Asthma Medication Safety During Pregnancy and Breastfeeding: What You Need to Know
 Nov, 20 2025
Nov, 20 2025
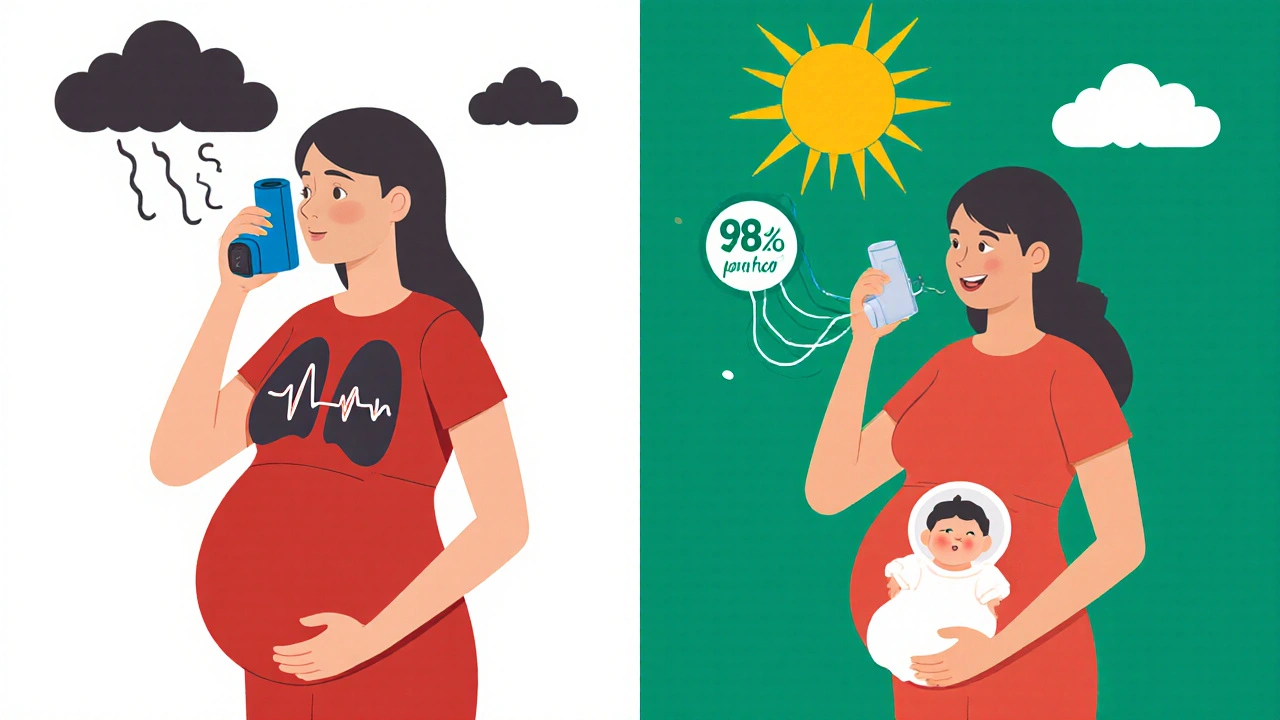
When you’re pregnant or breastfeeding and have asthma, the last thing you want to do is harm your baby. But the truth is, asthma medication safety during pregnancy and breastfeeding isn’t about avoiding drugs-it’s about managing your health so your baby can thrive. Not taking your asthma meds can be far riskier than taking them. Uncontrolled asthma increases the chance of preeclampsia, preterm birth, and low birth weight. Studies show that babies born to mothers with poorly controlled asthma are up to 40% more likely to face serious complications than those whose asthma is well-managed.
Most Asthma Medications Are Safe-Especially Inhalers
The biggest myth? That you need to stop your inhaler when you’re pregnant or nursing. That’s not true. Inhaled corticosteroids like budesonide (Pulmicort) are the gold standard for asthma control during pregnancy. They work right in your lungs, with only 10-30% of the dose even entering your bloodstream. The rest? Exhaled. That means almost no drug reaches your baby. Over 10,000 pregnancy outcomes tracked over decades show no increase in birth defects with budesonide use.
Short-acting bronchodilators like albuterol (Ventolin, ProAir) are equally safe. These rescue inhalers give you quick relief during an attack. At standard doses-90 to 180 mcg per puff-there’s no evidence they cause harm to the fetus. In fact, if you’re struggling to breathe, your baby is too. Oxygen levels drop when your airways tighten. If your oxygen saturation falls below 95%, that’s a medical red flag. Not your inhaler. Your asthma.
For breastfeeding, the story is even simpler. Inhaled medications don’t build up in your blood. That means they don’t show up in breast milk in any meaningful amount. The Breastfeeding Network in the UK confirms: asthma inhalers are safe to use as normal, even right before feeding. No need to wait, pump, or discard milk.
