Coronary Artery Disease: Atherosclerosis, Risk Factors, and Treatments
 Feb, 7 2026
Feb, 7 2026
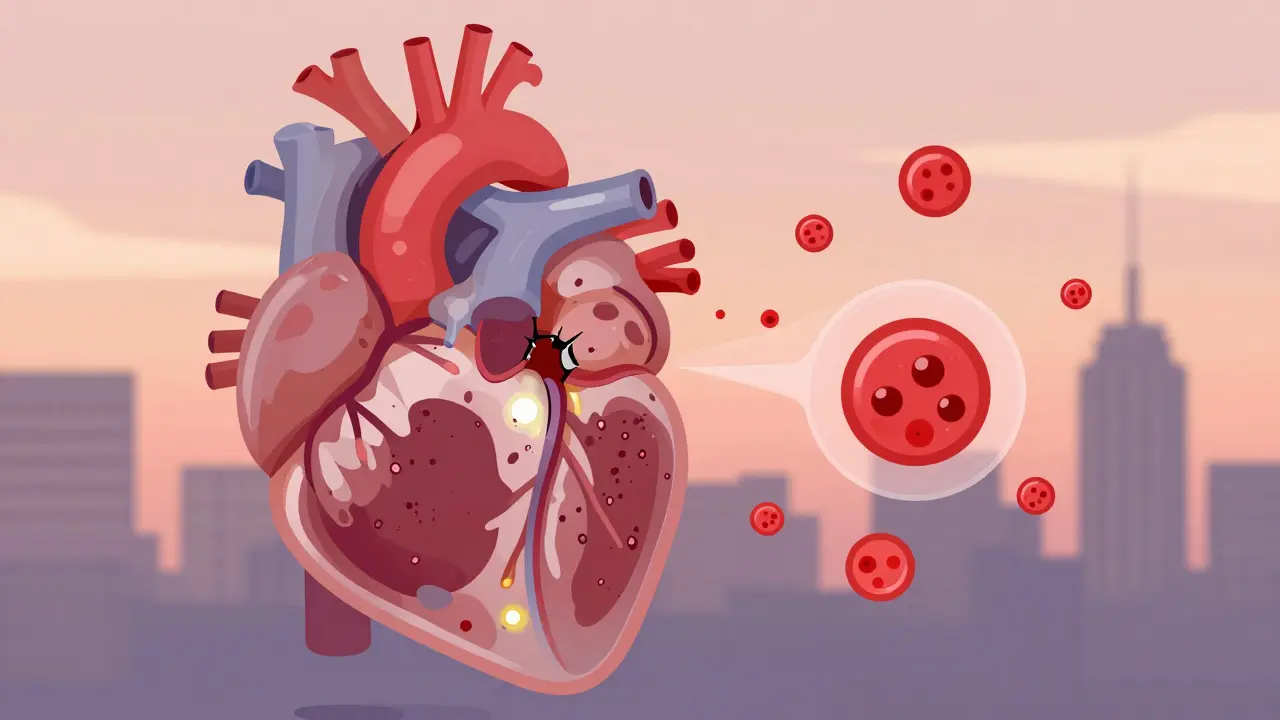
Coronary artery disease isn't just a buzzword in medical journals-it's the number one killer worldwide. Every year, over 18 million adults in the U.S. alone live with it, and it claims about 360,900 lives annually. Behind this statistic is a slow, silent process: fatty deposits clogging the very arteries that feed your heart. This isn't about being out of shape or eating one too many burgers. It's about biology, inflammation, and how your body responds over decades to lifestyle, genetics, and environment. Understanding how it starts, who's at risk, and what actually works to stop it can save your life-or someone you love.
What Exactly Is Atherosclerosis?
