Bipolar Disorder: Managing Mood Stabilizers and Antipsychotics Effectively
 Jan, 4 2026
Jan, 4 2026
Managing bipolar disorder isn’t just about taking pills-it’s about finding the right balance between controlling wild mood swings and living with side effects that can feel just as overwhelming. For many, the journey starts with a diagnosis and ends up in a long, sometimes frustrating, trial-and-error process with medications. Two main classes of drugs-mood stabilizers and antipsychotics-form the backbone of treatment. But knowing which one to use, when, and how to handle the downsides makes all the difference.
Why Mood Stabilizers Are Still the Foundation
Lithium has been the gold standard since the 1970s, and for good reason. It doesn’t just calm mania-it lowers the risk of suicide by 80% compared to no treatment. That’s not a small number. It’s life-saving. But lithium isn’t simple. You need regular blood tests to keep levels between 0.6 and 1.0 mmol/L. Too low, and it doesn’t work. Too high, and you risk toxicity-slurred speech, shaking, even seizures. Many people start lithium and quit fast because of the side effects. Constant thirst? Check. Urinating every hour? Common. Weight gain of 10 to 15 pounds in the first year? Almost expected. Some say it feels like your body is slowly turning into a sponge. But for others, the trade-off is worth it. One person on Reddit shared: “After three meds failed, lithium finally stopped my weekly suicidal depression. I gained 15 pounds-but I’m alive.” Other mood stabilizers like valproate and carbamazepine work well too, especially if lithium doesn’t fit. But valproate comes with serious risks for women of childbearing age-it can cause severe birth defects. Lamotrigine is different. It’s the go-to for preventing depressive episodes and causes little to no weight gain. But it comes with its own scare: a 1 in 10 chance of a serious skin rash. That’s why doctors start low-25mg a week-and move slow.Antipsychotics: Faster Relief, Heavier Costs
If you’re in the middle of a manic episode, mood stabilizers can take weeks to kick in. Antipsychotics like quetiapine (Seroquel) and olanzapine often bring relief in days. That’s why they’re now first-line for acute mania. Quetiapine also got FDA approval for bipolar depression in 2006, making it one of the few drugs that tackle both highs and lows. But here’s the catch: side effects hit hard. Up to 70% of people on quetiapine feel drowsy. Nearly two-thirds report weight gain-on average, 22 pounds in the first year. Olanzapine is even worse for metabolism: it raises your risk of type 2 diabetes by 20-30%. One patient on PatientsLikeMe rated its effectiveness 3.7 out of 5, but tolerability just 2.8. That gap says everything. Risperidone and aripiprazole are alternatives. Risperidone works fast for mania-68% respond within three weeks. Aripiprazole has a lower chance of weight gain, and now comes as a monthly injection (Abilify Maintena), which helps people who forget daily pills. But even these aren’t magic. Akathisia-a restless, agitated feeling-hits 15-20% of users. It’s not laziness. It’s a physical need to move that can make sitting still unbearable.Combining Medications: More Power, More Problems
When one drug doesn’t cut it, doctors often add another. A mood stabilizer plus an antipsychotic can push response rates to 70% in tough cases. But side effects pile up. Weight gain becomes worse. Sedation doubles. Blood sugar and cholesterol climb faster. One study showed combination therapy increases side effect burden by 25-30%. This isn’t about stacking pills-it’s about strategy. If you’re stuck in depression and lithium isn’t helping, adding lamotrigine might be smarter than adding an antipsychotic. If you’re cycling rapidly between mania and depression, a long-acting injectable like aripiprazole can give stability without daily reminders.What About Antidepressants?
