The moral hazard inherent in this structure is not merely lamentable - it is indefensible.
Nina Stacey
December 22, 2025 AT 14:17So like… I get that some drugs save lives but like… why do we let companies charge like 10x what it costs to make it? Like I know they need to make money but also like… my friend took a drug that cost 12k a month and it gave her headaches and made her tired but she was able to work again so like… I guess it’s worth it but also like… why is this even a thing in 2025
Dominic Suyo
December 24, 2025 AT 13:09Let’s be real - the pharma industry is a glorified lottery where patients are the suckers and shareholders are the winners. CAR-T? $475K. That’s not medicine, that’s a ransom note written in clinical trial data. And don’t get me started on the ‘patient assistance’ fairy tales - it’s just PR spin wrapped in a nonprofit bow. The system is rigged. We’re just haggling over how much blood to bleed out.
Kevin Motta Top
December 26, 2025 AT 01:03My dad’s on a $14k/month drug. Insurance covers 80%. We pay $2,800. We’re broke. But he walks. He cooks. He plays with his grandkids. No drug is worth it if you’re dead. But if you’re alive? That’s the only math that matters.