Atherosclerosis is the root of coronary artery disease. It's not just "plaque" in a vague sense. It's a living, changing buildup inside your arteries made of cholesterol, fat, calcium, and immune cells. These plaques don't just sit there. They grow slowly, sometimes for decades, before they cause symptoms. And here's the scary part: the most dangerous plaques aren't always the biggest ones. Unstable plaques have a thin outer shell, a big oily core, and lots of inflammatory cells. They might only block 30% to 40% of the artery-but they can rupture without warning. When they do, a blood clot forms on the spot, suddenly cutting off blood flow to part of the heart. That's a heart attack. Stable plaques, on the other hand, grow thicker and harder over time. They might block more than 70% of the artery, but they don't rupture as easily. These cause predictable chest pain during exertion-stable angina-but they're easier to manage. The process starts with damage to the inner lining of the artery, often from high blood pressure, smoking, or too much LDL (bad) cholesterol. Once the lining is injured, LDL particles slip in, get oxidized, and trigger inflammation. White blood cells rush in, swallow the fat, and turn into foam cells. Over time, smooth muscle cells and calcium build up around them, forming a fibrous cap. That cap is what determines whether the plaque is ticking time bomb or a slow-burning problem.Who’s Really at Risk?
Risk factors for coronary artery disease aren't just "high cholesterol" or "smoking." They're layered. Some you can change. Others you can't. But knowing which ones apply to you helps you act before it's too late.- High LDL cholesterol: Levels above 190 mg/dL are a major red flag. LDL isn't just "bad"-it's the main fuel for plaque.
- High blood pressure: Consistently above 130/80 mm Hg damages artery walls over time. This is why even "pre-hypertension" matters.
- Diabetes: People with diabetes have a risk of heart disease equal to someone who already had a heart attack. High blood sugar fries blood vessels from the inside.
- Smoking: One pack a day for 10 years increases CAD risk by 2 to 4 times. Quitting cuts that risk in half within a year.
- Obesity: A BMI over 30 raises risk independently, even if cholesterol and blood pressure look fine.
- Family history: If a parent had heart disease before age 55 (men) or 65 (women), your risk doubles.
- Chronic kidney disease: An eGFR below 60 ml/min is a strong predictor of future heart events.
- Atrial fibrillation: This irregular heartbeat isn't just about stroke-it's tightly linked to coronary artery disease.
How Is It Diagnosed?
Many people don’t know they have coronary artery disease until they have chest pain, shortness of breath, or a heart attack. But there are ways to catch it early.- Electrocardiogram (ECG): This simple test checks your heart’s electrical rhythm. It can show signs of past damage or ongoing stress.
- Stress test: You walk on a treadmill or take medicine to make your heart work harder while doctors monitor your ECG, blood pressure, and symptoms. If your heart doesn’t get enough oxygen during stress, it shows up on the test.
- Coronary angiography: This is the gold standard. A thin tube is threaded into your artery, dye is injected, and X-rays show exactly where blockages are. It’s invasive, but it’s the only way to see the full picture.
- Ankle-Brachial Index (ABI): This quick test compares blood pressure in your ankle and arm. A low number means you likely have artery disease in your legs-which often means you have it in your heart too.
What Actually Works in Treatment?
