Audiometry Testing Explained: How Hearing Assessment and Decibel Levels Work
 Nov, 20 2025
Nov, 20 2025
What Is Audiometry Testing?
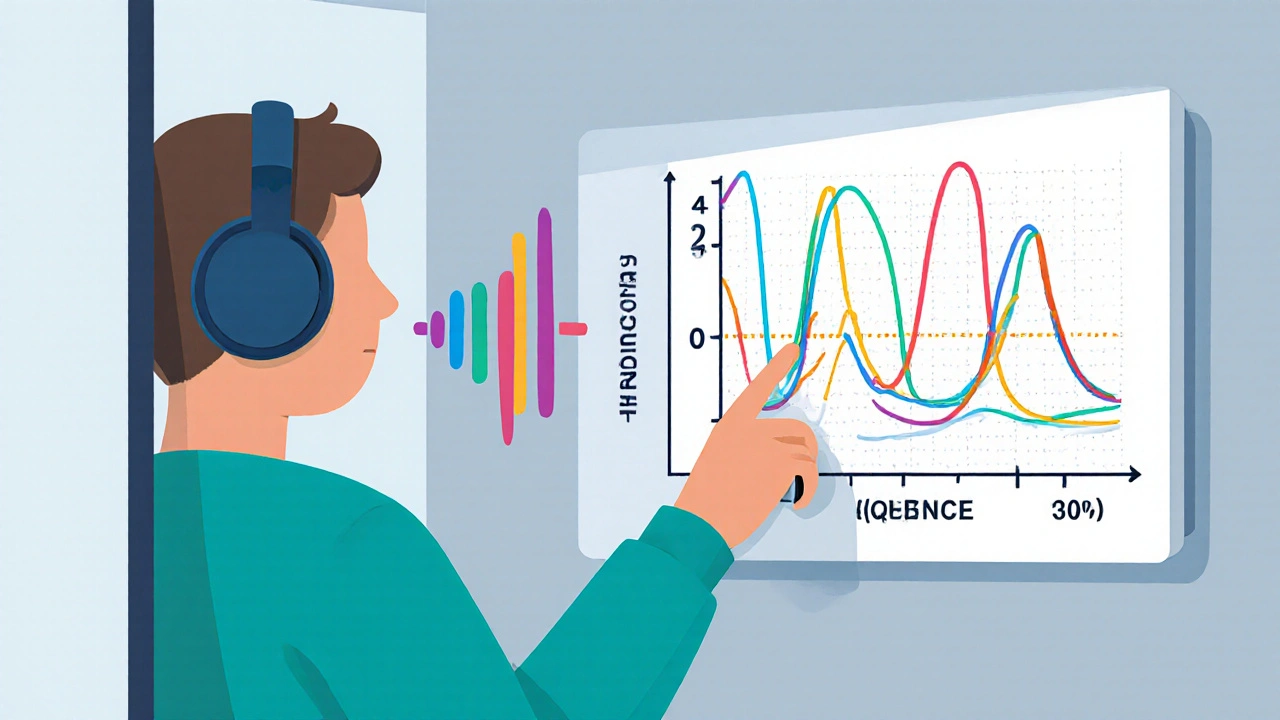
Audiometry testing is the standard way doctors measure how well you hear sounds at different pitches and volumes. It’s not a guess or a quick check-it’s a precise, science-backed process that maps your hearing ability using decibel levels and specific frequencies. The results are shown on a graph called an audiogram, which tells your audiologist exactly where your hearing is strong and where it’s weak.
This test doesn’t just say “you have hearing loss.” It tells you how much loss you have, which frequencies are affected, and what kind of hearing loss it is-whether it’s from earwax, middle ear fluid, nerve damage, or something else. That’s why it’s the gold standard for diagnosing hearing problems.
How Decibel Levels Work in Hearing Tests
Decibels (dB) measure sound intensity. In audiometry, the scale starts at 0 dB HL (hearing level), which isn’t silence-it’s the softest sound a young, healthy ear can detect. Normal hearing means you can hear sounds at 25 dB HL or lower across all tested frequencies.