This is where things get tricky. Antidepressants like fluoxetine or sertraline can help with deep depression in bipolar disorder-but they also carry a 10-15% risk of flipping you into mania. Some doctors avoid them entirely. Others use them cautiously, only if you’re already on a mood stabilizer. The Harvard Bipolar Research Program warns that up to 25% of people switch into mania with antidepressants alone. But UCLA researchers argue that for severe, treatment-resistant depression, the benefits can outweigh the risks-when used carefully. The key? Never use an antidepressant alone. Always pair it with a mood stabilizer or antipsychotic. And if you notice sudden energy, less need for sleep, or racing thoughts after starting an antidepressant-call your doctor. That’s not improvement. That’s a warning sign.Monitoring: The Unspoken Rule
Medication management isn’t a one-time script. It’s ongoing. For lithium, you need blood tests weekly at first, then every 2-3 months once stable. Elderly patients need lower doses-0.4 to 0.8 mmol/L-because their kidneys don’t clear it as well. For antipsychotics, you need quarterly checks on weight, waist size, blood sugar, and cholesterol. If your waist is over 40 inches (men) or 35 inches (women), you’re at higher risk for metabolic syndrome. That’s not just about looks-it’s about heart disease, stroke, and diabetes. Drug interactions are another silent danger. Taking lithium with ibuprofen or naproxen can spike your lithium levels by 25-60%. That’s dangerous. Antipsychotics interact with over 40 common medications, from antibiotics to heart drugs. Always tell every doctor you see what you’re taking-even your dentist.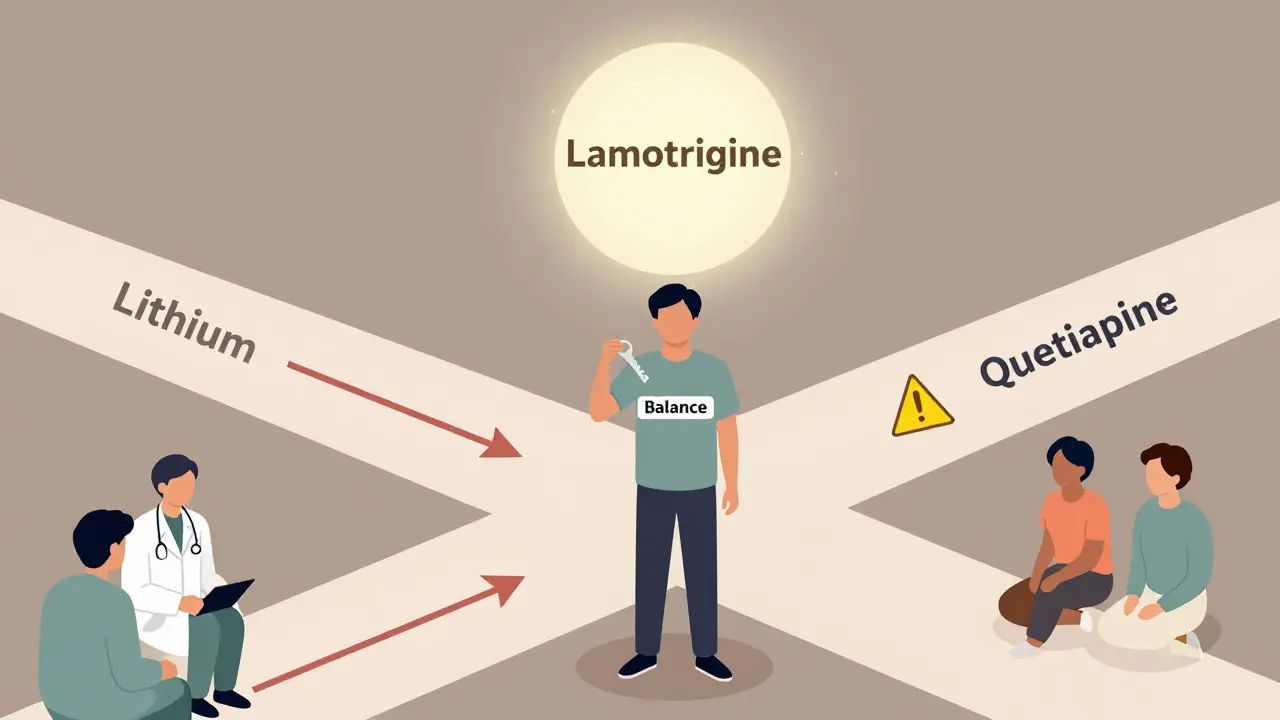
Real Stories, Real Trade-Offs
People don’t quit meds because they’re lazy. They quit because they feel worse on the medicine than they did before. - One user switched from lithium to lamotrigine to escape constant thirst-only to get severe insomnia. - Another lost 30 pounds after starting metformin to fight quetiapine-induced weight gain. - A third stopped all meds for a year, then went back to lithium because “the black holes of depression were worse than the tremors.” The common thread? Success isn’t about finding the perfect drug. It’s about finding the right balance for you. That takes time. It takes honesty. And it takes a team-psychiatrist, primary care doctor, and you.What’s New in 2026?
