Combo Generics vs Individual Components: The Real Cost Difference
 Dec, 30 2025
Dec, 30 2025
When you’re on multiple medications, your doctor might suggest a combo pill-a single tablet with two or more drugs inside. It sounds convenient. Fewer pills to swallow. Easier to remember. But here’s the catch: combo generics aren’t always cheaper than buying the same drugs as separate generic pills. In fact, in many cases, they cost way more.
Why Combo Pills Cost More Than You Think
A 2018 study published in JAMA Internal Medicine looked at 29 branded combination drugs used by Medicare Part D. The researchers found that if patients had taken the same active ingredients as separate generic pills instead of the combo, Medicare would’ve saved $925 million in just one year. That’s not a typo. $925 million. For 29 drugs. Take Janumet, a combo of sitagliptin and metformin. In 2016, Medicare paid an average of $472 for a 30-day supply. Meanwhile, generic metformin alone? At Walmart’s $4 program, it cost $4. Even if you added the cost of generic sitagliptin (which was available at the time), the total would still be under $50. That’s a 90%+ price difference. Another example: Kazano (alogliptin + metformin). The combo cost $425 a month. Generic metformin? Less than $10. The other component? Even if it was brand-new and expensive, it wouldn’t push the total past $100. So why pay $425? The answer lies in how drug pricing works. When a company combines an old, off-patent drug with a new, patented one, they can slap a premium price on the whole thing. The old drug is cheap. The new one is expensive. Together? They become a “high-margin product.” It’s called evergreening-using a combo to extend profits when the original patent expires.The Math Behind the Markup
You’d think two generic drugs added together would cost less than a combo. And usually, they do. But the industry doesn’t always play by those rules. IQVIA, a major pharmaceutical data firm, found that branded combo drugs typically cost about 60% of what two separate brand-name drugs would cost. That sounds good-until you realize that generic versions of those same drugs cost 80-85% less than brand names. So if you’re comparing a combo to two generics, you’re not comparing apples to apples. You’re comparing a luxury SUV to two used bicycles. For example, Entresto (sacubitril/valsartan) is a heart failure combo. The brand-name version costs over $500 a month. Generic valsartan? Around $15. Sacubitril? Still under patent, so it’s expensive-but not $500 expensive. Even if sacubitril costs $300, you’re still paying $200 more than necessary. This isn’t just a U.S. problem. In Europe, Nexlizet (ezetimibe/bempedoic acid) sells for $12 a day in the U.S. and €5 a day in the EU. Ezetimibe has been generic for years. It costs pennies. But because it’s paired with a newer drug, the combo gets a premium price tag.When Combo Pills Make Sense
Not all combos are bad. Sometimes, they’re the right choice. For patients with complex conditions-like type 2 diabetes with high blood pressure or HIV on multiple antivirals-taking one pill instead of three or four can improve adherence. Studies show people are 15-20% more likely to stick to their regimen when they have fewer pills. That matters. Missed doses lead to hospitalizations, which cost way more than the drug itself. The American College of Cardiology found that for certain heart patients, combo pills improved adherence by 25%. That means fewer emergency visits, fewer complications, and better long-term outcomes. If a combo helps you stay healthy, the extra cost might be worth it. But here’s the key: only if you can’t get the same result with separate generics. If your doctor prescribes a combo without checking if cheaper alternatives exist, you’re probably overpaying.
What You Can Do
You don’t have to accept the price tag. Here’s how to take control:- Ask your pharmacist: “Are these drugs available as separate generics?”
- Check prices on GoodRx or SingleCare. Type in each drug individually and compare to the combo.
- Ask your doctor: “Is there a generic alternative for each component?”
- If your insurance denies coverage for the combo, file an appeal. Mention the cost difference and cite the JAMA study.
- Request a “combination drug utilization review” through your pharmacy benefit manager. Many plans have programs to flag overpriced combos.