Here’s what different decibel ranges mean:
- 0-25 dB HL: Normal hearing
- 26-40 dB HL: Mild hearing loss-you miss soft speech, especially in noisy places
- 41-55 dB HL: Moderate hearing loss-you struggle with regular conversation
- 56-70 dB HL: Moderately severe hearing loss-you need people to speak loudly or clearly
- 71-90 dB HL: Severe hearing loss-you hear only loud sounds or shouting
- 91+ dB HL: Profound hearing loss-you may rely on lip reading or sign language
Most people don’t realize that hearing loss often starts in the high frequencies-like birds chirping, children’s voices, or consonants like “s,” “f,” and “th.” That’s why you might say, “I can hear people talk, but I can’t understand them.” Audiometry catches that early.
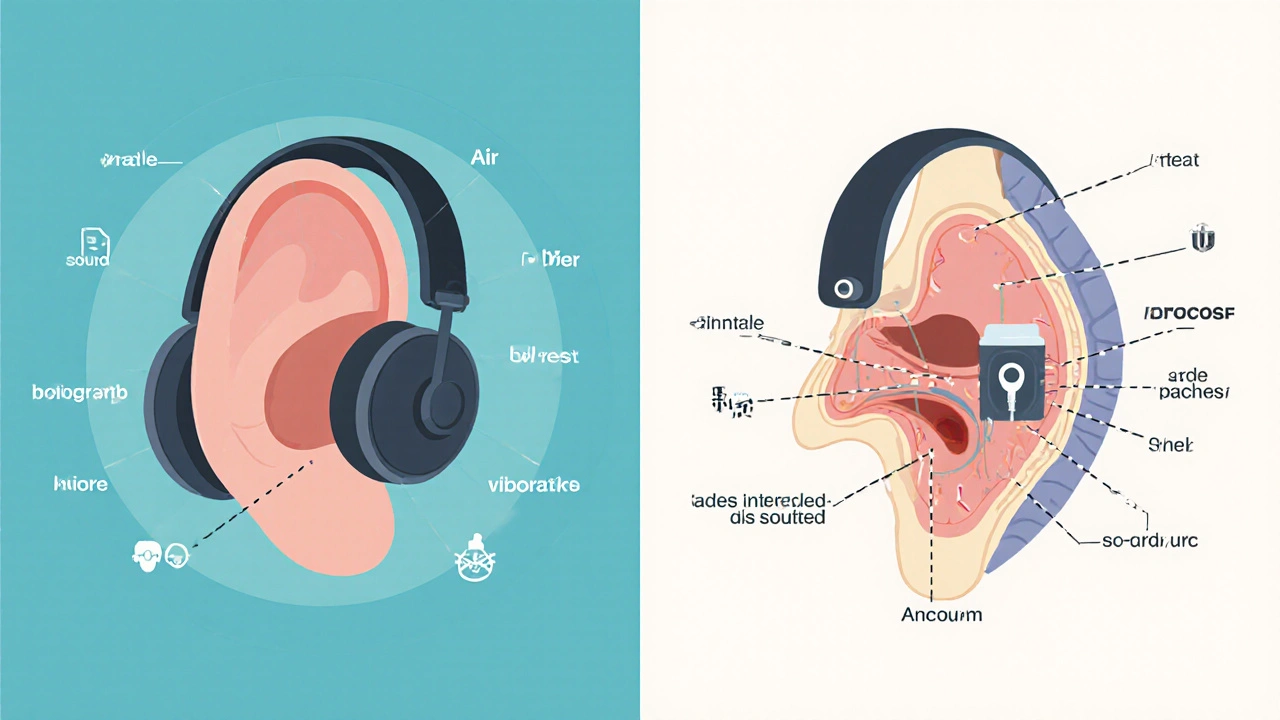
How the Test Is Done: Air and Bone Conduction
You sit in a quiet room, wear headphones, and press a button every time you hear a tone. That’s air conduction testing-it sends sound through your ear canal, eardrum, and middle ear bones to your inner ear.
