Calcium Channel Blockers: How Metabolic Interactions Affect Drug Clearance and Safety
 Jan, 17 2026
Jan, 17 2026
Calcium Channel Blocker Interaction Risk Calculator
Calcium channel blockers (CCBs) are one of the most commonly prescribed heart medications in the U.S., with over 50 million people using them to treat high blood pressure, chest pain, and irregular heartbeats. But for many, the real danger isn’t the drug itself-it’s what happens when it mixes with other pills, foods, or even natural supplements. The problem? These drugs don’t just work in your bloodstream. They’re processed by your liver, and that’s where things can go wrong-fast.
How Calcium Channel Blockers Work and Why They’re So Widely Used
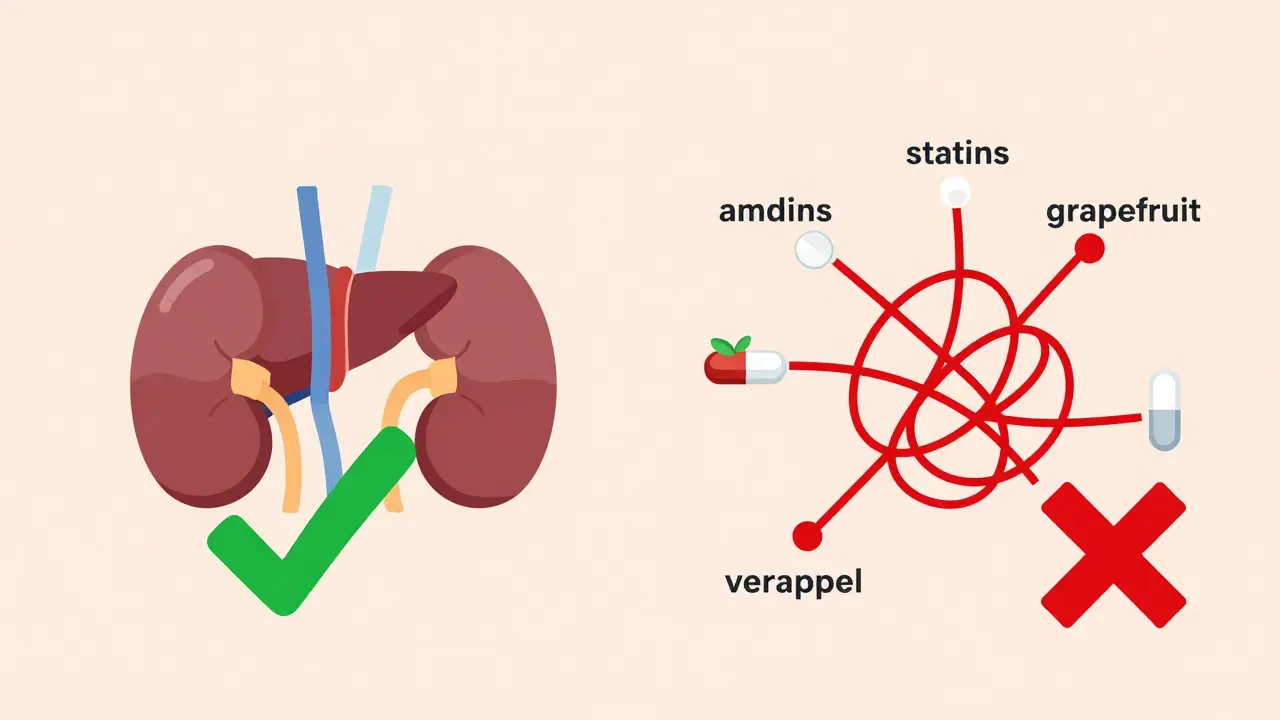
Calcium channel blockers stop calcium from entering heart and blood vessel cells. This relaxation of blood vessels lowers blood pressure and reduces the heart’s workload. There are two main types: dihydropyridines (DHPs) like amlodipine, nifedipine, and felodipine, and non-dihydropyridines (non-DHPs) like verapamil and diltiazem.