How Insurance and Formularies Handle Combos
Most Medicare Part D plans don’t automatically cover combo drugs unless you’ve tried the cheaper options first. In fact, 62% of Part D plans require prior authorization for high-cost combos. That means your doctor has to jump through hoops to get approval. Pharmacy benefit managers (PBMs) use “carve-outs” to exclude expensive combos from standard formularies. They push prescribers toward separate generics. Some plans even offer incentives-like lower co-pays-for choosing the cheaper option. But here’s the problem: many doctors don’t know the exact prices. They know the combo is “convenient.” They don’t know that metformin costs $4. Or that amlodipine (a blood pressure drug) is $5 as a generic. So they prescribe the combo without realizing the cost difference.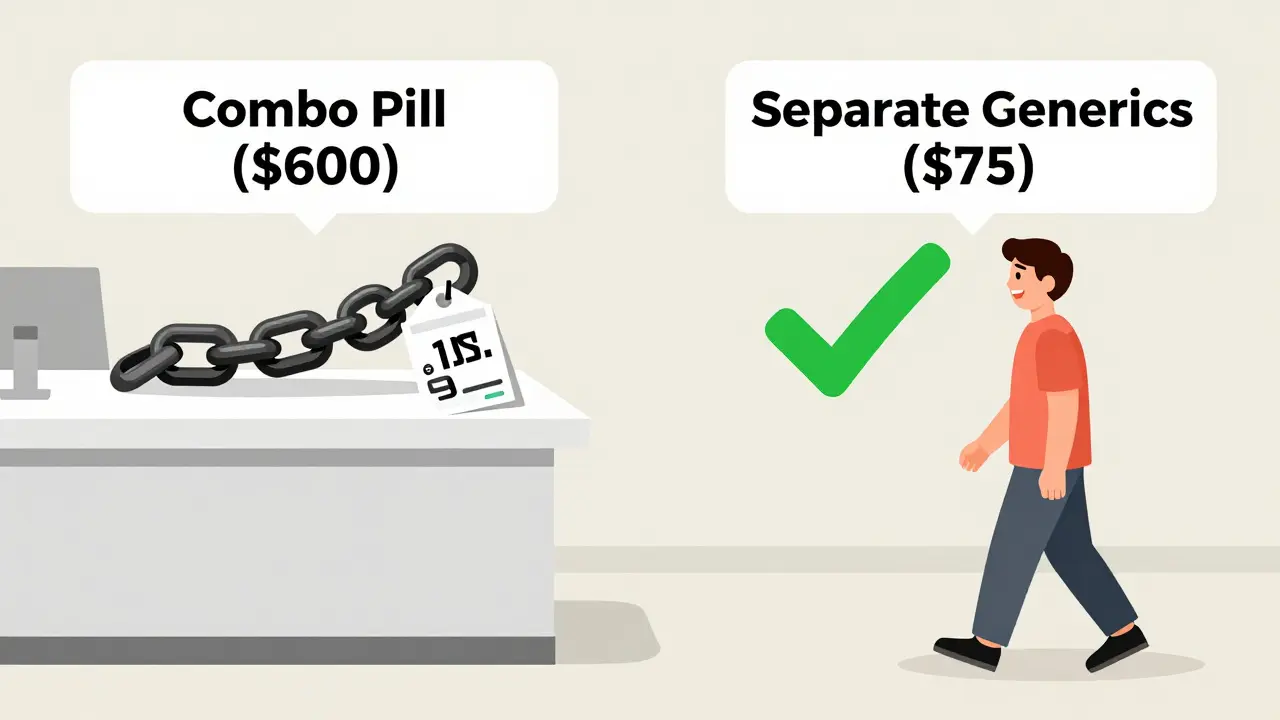
What’s Changing? New Laws and Trends
The Inflation Reduction Act of 2022 gave Medicare the power to negotiate drug prices for the most expensive medications. That includes some combo drugs. Starting in 2026, Medicare will start negotiating prices for 10 combo drugs annually. That could bring down costs significantly. The FDA is also pushing to speed up generic approvals. More generic versions of individual components mean more pressure on combo drug prices. If you can get generic amlodipine, generic atorvastatin, and generic metformin-all cheap-why pay $600 for a combo? Some drugmakers are responding with discount programs. Novartis offers Entresto for $10 a month to eligible Medicare patients. Sounds great-until you realize generic valsartan still costs $15 for the whole month. You’re still paying more than necessary.Bottom Line: Don’t Assume the Combo Is Cheaper
Combo pills aren’t evil. They’re a tool. But they’re being used to extract billions in unnecessary spending. The data is clear: when both drugs in a combo are available as generics, buying them separately almost always saves money. If you’re on a combo drug, ask three questions:- Are both components available as generics?