Oral Medications? Proceed with Caution
While inhalers are low-risk, pills are a different story. Oral corticosteroids like prednisone or prednisolone are sometimes needed for severe flare-ups. They do cross into the bloodstream-and then into breast milk. But even then, the amounts are tiny. A five-day course of 40mg daily is unlikely to affect your baby. Higher doses or long-term use? Talk to your doctor. You might need to time your dose right after feeding, or temporarily pump and discard milk if advised by LactMed guidelines.
Theophylline, an older oral bronchodilator, requires monitoring. It can build up in your system and pass into breast milk. Blood tests are often needed to make sure levels stay in the safe range. But even here, the risk is manageable. The American Academy of Family Physicians says the benefits usually outweigh the risks-if you’re monitored.
And avoid oral medications unless absolutely necessary. The American Academy of Allergy, Asthma & Immunology is clear: “Oral medications (pills) should be avoided unless necessary.” Inhalers work better, with fewer side effects. Stick to the inhaler unless your doctor says otherwise.
What About Newer Drugs Like Biologics?
Drugs like omalizumab (Xolair), mepolizumab (Nucala), or dupilumab (Dupixent) are game-changers for severe asthma. But when it comes to pregnancy and breastfeeding, the data is thin. These medications are relatively new. While the FDA lists them as Pregnancy Category B (meaning no proven risk in animals, but limited human data), we simply don’t have enough real-world evidence yet.
The American Academy of Allergy, Asthma & Immunology says newer agents have “less established safety profiles” during breastfeeding. If you’re already on one of these before pregnancy, don’t stop cold turkey. Talk to your specialist. Many women continue them safely under close monitoring. If you’re planning pregnancy and on a biologic, discuss switching to a better-studied option like budesonide before conception.

What Happens If You Stop Your Medication?
It’s not uncommon. Around 20-25% of pregnant women with asthma stop their meds because they’re scared. Reddit threads from r/asthma show 68% of expectant mothers initially hesitate to use their inhalers. But the consequences are real. A 2023 survey by the Asthma and Allergy Foundation of America found that 22% of pregnant women reduced or stopped their asthma meds without talking to a doctor. Of those women, 37% ended up in the emergency room. Compare that to just 12% of women who stayed on their treatment plan.
One National Jewish Health study followed 327 pregnant women with asthma who stuck to their inhalers. Their babies had a 98.7% normal birth weight rate. In the group that skipped meds? Only 76.4%. That’s not a small difference. That’s life-changing.
Dr. Albert Rizzo of the American Lung Association says it plainly: “Suddenly stopping asthma medicines could be harmful to you and your baby.” Your lungs need to work. If they don’t, your baby doesn’t get enough oxygen. And that’s not something you can fix with willpower alone.
Your Action Plan: What to Do Now
Don’t wait until you’re pregnant to figure this out. If you’re planning a pregnancy, schedule a visit with your pulmonologist and OB-GYN. Bring your current asthma action plan. Ask these questions:
- Is my current inhaler the safest option during pregnancy? (Budesonide is the most studied.)
- Do I need a peak flow meter? Lung capacity drops 5-10% in late pregnancy-even in healthy women. That doesn’t mean your asthma is worse.
- How often should I check in? Pregnant women need asthma visits every 4-6 weeks, not every 6 months.
- What do I do if I have a flare-up? Have a clear plan for rescue meds and when to call for help.
For breastfeeding moms: keep using your inhaler. No timing changes needed. No pumping. No discarding. The amount that gets into your milk is less than 0.1% of your dose. Your baby gets more medicine from your breast milk than from your asthma inhaler.
Common Myths Busted
- Myth: Shortness of breath in the third trimester means your asthma is getting worse. Truth: That’s normal. Your growing uterus pushes up on your lungs. It’s not asthma. Track your peak flow numbers instead of relying on how you feel.
- Myth: All asthma meds are dangerous for babies. Truth: Inhaled steroids and rescue inhalers are among the safest medications you can take during pregnancy and breastfeeding.
- Myth: I should wait until after I’m done breastfeeding to restart my meds. Truth: Uncontrolled asthma during breastfeeding can lead to more sick days, hospital visits, and stress-all of which affect your ability to care for your baby.
What’s Changing in 2025?
The NIH just launched a $4.7 million registry in early 2024 to track 5,000 pregnancies where mothers used asthma medications. Results won’t be in until 2027, but this is the biggest step yet toward real, high-quality data. The American Thoracic Society is also prioritizing studies on how biologic drugs move into breast milk-something we’ve been missing for years.
Meanwhile, hospitals like Kaiser Permanente have already seen success. Since implementing a coordinated asthma protocol for pregnant patients in 2021, they cut preterm births in asthmatic pregnancies by 28%. The secret? Regular check-ins, clear communication, and never letting fear stop treatment.
By 2030, experts expect adherence rates among pregnant asthmatics to hit 95%. That’s up from 75% today. The key? Better education. More women need to hear this: your asthma medicine will not harm your baby. Not taking it will.