DHPs mainly affect blood vessels. That’s why they’re the go-to for high blood pressure-they don’t slow your heart rate much. Non-DHPs hit both the heart and vessels. They’re used for arrhythmias and angina, but they carry more risk because they directly affect how your heart beats.
Why are DHPs prescribed more? About 75% of CCB prescriptions are for amlodipine or similar drugs. They’re longer-lasting, need just one dose a day, and-critically-they cause fewer dangerous interactions than verapamil or diltiazem.
The Liver Is the Main Battleground: CYP3A4 and Drug Clearance
Almost all calcium channel blockers are broken down by the same liver enzyme: CYP3A4. This enzyme is responsible for metabolizing more than half of all prescription drugs. When CCBs enter your body, CYP3A4 chops them into smaller pieces so your kidneys can flush them out.
But here’s the catch: many other drugs, herbs, and even foods block or slow down CYP3A4. When that happens, your body can’t clear the CCB fast enough. The drug builds up in your blood. That’s when you get dangerously low blood pressure, a slow heart rate, or even heart block.
For example, amlodipine’s bioavailability is only 64% because CYP3A4 breaks down a big chunk of it right after you swallow it. If you take a strong CYP3A4 inhibitor like ketoconazole or clarithromycin, that clearance drops by 40%. For verapamil? It drops by 60-70%. That’s not a small change-it’s life-threatening.
Key Interactions That Can Land You in the ER
Some interactions are so dangerous they’re outright contraindicated. The European Society of Cardiology warns that combining verapamil with strong CYP3A4 inhibitors like ritonavir or itraconazole has led to 17 cases of complete heart block requiring pacemakers. That’s not rare. It’s documented.
Grapefruit juice is another silent killer. It blocks CYP3A4 in your gut, so more of the drug gets into your bloodstream before the liver can break it down. On Mayo Clinic’s patient forum, 68% of users who reported sudden drops in blood pressure were taking CCBs with grapefruit juice. Nearly 50 of them ended up in the ER.
Statin drugs like simvastatin and atorvastatin are another major risk. Diltiazem can increase simvastatin levels by 400%. That’s not a typo. It leads to muscle breakdown (rhabdomyolysis), kidney failure, and even death. One Reddit thread from r/Pharmacy documented 37 cases of statin-CCB myopathy-all preventable with better screening.
And then there’s sildenafil (Viagra). It’s a CYP3A4 substrate too. When taken with verapamil, 87% of users reported severe hypotension. With amlodipine? Only 23%. That’s why doctors now tell patients: if you’re on verapamil, don’t take ED meds unless under strict supervision.
Amlodipine vs. Verapamil: Why One Is Safer Than the Other
Not all CCBs are created equal when it comes to interactions.
Amlodipine is the safest bet for patients on multiple medications. It’s metabolized by CYP3A4, but it doesn’t inhibit the enzyme itself. It’s also highly protein-bound (97.5%), which means it stays stable in the blood. Its half-life is 30-50 hours, so it builds up slowly and predictably. Only 12% of patients on moderate CYP3A4 inhibitors need a dose change with amlodipine.
Verapamil? It’s a double agent. It’s broken down by CYP3A4-and it also blocks it. That means it doesn’t just sit there waiting to be cleared. It actively slows down how other drugs are processed. It also inhibits P-glycoprotein, a transporter that pushes drugs like digoxin out of cells. The result? Digoxin levels spike by 50-75%. That’s enough to cause fatal arrhythmias.
Diltiazem is in the middle. It’s a moderate CYP3A4 inhibitor. It’s safer than verapamil but still risky with statins, antifungals, or certain antidepressants. About 45% of patients on diltiazem need dose adjustments when adding other meds. That’s nearly four times higher than amlodipine.
Who’s at Highest Risk? Age, Kidneys, and Polypharmacy
It’s not just about what you take-it’s who you are.
Patients over 65 are 3.2 times more likely to have severe CCB interactions. Why? Their livers don’t process drugs as fast. Their kidneys are slower at clearing metabolites. And they’re more likely to be on five or more medications.