- What’s the total cost of buying them separately?
- Will my doctor agree to switch if it saves me money?
What to Do Next
1. Make a list of all your medications. Highlight any combos. 2. Go to GoodRx or your local pharmacy’s price checker. Search each drug individually. 3. Add up the total cost of the separate generics. 4. Compare it to your combo’s copay. 5. If the combo costs more than 2x the sum of the generics, ask your doctor about switching. It’s not about rejecting convenience. It’s about not paying for convenience you don’t need.Are combo pills always more expensive than buying separate generics?
No, not always. If both drugs in the combo are still under patent, the combo might be cheaper than buying two brand-name pills. But if one or both drugs are available as generics, the combo is almost always more expensive. In fact, studies show combos can cost 10 to 15 times more than buying the same drugs separately when generics are available.
Why do pharmacies and doctors still prescribe combo pills if they cost more?
Doctors often prescribe combos because they’re convenient and assume they’re cost-effective. Many aren’t aware of exact generic prices. Pharmacies follow formulary rules set by insurance companies, and some combos are preferred because they’re easier to manage in bulk. But that doesn’t mean they’re the cheapest option for you.
Can I ask my doctor to switch me from a combo to separate generics?
Absolutely. You have the right to ask for the most cost-effective option. Bring your price comparison to your appointment. Many doctors will switch you if it’s safe and effective. Studies show switching to generics doesn’t reduce effectiveness-it often improves adherence because patients are more likely to fill affordable prescriptions.
What if my insurance won’t cover the separate generics?
If your insurance denies coverage for separate generics, ask for a prior authorization or exception form. Cite the JAMA study showing significant cost savings. You can also use patient assistance programs or pharmacy discount cards like GoodRx to pay cash-often cheaper than your insurance copay.
Do combo pills improve adherence more than separate generics?
Yes, for some people. Taking one pill instead of three can improve adherence by 15-25%. But this benefit only matters if the combo is the only affordable option. If you can afford the separate generics, you’re just as likely to take them. The key is affordability-if the generics are too expensive, the combo might help. But if the combo is priced unfairly, you’re paying more for the same benefit.
Bennett Ryynanen
January 1, 2026 AT 08:46Bro this is wild. I was on Janumet for a year and didn’t even know metformin was $4 at Walmart. My copay was $80. I switched to separate generics and now I’m saving $70 a month. I feel like I just robbed the pharmaceutical industry. Thanks for the wake-up call.
Chandreson Chandreas
January 2, 2026 AT 11:34Bro… 🤔 I’m from India, we get metformin for like 2 rupees a pill. Like, literally cheaper than a samosa. And here you guys paying $472 for the same thing? Madness. 🤯 Pharma is a casino and we’re all losing.
Darren Pearson
January 3, 2026 AT 16:27While the anecdotal evidence presented is compelling, one must consider the broader macroeconomic implications of pharmaceutical pricing structures. The cost of R&D, regulatory compliance, and distribution networks cannot be ignored, even when generics are available. The notion that combination therapies are inherently exploitative oversimplifies a highly complex industry ecosystem.
