Cannabinoids and Pain: What the Evidence Really Says About Dosing and Safety
 Jan, 13 2026
Jan, 13 2026
When you’re living with chronic pain, every new study, Instagram ad, or friend’s recommendation about cannabinoids feels like a lifeline. You’ve tried opioids, NSAIDs, physical therapy-maybe even nerve blocks. Now you’re hearing CBD can silence the pain without the high, or that THC might be the real answer. But here’s the truth: cannabinoids for pain isn’t a simple yes-or-no story. It’s a messy, contradictory, rapidly changing landscape where science, marketing, and desperation collide.
What Exactly Are Cannabinoids, and How Do They Work?
Cannabinoids are chemical compounds found in the cannabis plant. The two most talked-about are THC (tetrahydrocannabinol) and CBD (cannabidiol). But there are others-CBG, CBN, CBC-that are starting to show up in labs and clinics. These compounds interact with your body’s endocannabinoid system, a network of receptors that helps regulate pain, mood, sleep, and inflammation. Unlike opioids that block pain signals in the brain, cannabinoids work more like a dimmer switch. They don’t turn off pain completely; they tweak how your nervous system processes it. This is why they’re being studied for neuropathic pain-nerve damage from diabetes, shingles, or multiple sclerosis-where traditional drugs often fail. The problem? Not all cannabinoids are created equal. THC binds strongly to CB1 receptors in the brain, which is why it causes euphoria and dizziness. CBD doesn’t bind the same way. It’s non-intoxicating, but that doesn’t mean it’s a magic bullet. A 2023 University of Bath review of 16 high-quality trials found CBD performed no better than placebo for pain relief. Meanwhile, a Yale study from January 2025 showed CBG (cannabigerol) significantly reduced a key pain-signaling protein in lab tests-suggesting it might be more effective than CBD, without the high.The Evidence: Strong for Some, Weak for Others
The science on cannabinoids and pain is split down the middle. Some studies say yes. Others say no. And the difference often comes down to what compound you’re using. For THC-containing products, the evidence is stronger. Health Canada approved Sativex, a 1:1 THC:CBD spray, specifically for nerve pain in multiple sclerosis and cancer pain that doesn’t respond to opioids. Real patients report real results: one Leafly testimonial described cutting daily oxycodone from 120mg to 30mg after switching to a THC:CBD tincture-with better pain control and fewer side effects. But pure CBD? The data is thin. Harvard Medical School, the CDC, and the JAMA Network all agree: there’s no high-quality human trial proving CBD alone relieves pain. The FDA has only approved CBD for two rare forms of epilepsy-not pain. A 2023 systematic review found three studies showed no benefit from CBD for chronic pain, and one had mixed results. Even more troubling: consumer CBD products are unreliable. The University of Bath tested 50 popular brands and found some had zero CBD. Others had up to 260% more than labeled. Some contained illegal levels of THC. You could be spending $100 a month on a product that’s either useless-or accidentally getting you high and failing a drug test.Dosing: No Rules, Just Guesswork