One study of 1,200 patients found that those with kidney impairment (eGFR below 60 mL/min) had a 47% higher risk of toxicity. That’s why FDA guidelines say: if your kidneys are weak, cut your verapamil dose in half. But amlodipine? No adjustment needed. That’s why it’s now the first-line choice for older adults with multiple conditions.
And then there’s polypharmacy. Over 58% of Medicare patients take five or more drugs that can interact with CCBs. That’s not just a coincidence-it’s a crisis. The cost of managing these interactions is projected to jump from $1.2 billion to $2.7 billion a year by 2027.

What Doctors and Pharmacies Are Doing to Stop the Harm
Hospitals and clinics aren’t ignoring this. The Cleveland Clinic now requires CYP3A4 interaction screening for every new CCB prescription. They found 23% of patients were at high risk.
Community pharmacists are spending over 12 minutes per CCB script checking for interactions. In 18% of cases, they catch something dangerous and call the doctor before the patient even leaves the pharmacy.
Electronic health records now have mandatory alerts. Epic Systems rolled out CYP3A4 interaction warnings in 2022. The result? A 42% drop in serious events.
There’s even a new FDA-approved tool called CCB-Check. It integrates with EHRs and gives a real-time risk score. In its first six months, it cut hospitalizations from CCB interactions by 31%.
What You Should Do Right Now
If you’re on a calcium channel blocker, here’s what you need to do:
- Check every medication-even over-the-counter ones. Antifungals, antibiotics like clarithromycin, and even some antidepressants can interact.
- Avoid grapefruit and Seville oranges. No exceptions. Even one glass a day can spike your drug levels.
- Ask your pharmacist if your CCB is amlodipine or something else. If it’s verapamil or diltiazem, ask if any of your other drugs are CYP3A4 inhibitors.
- Know your kidney function. If you’ve had a recent blood test showing low eGFR, tell your doctor. You may need a dose change.
- Monitor for symptoms: dizziness, fainting, slow pulse, swelling in your legs, or unusual muscle pain. These aren’t normal side effects-they’re warning signs.
If you’re prescribed a new drug while on a CCB, don’t assume it’s safe. Always ask: "Does this affect CYP3A4?" If the answer is yes, your doctor needs to reconsider.
The Future: Personalized Dosing and Genetic Testing
Science is catching up. Researchers at the Pharmacogenomics Research Network are studying how your genes affect CYP3A4 activity. Early results show 27% of people have genetic variants that make them ultra-sensitive to CCBs. They need much lower doses.
Even your gut bacteria matter. New studies show gut microbiome differences explain 34% of why some people clear CCBs faster than others. That’s why a one-size-fits-all dose doesn’t work.
By 2027, personalized dosing based on liver function, kidney health, genetics, and gut health will be standard. Until then, the safest choice is clear: if you’re on multiple medications, choose amlodipine. It’s not just the most prescribed CCB-it’s the most predictable, the most forgiving, and the most patient-safe.
Can I drink grapefruit juice while taking a calcium channel blocker?
No. Grapefruit juice blocks the CYP3A4 enzyme in your gut, causing calcium channel blockers-especially verapamil, diltiazem, and nifedipine-to build up to dangerous levels. This can cause severe low blood pressure, dizziness, or fainting. Even one glass a day can trigger this. Amlodipine is less affected, but the risk isn’t zero. Avoid grapefruit entirely if you’re on any CCB.
Which calcium channel blocker has the fewest drug interactions?
Amlodipine has the fewest drug interactions among calcium channel blockers. It’s metabolized by CYP3A4 but doesn’t inhibit the enzyme itself. Only about 12% of patients on moderate CYP3A4 inhibitors need a dose adjustment with amlodipine. In contrast, diltiazem and verapamil actively interfere with drug metabolism and require frequent dose changes. For patients on multiple medications, amlodipine is the safest choice.
Can calcium channel blockers cause kidney damage?