Then, the audiologist places a small device behind your ear on the mastoid bone. This is bone conduction testing. It bypasses your outer and middle ear entirely, sending vibrations straight to your inner ear. If your air conduction thresholds are worse than your bone conduction ones by 15 dB or more, that means something’s blocking sound in your outer or middle ear-like earwax, fluid, or a perforated eardrum. That’s called conductive hearing loss.
If both air and bone conduction are equally poor, the problem is in your inner ear or auditory nerve. That’s sensorineural hearing loss, the most common type, often caused by aging or noise exposure.
The Hughson-Westlake Method: How Thresholds Are Found
It’s not just about hearing a loud tone. The goal is to find the softest sound you can hear half the time. That’s called your threshold.
The method used is called the modified Hughson-Westlake technique. Here’s how it works:
- The audiologist starts with a tone you can easily hear-say, 40 dB at 1000 Hz.
- They lower the volume by 10 dB. If you don’t hear it, they raise it by 5 dB.
- They keep going up and down in 5 dB steps until they find the quietest sound you hear 50% of the time.
This takes time-about 10 to 15 minutes per ear. But it’s accurate. Screening tests skip this and just check if you hear a loud tone. They’re good for schools or workplaces, but they miss subtle losses. Diagnostic audiometry doesn’t cut corners.
Speech Testing: Can You Understand Words?
Hearing a tone isn’t the same as understanding speech. That’s why speech testing is part of the full evaluation.
First, they test your speech reception threshold (SRT)-the quietest level at which you can repeat 50% of two-syllable words like “baseball” or “hotdog.” Your SRT should match your average pure-tone hearing level at 500, 1000, and 2000 Hz. If it doesn’t, something’s off.
Then comes word recognition or speech discrimination testing. You’ll hear a list of single-syllable words at a volume 25-40 dB above your threshold. Normal listeners get 90% or more correct. If you score below 70%, it suggests nerve damage or problems with how your brain processes sound-even if your ears are working fine.
This is why two people with the same audiogram can have totally different experiences. One hears everything clearly. The other hears sounds but can’t make sense of them. Speech testing explains why.
Tympanometry and ABR: The Supporting Tests
Audiometry doesn’t stop at tones and words. Tympanometry checks your eardrum’s movement. A small probe goes in your ear and changes air pressure while measuring how your eardrum responds. A flat line (Type B) means fluid is behind the eardrum-common in kids with ear infections. A normal curve (Type A) means your middle ear is healthy.
For babies, toddlers, or people who can’t respond reliably, they use auditory brainstem response (ABR). Electrodes on your head record how your brainstem reacts to clicking sounds. No response needed from you. It’s used for newborn screenings and for patients who can’t sit still or follow instructions.
These tests don’t replace audiometry-they complete it. Together, they give a full picture: is it your ear canal? Your eardrum? Your inner ear? Your nerve? Your brain?
Who Needs Audiometry Testing?
You don’t have to be old to need this test. Here are common reasons:
- You’re over 50 and notice trouble with conversations
- You work in a noisy environment (construction, factory, music)
- You have ringing in your ears (tinnitus)
- You feel like people are mumbling
- You’ve had ear infections, head injuries, or take medications that can harm hearing (like some antibiotics or chemotherapy drugs)
- Your child didn’t pass a newborn hearing screen
- You’re considering hearing aids
The CDC recommends all newborns be screened before leaving the hospital. If they fail, a full diagnostic audiometry test should happen by 3 months old. Early intervention changes everything.
What to Expect During the Test
It’s not scary. You’ll sit in a soundproof booth. You’ll wear headphones or earplugs. You’ll hear beeps, tones, and sometimes words. You’ll press a button or raise your hand. That’s it.
Some people find bone conduction uncomfortable-especially if you wear glasses. The oscillator on your skull can feel odd. But it’s brief. Most tests last 30-45 minutes. You can take breaks.
Don’t worry if you miss some tones. The test is designed so you won’t hear everything. The audiologist knows how to interpret partial responses. Just answer honestly. Don’t guess.