There’s no official dosing guideline for cannabinoids and pain. Why? Because the FDA hasn’t approved any for this use. That means doctors are flying blind. Most pain clinics recommend starting low. For THC, that’s 2.5-5mg. For CBD, 10-20mg. Take it once or twice a day. Wait at least two weeks before increasing. Track your pain on a scale of 1-10. Keep a journal. If you don’t feel a difference after 4-6 weeks, it’s probably not working. The Yale study didn’t specify ideal doses for CBG, but it did show effects at low concentrations in lab models. That’s promising-but still far from human data. Until large clinical trials finish (some expected in 2025), dosing is trial and error. And here’s the catch: your body’s response depends on your weight, metabolism, liver function, and what other medications you’re taking. Cannabinoids are processed by the same liver enzymes as blood thinners, antidepressants, and seizure meds. Mixing them can lead to dangerous interactions. If you’re on warfarin, SSRIs, or statins, talk to your doctor before trying anything.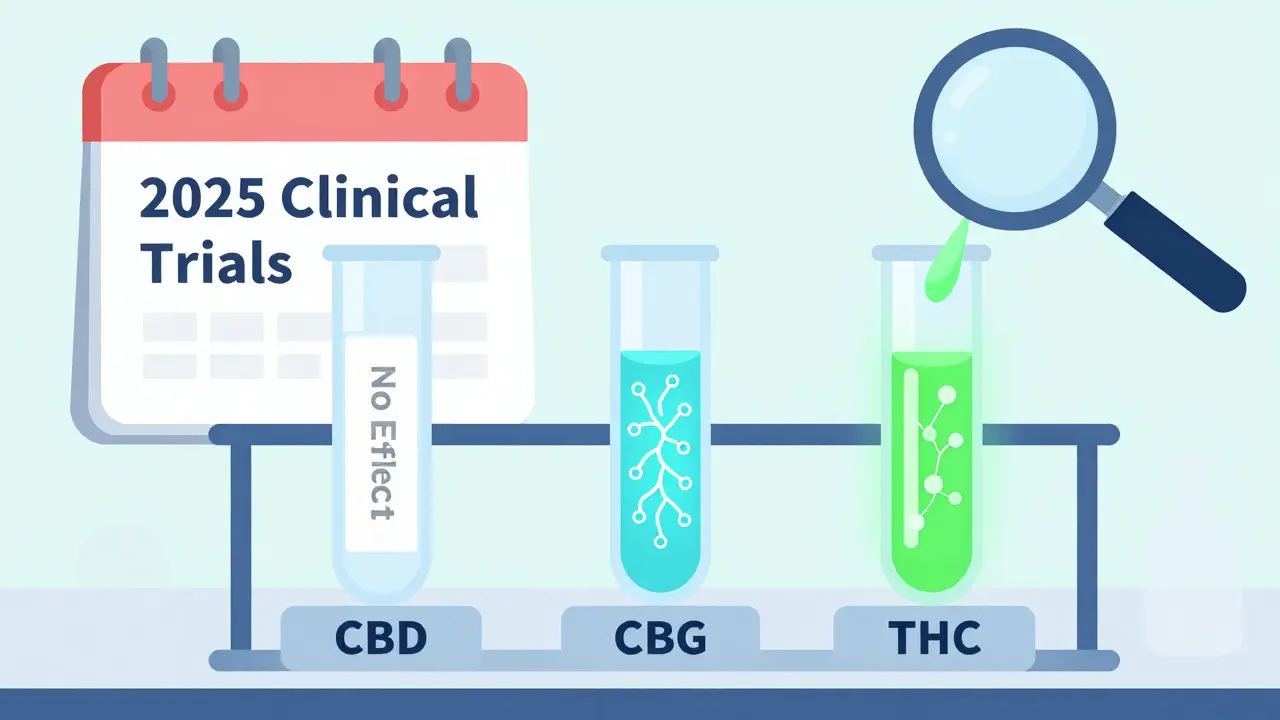
Safety: It’s Not Just About the High
Many people assume cannabinoids are safe because they’re “natural.” That’s dangerous thinking. Short-term side effects are common: dizziness (9% of users), dry mouth (7%), nausea (5%), and fatigue. These aren’t deal-breakers-but they’re not negligible either. Long-term risks are less clear. A 2023 meta-analysis flagged potential liver toxicity at high CBD doses. The CDC warns that chronic use may affect memory and motivation, especially in teens and young adults. And if your product contains unregulated THC, you risk anxiety, paranoia, or even psychosis in susceptible individuals. The biggest safety issue? Contamination. A 2023 analysis of 147 CBD products found traces of heavy metals, pesticides, or synthetic cannabinoids. These aren’t listed on labels. You have no idea what you’re ingesting. If you’re considering cannabinoids for pain, avoid online marketplaces like Amazon or Instagram sellers. Stick to licensed medical cannabis programs in states or countries with strict testing-like Canada, the Netherlands, or U.S. states with regulated dispensaries. Look for third-party lab reports (COAs) that verify potency and purity.Who Might Benefit? Who Should Avoid It?
Cannabinoids aren’t for everyone. But for some, they’re a game-changer. Good candidates:- People with neuropathic pain (diabetic nerve pain, post-shingles pain, MS-related pain)
- Those who can’t tolerate opioids due to side effects or addiction risk
- Patients already using opioids who want to reduce their dose (with medical supervision)
- Individuals seeking non-addictive alternatives for chronic, non-cancer pain
- Those with a personal or family history of psychosis or schizophrenia
- Pregnant or breastfeeding women (data is too limited)
- People on medications metabolized by the liver (especially blood thinners, antidepressants, statins)
- Anyone expecting CBD alone to cure severe arthritis or back pain without other treatment

The Future: What’s Coming Next?