The field is evolving. In 2023, the FDA approved lumateperone (Caplyta) for bipolar depression-and it causes almost no weight gain. That’s huge. Cariprazine and lurasidone are now first-line choices for depression because they’re gentler on metabolism. Genetic testing (like Genomind’s test) helps predict which drugs your body will handle better, improving success rates by 30%. Long-acting injectables are becoming more common. Monthly shots mean fewer missed doses and more stable moods. Digital tools like reSET-BD, a smartphone app that tracks mood and medication adherence, are showing a 22% drop in relapses. But here’s the hard truth: only 35% of people with bipolar disorder reach full remission. Sixty percent still deal with side effects that interfere with daily life. The goal isn’t perfection. It’s function. Can you work? Can you sleep? Can you be present with your family? If the answer is yes-even with some side effects-you’re doing better than most.What to Do Next
If you’re on medication:- Track your mood, sleep, and side effects in a journal or app.
- Never stop or change doses without talking to your doctor.
- Ask about blood tests and metabolic checks every three months.
- If side effects are unbearable, say so. There’s always another option.
- Expect a few tries before finding the right mix.
- Ask your doctor: “What’s the goal here-stopping mania? Preventing depression? Reducing hospital visits?”
- Know your numbers: lithium levels, weight, waist size, fasting glucose.
Can you take mood stabilizers and antipsychotics together?
Yes, many people take both, especially if one drug alone isn’t enough. Combining lithium or lamotrigine with quetiapine or aripiprazole can improve mood control in treatment-resistant cases. But this also increases side effects like weight gain, drowsiness, and metabolic issues. Doctors usually start with one, then add the second only if needed.
Which is better for depression: lithium or quetiapine?
For bipolar depression, lamotrigine and quetiapine are both first-line. Quetiapine works faster-some feel better in a week. Lithium is slower but offers better long-term protection against both mania and suicide. Lamotrigine has the best side effect profile for depression-minimal weight gain-but carries a small risk of serious rash. The best choice depends on your history, side effect tolerance, and whether you’ve had more mania or depression episodes.
Why do some people gain so much weight on antipsychotics?
Antipsychotics like olanzapine and quetiapine affect hormones that control hunger and metabolism. They increase appetite, slow down metabolism, and make the body store fat more easily. Olanzapine causes about 4.6kg of weight gain in just six weeks. Quetiapine users average 22 pounds over a year. Metformin is often prescribed alongside to help manage this. Lifestyle changes-regular exercise, low-sugar diet-are also critical.
Is lithium dangerous long-term?
Lithium is safe for long-term use if monitored. The main risks are kidney and thyroid problems, which develop slowly over years. Blood tests every 3-6 months catch these early. Most people on lithium don’t develop serious issues if levels are kept in range. The benefit-reducing suicide risk by 80%-far outweighs the risks for most. Never stop lithium suddenly; it can trigger a severe relapse.
Can you drink alcohol while on these medications?
It’s not recommended. Alcohol can worsen drowsiness from antipsychotics and increase the risk of lithium toxicity by affecting kidney function. It also destabilizes mood, making episodes more likely. Even one drink can throw off your balance. Most psychiatrists advise complete avoidance, especially during the first few months of treatment.
What should you do if you miss a dose?
If you miss a lithium dose, take it as soon as you remember-if it’s within a few hours. If it’s close to your next dose, skip it. Never double up. For antipsychotics like quetiapine, missing one dose usually won’t cause withdrawal, but it can trigger mood instability. If you miss multiple doses, contact your doctor. Long-acting injections are an option if forgetting pills is a problem.
Are there natural alternatives to these drugs?