Stewart Smith
January 4, 2026 AT 06:54So let me get this straight… you’re telling me the same pills I’ve been paying $500 for are just sitting on a shelf somewhere, labeled ‘$15 each’? And my doctor didn’t know? 🤡
Retha Dungga
January 4, 2026 AT 19:26they just want you to stay sick so you keep buying pills lol its not about health its about profit 🤑 capitalism is a drug and we're all addicted
Aaron Bales
January 5, 2026 AT 16:42Always check GoodRx. Always. If your combo costs more than 2x the sum of the generics, ask for a switch. Simple. Effective. No drama.
Lawver Stanton
January 7, 2026 AT 00:41Okay so imagine this: you’re sitting in your doctor’s office, 72 years old, on five different pills, and your doc slides you a little white pill and says, ‘This one does it all.’ You’re like, ‘Oh thank god, I can finally stop juggling my pill organizer like a circus performer.’ Then you get the bill and it’s $600. You’re like… ‘Wait, what?’ And then you find out your blood pressure pill is $5 and your sugar pill is $3 and your cholesterol pill is $2? And they just glued them together and called it ‘Entresto’? And now you’re crying in the pharmacy aisle because you thought you were getting convenience but you were getting scammed? And your doctor didn’t even know? And the FDA is asleep? And your insurance? Oh, they’re just collecting the extra $500 and laughing all the way to the bank? And you’re just… a dumb human who trusted the system? And now you’re broke? And you’re still on the pill? Because you’re too tired to fight? And you just want to nap? And you’re not even mad anymore? You’re just… sad? And hungry? And you wish you’d never heard of combo pills? And now you’re Googling ‘how to make your own pills at home’? And you’re not even joking? Because this is America? And this is healthcare? And this is real life? And you’re not alone? And you’re not crazy? And you’re just… tired? And you just want to sleep? And you’re not asking for much? Just… a fair price? For a pill? That’s been around since the 80s? And you’re not asking for much? Just… not to be robbed? Every. Single. Month?
linda permata sari
January 7, 2026 AT 06:54In my country, we don’t even have combo pills like this. We get the generics, we take them, we live. Here, you need a PhD just to figure out if your medicine is a scam. It’s not healthcare, it’s performance art.
Hanna Spittel
January 8, 2026 AT 18:53Big Pharma owns Congress. The FDA is a shell game. They’re selling you placebo pills with extra profit margins. You think this is about health? Nah. It’s about control. They want you dependent. They want you scared. They want you paying $500 for a $15 pill. Wake up. 🕵️♀️💊
Joy Nickles
January 10, 2026 AT 05:22Okay so i went to goodrx and looked up janumet and it was $470 and then i looked up sitagliptin and metformin and metformin was 4$ and sitagliptin was 45$ so like 49$ total?? and i was like… wait… what… did they just… glue two pills together and charge me 10x?? and i called my pharmacy and they said ‘oh yeah we can do that’ and i switched and now i’m saving $420 a month and i feel like i just hacked the system?? but also… why does this even exist??
Emma Hooper
January 10, 2026 AT 14:02Y’all are losing your minds over $4 pills? 😂 I love it. I’ve been doing this for years-buying my metformin, lisinopril, and atorvastatin separately. I save over $500/month. My pharmacist thinks I’m a genius. My doctor thinks I’m weird. My bank account? Pure bliss. You’re not ‘cheap,’ you’re just smarter than the system. Keep it up.
Marilyn Ferrera
January 10, 2026 AT 14:27Always verify. Always compare. Always ask. Your health is worth the five minutes it takes to check GoodRx. You’re not being difficult-you’re being responsible.
Harriet Hollingsworth
January 10, 2026 AT 21:49People are dying because they can’t afford their meds. And here you are, saving $400 a month by being ‘smart.’ What’s the point of being smart if the system is still broken? This isn’t a win. It’s a tragedy dressed up as a hack.