The field is changing fast. In 2025, we’re seeing the first serious clinical trials for CBG-based pain treatments. If Yale’s lab results hold up in humans, we could see a new class of non-intoxicating pain meds by 2027. The FDA is also reviewing whether cannabis should be moved from Schedule I (no medical use) to Schedule III (like ketamine). That could unlock billions in research funding and lead to FDA-approved cannabinoid drugs for pain. Meanwhile, the market is booming. The U.S. medical cannabis industry hit $12.4 billion in 2022 and is projected to grow to $47 billion by 2027. But most of that growth is fueled by consumer demand for CBD-despite the lack of evidence. Companies are selling hope, not science. Until rigorous trials are done, the best advice is simple: don’t gamble with your pain. If you’re considering cannabinoids, do it under medical supervision. Use regulated products. Start low. Go slow. And keep your expectations realistic.Real People, Real Results
Reddit threads and patient forums show the divide. One user, u/PainWarrior22, wrote: “After two weeks of CBD oil, my fibromyalgia pain dropped 30%.” Another, u/TruthSeeker87, said: “Spent $400 on gummies. Zero effect on my back pain.” Trustpilot reviews for top CBD brands average just 3.2 out of 5. The most common complaint? “No pain relief.” The most common praise? “Helped me sleep.” That’s the pattern: cannabinoids may help with sleep or anxiety-which indirectly eases pain-but they rarely eliminate the pain itself. If you’re looking for a miracle, you’ll be disappointed. If you’re looking for a tool to add to your toolkit, it might be worth trying-carefully.Can CBD alone relieve chronic pain?
Current high-quality evidence says no. Multiple randomized controlled trials, including a 2023 University of Bath review of 16 studies, found CBD performed no better than placebo for chronic pain. The FDA has not approved CBD for pain treatment. While some people report benefits, these are likely due to placebo effect, improved sleep, or reduced anxiety-not direct pain relief.
Is THC better than CBD for pain?
Yes, for certain types of pain. THC has stronger evidence for neuropathic pain and cancer-related pain, especially when combined with CBD. Health Canada approved Sativex, a 1:1 THC:CBD spray, for these conditions. Pure THC can cause intoxication, but many patients find the pain relief worth the trade-off-especially when opioids aren’t working or are too risky.
What’s the safest way to take cannabinoids for pain?
Use regulated, lab-tested products from licensed medical cannabis dispensaries. Avoid online CBD gummies, oils, or vape pens sold on Amazon or Instagram. Start with low doses: 2.5-5mg THC or 10-20mg CBD. Take it orally (tincture or capsule) rather than smoking or vaping. Monitor your response for at least 4-6 weeks before deciding if it works.
Can cannabinoids replace opioids?
Not without medical supervision. Some patients have successfully reduced opioid doses using THC:CBD combinations, but stopping opioids abruptly can cause severe withdrawal. Always work with a pain specialist. Cannabinoids may help reduce opioid use, but they shouldn’t be used as a direct substitute without a structured plan.
Are there any new cannabinoids on the horizon for pain?
Yes. CBG (cannabigerol) is emerging as a promising non-intoxicating option. A January 2025 Yale study found CBG reduced a key pain-signaling protein more effectively than CBD or CBN in lab tests. Clinical trials are expected to begin in 2025. If proven safe and effective in humans, CBG could become the first non-psychoactive cannabinoid approved for pain.
Why do some people say cannabinoids work while others say they don’t?
It depends on the product, the condition, and the individual. People using regulated THC:CBD products for nerve pain often report success. Those buying unregulated CBD oil for arthritis or back pain usually don’t. Placebo effect, sleep improvement, and reduced anxiety can feel like pain relief. But for true, persistent pain, the science doesn’t support most over-the-counter CBD products.
If you’re considering cannabinoids for pain, don’t let marketing push you into spending hundreds on unproven products. Talk to your doctor. Get lab-tested options. Track your results. And remember: the goal isn’t to find a miracle. It’s to find a tool that helps-safely and sustainably.
Susie Deer
January 13, 2026 AT 22:33Allison Deming
January 15, 2026 AT 14:08Andrew Freeman
January 16, 2026 AT 17:04TooAfraid ToSay
January 17, 2026 AT 18:54Anna Hunger
January 18, 2026 AT 21:51says haze
January 19, 2026 AT 21:12Alvin Bregman
January 20, 2026 AT 06:43Henry Sy
January 21, 2026 AT 04:02Jason Yan
January 22, 2026 AT 12:20shiv singh
January 22, 2026 AT 15:25Robert Way
January 23, 2026 AT 14:41Sarah -Jane Vincent
January 25, 2026 AT 11:53Dylan Livingston
January 27, 2026 AT 11:36