Calcium channel blockers themselves don’t damage kidneys. In fact, they’re often used to protect kidney function in people with high blood pressure. But if your kidneys are already impaired (eGFR below 60), your body can’t clear the drug’s metabolites as quickly. This raises the risk of toxicity, especially with verapamil, which requires a 50% dose reduction in kidney disease. Amlodipine doesn’t need adjustment. Always check your kidney function before starting or changing a CCB.
Why is verapamil riskier than amlodipine?
Verapamil is both a substrate and an inhibitor of CYP3A4, meaning it slows down how your body processes other drugs. It also blocks P-glycoprotein, raising levels of digoxin and other medications. This dual action makes it far more likely to cause dangerous interactions. Amlodipine doesn’t inhibit enzymes or transporters-it just gets cleared. Verapamil’s short half-life also means levels can spike quickly if metabolism is blocked. That’s why it’s avoided in elderly patients and those on multiple drugs.
What should I do if I start a new medication while on a calcium channel blocker?
Always check with your pharmacist or doctor before starting any new drug, supplement, or herb. Even common items like St. John’s wort, turmeric, or certain antibiotics can interfere with CCB metabolism. If you’re on verapamil or diltiazem, assume any new drug could interact until proven otherwise. Ask specifically: "Does this affect CYP3A4?" If yes, your CCB may need to be changed or your dose adjusted.
Are there any blood tests to check if my calcium channel blocker level is too high?
Yes, but they’re not routine. Therapeutic drug monitoring for verapamil is recommended when combined with CYP3A4 inhibitors, with target levels between 50-150 ng/mL. For amlodipine, routine blood testing isn’t needed because it’s predictable and has a wide safety margin. Most community pharmacies don’t offer this testing, but hospitals and specialty clinics do. If you’re on verapamil with other interacting drugs and feel dizzy or have a slow pulse, ask your doctor about checking your blood level.
Calcium channel blockers save lives-but only if used carefully. The biggest threat isn’t the drug. It’s the silence around how they interact with everything else you take. Talk to your pharmacist. Know what you’re on. And if you’re on more than one medication, don’t guess-ask.
kenneth pillet
January 18, 2026 AT 18:23Been on amlodipine for 5 years. Never had an issue. Grapefruit? Never touched it. Just read the label and ask your pharmacist. Simple.
Naomi Keyes
January 19, 2026 AT 15:57It's fascinating how the CYP3A4 pathway is so central to drug metabolism-yet, most patients are never educated on this! The enzyme’s inhibition isn't merely a pharmacokinetic footnote; it's a clinical earthquake waiting to happen. And yet, pharmacies still hand out prescriptions without verifying concurrent medications. This isn't negligence-it's systemic failure. The FDA's CCB-Check tool is a start, but mandatory genetic screening for CYP3A4 variants should be standard before prescribing any CCB, especially in polypharmacy patients. We're treating symptoms, not root causes.
Jake Moore
January 21, 2026 AT 06:31Good breakdown. I work in cardiology and see this every week. Amlodipine is the default for a reason. If someone's on 6 meds and needs a CCB? Amlodipine. No debate. Verapamil? Only if they’re got a specific arrhythmia and no other options. And always, always check the grapefruit juice thing. People think it’s just a ‘warning’-it’s a red alert.
Joni O
January 21, 2026 AT 11:46I’m 71 and on amlodipine. My pharmacist sat me down and explained all this last month. I didn’t know grapefruit could be dangerous. Now I drink orange juice instead. Thanks for writing this-really helped me feel less scared.
Ryan Otto
January 21, 2026 AT 23:13Let’s be honest-this whole CYP3A4 narrative is a pharmaceutical industry distraction. The real issue? Big Pharma pushes amlodipine because it’s patent-expired and profitable, while they bury the truth: verapamil is more effective for angina, but they don’t make money off it anymore. They’d rather you take a ‘safer’ drug that’s cheaper to produce. Meanwhile, your doctor gets kickbacks from the rep. Don’t be fooled by ‘evidence-based’ guidelines-they’re written by men in suits with stock options.