There’s no magic pill. But there are proven, science-backed strategies that work-when used together.Lifestyle: The Foundation
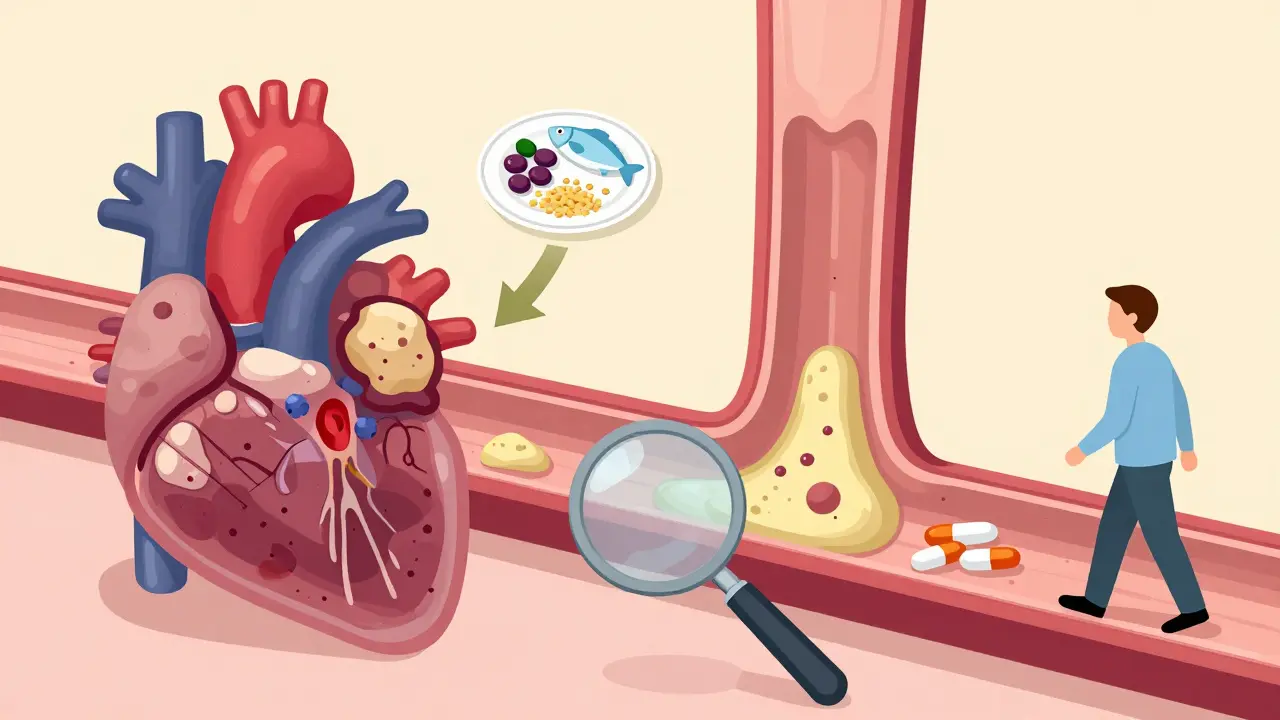
Medications help, but they don’t fix the root cause. The biggest impact comes from:- Heart-healthy diet: Focus on vegetables, whole grains, fish, nuts, and legumes. Cut back on processed meats, sugary drinks, and refined carbs. The Mediterranean diet has been shown to reduce heart events by 30% in high-risk people.
- Exercise: At least 150 minutes a week of brisk walking, cycling, or swimming. Even 10-minute bursts help. Moving regularly improves blood flow, lowers blood pressure, and reduces inflammation.
- Quitting smoking: No other single change cuts heart disease risk faster.
- Weight loss: Losing just 5% to 10% of body weight can improve blood pressure, cholesterol, and insulin sensitivity.
Medications
These aren’t optional for most people with CAD-they’re essential.- Statins: Lower LDL cholesterol by 30% to 50%. They also stabilize plaques and reduce inflammation. Even if your LDL is "normal," statins are often recommended for people with CAD.
- Antiplatelets: Aspirin or clopidogrel prevent blood clots. For people with a history of heart attack or stent placement, these are lifelong.
- Beta-blockers: Reduce heart rate and blood pressure, lowering oxygen demand on the heart. Especially helpful after a heart attack.
- ACE inhibitors or ARBs: Lower blood pressure and protect the heart muscle. Recommended for people with diabetes, heart failure, or kidney disease.
- PCSK9 inhibitors: Newer injectable drugs for those who can’t get LDL low enough with statins alone. They can drop LDL by 60%.
Procedures
If lifestyle and meds aren’t enough:- Percutaneous Coronary Intervention (PCI): A balloon is inflated in the blocked artery, and a metal mesh stent is placed to keep it open. It’s done through a small incision in the wrist or groin. Recovery is usually under a week.
- Coronary Artery Bypass Grafting (CABG): A surgeon takes a healthy blood vessel from your leg, arm, or chest and reroutes it around the blocked artery. This is for people with multiple blockages, especially if they have diabetes or heart failure.