What Happens After the Test?
Your audiologist will show you your audiogram. They’ll explain what each line means. They’ll tell you if you have hearing loss, what kind, and how severe.
If you have mild to moderate loss, they might recommend hearing aids. If it’s conductive, they might refer you to an ENT for treatment-like removing wax or fixing a perforated eardrum. If it’s sensorineural, they’ll discuss hearing devices or assistive tech.
They’ll also give you a written report. Keep it. You’ll need it for insurance, hearing aid fitting, or future comparisons.
Why This Test Matters More Than You Think
Hearing loss doesn’t just affect your ears. It affects your brain, your relationships, your safety, and your mental health. People with untreated hearing loss are more likely to develop depression, anxiety, and even dementia.
That’s why accurate audiometry is so important. It’s not just about turning up the volume. It’s about catching problems early, understanding the cause, and getting the right solution. A hearing aid won’t help if your problem is fluid in your ear. Surgery won’t help if your nerve is damaged.
With the population aging and noise exposure rising, audiometry is becoming more critical than ever. In the U.S., 48 million people have hearing loss. Many don’t know it-until they get tested.
Common Myths About Audiometry
- Myth: “I don’t need a test because I can still hear loud sounds.”
Truth: High-frequency loss is common and sneaky. You hear shouting but miss whispers and consonants. - Myth: “Retail hearing tests are good enough.”
Truth: Screening kiosks only check if you hear a loud tone. They miss type, severity, and cause. They’re not diagnostic. - Myth: “My hearing got worse overnight.”
Truth: Hearing loss is usually gradual. You adapt slowly. What feels sudden is often years of slow decline. - Myth: “Audiometry is painful or invasive.”
Truth: It’s completely non-invasive. No needles, no radiation, no discomfort beyond mild pressure from bone conduction.
How long does an audiometry test take?
A full diagnostic audiometry test usually takes 30 to 45 minutes. This includes air and bone conduction testing, speech recognition, and tympanometry. Screening tests can be done in 5 to 10 minutes, but they’re not diagnostic.
Can I do audiometry at home?
Some tele-audiology platforms offer remote screening using validated apps and headphones, but they’re not as accurate as in-clinic tests. For a full diagnosis-especially if you’re considering hearing aids-you need a professional test in a soundproof booth with calibrated equipment.
What if my audiogram shows hearing loss but I feel fine?
That’s common. Hearing loss often develops slowly, and your brain adapts. You might not notice until you’re in a noisy restaurant or trying to follow a group conversation. An audiogram shows the reality-even if you’ve learned to compensate. Early intervention prevents further strain on your brain and communication skills.
Are there different types of audiometry tests?
Yes. Pure-tone audiometry is the most common. Speech audiometry measures word understanding. Tympanometry checks middle ear function. ABR tests the brain’s response to sound, used for babies or non-responsive patients. Otoacoustic emissions (OAE) test inner ear function and are often used in newborn screening.
How often should I get my hearing tested?
If you’re over 50, get tested every 2 to 3 years. If you’re exposed to loud noise regularly (music, machinery, firearms), get tested annually. If you already have hearing loss or use hearing aids, get checked every year to monitor changes. For children, follow-up testing is recommended if they had early hearing loss or recurrent ear infections.
Erika Sta. Maria
November 20, 2025 AT 19:35Debanjan Banerjee
November 21, 2025 AT 05:15Steve Harris
November 23, 2025 AT 00:33Elaina Cronin
November 24, 2025 AT 11:01Willie Doherty
November 24, 2025 AT 23:36Darragh McNulty
November 26, 2025 AT 20:14Sandi Moon
November 28, 2025 AT 02:45Chris Vere
November 28, 2025 AT 07:00Pravin Manani
November 28, 2025 AT 15:28Mark Kahn
November 30, 2025 AT 09:31Leo Tamisch
November 30, 2025 AT 23:48Daisy L
December 1, 2025 AT 18:10Clifford Temple
December 2, 2025 AT 02:36