Max Sinclair
January 22, 2026 AT 10:42Thanks for the clear, well-researched post. I’ve seen patients panic over grapefruit juice-sometimes they’ve been drinking it for years without knowing. A simple conversation with a pharmacist can prevent ER visits. I’ve started asking my patients: ‘What’s in your kitchen?’ Not just what’s in your medicine cabinet.
Chuck Dickson
January 24, 2026 AT 10:21If you're on a CCB and you're over 60, stop guessing. Go to your pharmacy. Ask them to run a med sync. They’ll catch interactions you didn’t even know existed. I used to think I was fine until my pharmacist flagged that my antidepressant and diltiazem were playing hide-and-seek with my liver. Changed my med. No more dizziness. Life’s better now. Don’t wait for a blackout to learn this stuff.
Praseetha Pn
January 25, 2026 AT 20:16They say amlodipine is safe-but what about the long-term effects? No one talks about how CCBs mess with your mitochondria over time. The liver doesn’t just ‘process’ drugs-it gets damaged slowly, quietly. And the ‘evidence’? All funded by pharma. My cousin died from rhabdomyolysis after being on simvastatin + diltiazem. They called it ‘unfortunate coincidence.’ Coincidence? No. It was a textbook case. And they still sell it like candy.
Stacey Marsengill
January 27, 2026 AT 06:38Oh honey. You think grapefruit is the worst? Try St. John’s wort. Or turmeric. Or that ‘natural heart support’ supplement your sister swears by. I watched my neighbor go into full cardiac arrest because she took ‘herbal blood pressure tea’ with verapamil. The ER nurse said, ‘Ma’am, you just took a bomb to your heart.’ She didn’t even know it was dangerous. People think ‘natural’ means safe. It’s the opposite. Nature is a minefield.
Andrew McLarren
January 27, 2026 AT 23:42It is imperative to underscore the clinical significance of CYP3A4-mediated pharmacokinetic interactions. The data presented herein are unequivocal and align with the 2023 ACC/AHA guidelines on antihypertensive management in the elderly. The preferential use of amlodipine in polypharmacy cohorts is not merely prudent-it is evidence-based standard of care. Furthermore, the integration of pharmacogenomic screening into primary care workflows represents the next logical evolution in precision medicine. Institutions failing to adopt such protocols are operating below acceptable standards of risk mitigation.
Andrew Short
January 29, 2026 AT 04:37Why are we still letting doctors prescribe these drugs without mandatory blood level monitoring? It’s 2025. We have the tech. We have the data. But we don’t have the will. This isn’t about safety-it’s about profit. If they had to test every patient’s blood before giving a CCB, the cost would skyrocket. So they gamble with your life instead. Wake up.
Emma #########
January 30, 2026 AT 14:49I just started amlodipine last month. I was terrified. I read all this and felt way less alone. Thank you for writing this. I showed it to my mom. She’s on diltiazem and didn’t realize grapefruit was a no-go. We’re both going to the pharmacy tomorrow to get it checked.
Tyler Myers
January 31, 2026 AT 03:22the whole cyp3a4 thing is bs. i read a blog once that said the fda hides the real risks because they're scared of lawsuits. grapefruit juice? they just want you to buy their special ‘safe’ meds. amlodipine is just a money maker. verapamil works better. they just don't want you to know.
Eric Gebeke
February 1, 2026 AT 06:55People don’t realize how many drugs are CYP3A4 substrates. It’s not just statins and grapefruit. It’s your allergy meds, your anxiety pills, your painkillers-even some cold medicines. I had a friend on verapamil who took a Z-pack and ended up in the ICU. He thought antibiotics were ‘safe.’ They’re not. Nothing’s safe unless you check. And if you’re over 60? You’re basically a walking interaction waiting to happen.
christian Espinola
February 2, 2026 AT 20:26Why are we still using CCBs at all? Why not just treat high blood pressure with diet, exercise, and weight loss? This whole system is broken. We medicate instead of heal. And now we’re medicating with drugs that interact with everything. The real solution? Stop prescribing. Start educating. But that wouldn’t make money for the clinic. So here we are. Another patient with low blood pressure and a pacemaker.