The Bigger Picture: Chronic Disease and New Frontiers
Coronary artery disease doesn’t happen in isolation. As people live longer, they’re more likely to have cancer, kidney disease, or atrial fibrillation at the same time. That’s why cardio-oncology is now a growing field-treating cancer without wrecking the heart, and treating heart disease without ignoring cancer risks. The 2023 guidelines stress one thing above all: personalized risk assessment. You’re not just "high risk" or "low risk." Your risk is calculated based on your specific combination of factors-diabetes, kidney function, number of blocked arteries, smoking history. That number determines whether you need a single aspirin or a triple therapy of statin, antiplatelet, and blood pressure drug. And here’s what most people don’t realize: you can reverse early atherosclerosis. Studies show that with aggressive LDL lowering (below 70 mg/dL) and lifestyle change, plaques can shrink. It’s not about living with it. It’s about fighting back.What Should You Do Next?
If you’re over 40 and have any risk factors:- Get your LDL, blood pressure, and fasting blood sugar checked.
- If you smoke, quit-today. Talk to your doctor about support programs.
- Start moving. Even a 20-minute walk after dinner helps.
- Ask your doctor: "Based on my history, am I in the high-risk group?"
- If you’ve had a heart attack, stent, or bypass, never stop your meds without talking to your cardiologist.
Can you reverse coronary artery disease?
Yes, in early stages. Aggressive lifestyle changes-like following a Mediterranean diet, exercising regularly, quitting smoking, and lowering LDL cholesterol below 70 mg/dL with statins or PCSK9 inhibitors-can cause plaques to shrink. Imaging studies have shown reductions in plaque volume after 1-2 years of intensive treatment. But once plaques become heavily calcified or cause major blockages, reversal is unlikely. The goal then shifts to stabilizing them to prevent rupture.
Is coronary artery disease the same as a heart attack?
No. Coronary artery disease (CAD) is the underlying condition where arteries narrow due to plaque buildup. A heart attack (myocardial infarction) is a sudden event caused when a plaque ruptures and triggers a blood clot that blocks blood flow to the heart muscle. CAD is the disease. A heart attack is one possible outcome of untreated or unstable CAD.
Do I need to take statins for life if I have CAD?
For most people with established coronary artery disease, yes. Statins aren’t just for lowering cholesterol-they stabilize plaques and reduce inflammation in the artery walls. Stopping them increases the risk of another heart attack, stroke, or death. Even if your LDL looks fine, guidelines recommend continuing statins indefinitely unless there’s a serious side effect or new medical reason to stop.
Can you have CAD without chest pain?
Absolutely. About 30% of people with significant CAD have no chest pain at all. This is more common in women, older adults, and people with diabetes. Symptoms might include fatigue, shortness of breath, nausea, or jaw/back pain during activity. Silent CAD is dangerous because it goes undetected until a heart attack happens.
How does diabetes increase heart disease risk?
High blood sugar damages the lining of arteries, increases inflammation, and makes LDL cholesterol more likely to form plaques. It also impairs the body’s ability to heal blood vessels. People with diabetes have the same heart attack risk as someone who already had one. That’s why diabetes is treated as a "coronary heart disease risk equivalent"-meaning doctors treat it like CAD even before symptoms appear.
Is a stent better than bypass surgery?
It depends. For one or two simple blockages, a stent (PCI) is less invasive and has a faster recovery. For multiple blockages, especially in people with diabetes or reduced heart function, bypass surgery (CABG) offers better long-term survival. Recent studies show CABG reduces the risk of future heart attacks and repeat procedures more than stents in complex cases. The decision is based on the number and location of blockages, overall health, and patient preference.
What’s the difference between stable and unstable angina?
Stable angina happens during physical activity or stress and goes away with rest or nitroglycerin. It’s caused by a fixed blockage. Unstable angina comes on suddenly, even at rest, lasts longer, and doesn’t fully respond to rest or medication. It signals that a plaque is about to rupture-and is a medical emergency. If you experience new, worsening, or unpredictable chest pain, call for help immediately.