No natural supplement has been proven to replace mood stabilizers or antipsychotics for bipolar disorder. Omega-3s, magnesium, or vitamin D may help with general mood, but they won’t stop mania or severe depression. Relying on them instead of medication can lead to dangerous episodes. They can be used as supports, not substitutes. Always talk to your doctor before adding anything.
How long do you need to stay on these medications?
Most people need to stay on medication long-term-even if they feel fine. Bipolar disorder is a chronic condition. Stopping meds increases relapse risk by 70% within a year. Some people stay on low doses for life. Others, after years of stability, may try tapering under strict supervision. But this is rare and requires careful planning. Never stop on your own.
Doreen Pachificus
January 6, 2026 AT 01:43Been on lamotrigine for 2 years. Zero weight gain, no tremors, just quiet stability. I still get low days, but they don’t swallow me whole anymore. Worth the slow ramp-up.
Rory Corrigan
January 6, 2026 AT 11:54lithium made me feel like a robot with a thirst for the ocean 🌊 but it saved my life. i’d take the sponge-body over the black hole any day. #worthit
Ethan Purser
January 6, 2026 AT 16:37Look, we’re all just trying not to kill ourselves while gaining 30 pounds and forgetting how to spell our own names. This isn’t treatment-it’s a high-stakes game of Russian roulette with a pharmacy. One day you’re stable, the next you’re sobbing in the cereal aisle because your brain forgot how to feel joy. And don’t get me started on the doctors who act like you’re a broken toaster. ‘Try this new combo!’ Like I’m some lab rat with a Netflix subscription. I’m not a statistic. I’m a person who just wants to sleep through the night without wondering if tomorrow’s gonna be the day I vanish.
And yeah, I know-‘just take your meds.’ Like I don’t hear that every damn day. I’ve got a pill organizer with more compartments than my therapist has degrees. But when your body turns against you and your meds turn against you too, what’s left? Just you, the clock, and the silence that screams louder than mania ever did.
I’ve tried everything. Even the damn injection. I still wake up wondering if today’s the day the world stops spinning. But I’m still here. And that’s not nothing. That’s everything.
They say bipolar is a disease of extremes. Nah. It’s a disease of exhaustion. Of being tired of being tired. Of loving people so hard you’re afraid you’ll break them. Of smiling through panic attacks because you don’t want to be ‘too much.’
So yeah. I’m tired. But I’m still here. And I’m not done fighting.
Stephen Craig
January 7, 2026 AT 11:56Combining lamotrigine and aripiprazole gave me the best balance. Minimal weight gain, no sedation, and no manic spikes. Took 18 months to find it. Worth it.
Connor Hale
January 8, 2026 AT 15:21The real issue isn’t the meds-it’s the system. We’re expected to self-manage chronic illness with 15-minute appointments, no insurance support, and zero access to therapy. Lithium works. But if you can’t afford blood tests every 3 months, you’re just waiting for a crisis. This isn’t healthcare. It’s a lottery.
And yes, side effects suck. But so does losing your family, your job, your sense of self. I’d rather be tired and alive than energetic and gone.
Roshan Aryal
January 10, 2026 AT 07:27USA still thinks psychiatry is about popping pills like candy. In India, we treat mental illness with family, discipline, and silence. No one here takes lithium. We just pray harder. And guess what? Our suicide rates are lower. Maybe the problem isn’t the brain-it’s the culture that makes you feel broken for needing help.
You think you’re special because you track your mood in an app? We track our emotions by how many times we eat in a day. No apps. No doctors. Just survival. You call it ‘treatment.’ We call it living.
Jack Wernet
January 10, 2026 AT 21:29I appreciate the thoroughness of this post. As a clinician, I’ve seen patients abandon treatment due to side effects, only to return months later in crisis. The key is not perfection-it’s persistence. Regular monitoring, open dialogue with your provider, and patience are non-negotiable. Medication is a tool, not a cure. But it’s one of the few tools we have that actually saves lives.
Charlotte N
January 11, 2026 AT 15:26i’ve been on quetiapine for 4 years… weight gain? yes. insomnia? yes. but i haven’t been hospitalized since i started… so… i guess… it works? i don’t know anymore… sometimes i wonder if i’m just… surviving… not living… but then i look at my dog and he’s still here and i’m still here and… that’s something? right?…