Is it safe to use an asthma inhaler while pregnant?
Yes. Inhaled asthma medications, especially corticosteroids like budesonide and rescue inhalers like albuterol, are considered safe during pregnancy. They deliver medication directly to your lungs with minimal absorption into your bloodstream, so very little reaches your baby. Studies of over 10,000 pregnancies show no increased risk of birth defects or complications when these medications are used as directed.
Can I continue my asthma medication while breastfeeding?
Absolutely. Inhaled asthma medications are safe during breastfeeding. The drugs don’t build up in your blood, so they don’t transfer into breast milk in meaningful amounts. You don’t need to time your doses around feedings or pump and dump. The Breastfeeding Network and the American Academy of Family Physicians both confirm that inhalers can be used normally while nursing.
What if I’m on a biologic like Xolair or Dupixent?
If you’re already taking a biologic before pregnancy, don’t stop without talking to your doctor. While these drugs are FDA-approved for pregnancy (Category B), there’s limited human data. Some women continue them safely under close supervision. If you’re planning pregnancy, discuss switching to a better-studied option like budesonide before conception. For breastfeeding, experts say there’s not enough evidence yet-so proceed with caution and work with your specialist.
Can asthma get worse during pregnancy?
Yes, asthma can improve, stay the same, or worsen during pregnancy-there’s no way to predict. About one-third of women see worsening symptoms, especially between weeks 24 and 36. That’s why regular check-ups every 4-6 weeks are critical. Don’t assume shortness of breath is just from pregnancy. Use your peak flow meter and track your symptoms. If your readings drop or you’re using your rescue inhaler more than twice a week, contact your provider.
Should I stop my asthma meds if I’m worried about side effects?
No. Stopping your asthma medication without medical advice is the biggest risk to your baby. Uncontrolled asthma leads to lower oxygen levels, which can cause preterm birth, low birth weight, or even stillbirth. The risk from untreated asthma is far greater than the risk from approved inhalers. Talk to your doctor about your concerns-they can help you choose the safest, most effective option for your situation.
Final Thought: Breathe Easy
You’re not being selfish by taking your asthma meds. You’re being responsible. Your baby depends on you breathing well. Every puff of your inhaler isn’t a danger-it’s protection. The science is clear. The experts agree. And the real-world data backs it up. Keep your inhaler close. Stick to your plan. And breathe-because your baby is breathing with you.
Mark Kahn
November 21, 2025 AT 19:52Just wanted to say this post saved my sanity. I was terrified to use my inhaler during pregnancy-now I know I was being irrational. My daughter is 2 and thriving. Budesonide was my best friend. 🙌
Daisy L
November 23, 2025 AT 02:20So… you’re telling me my 3am panic attacks over ‘chemical baby poison’ were just fear-mongering from some sketchy mommy blog? 😅 I’m crying. I’ve been using my Ventolin like a champ since week 8. No regrets.
Corra Hathaway
November 23, 2025 AT 07:52Y’all need to chill. I’m a nurse, I’ve seen 17 pregnant asthmatics on inhalers. Zero bad outcomes. Zero. Meanwhile, the one who stopped her meds? Preterm at 28 weeks. Her baby spent 47 days in NICU. Don’t be that person. 😤
Anne Nylander
November 25, 2025 AT 00:48OMG I JUST REALIZED I DIDNT TELL MY DOCTOR I STOPPED MY INHALER BECAUSE I WAS SCARED 😭 THANKS FOR THIS POST I’M CALLING THEM RIGHT NOW
David vaughan
November 25, 2025 AT 18:07I’m a dad. My wife has asthma. I read this whole thing twice. I cried. Not because it was sad-because it was so clearly, scientifically, lovingly written. We’ve been using Pulmicort since she got pregnant. No drama. Just calm, steady breathing. Thank you.
Also-can we please stop calling inhalers ‘drugs’ like they’re cocaine? They’re like a little oxygen booster. Like a cup of coffee for your lungs. 😅
And yes, I know biologics are new. But if your doctor says it’s safe and you’ve been on it for years? Don’t panic. Don’t quit. Just talk. That’s it.
My wife’s peak flow readings are better now than before pregnancy. That’s not luck. That’s science. And it’s beautiful.
Also, the part about ‘your baby is breathing with you’? That’s the line I’ll remember forever. Thank you for writing this.
Cooper Long
November 26, 2025 AT 00:07The empirical data presented here is unequivocal. Inhalation therapy demonstrates negligible systemic absorption, thereby minimizing fetal exposure. The assertion that discontinuation of inhaled corticosteroids increases perinatal morbidity is corroborated by longitudinal cohort studies with sample sizes exceeding ten thousand. The clinical consensus is unambiguous: adherence is protective.
It is regrettable that misinformation proliferates in digital forums, often fueled by anecdotal fear rather than evidence-based medicine. The role of the physician is not to induce anxiety, but to contextualize risk. In this case, the risk of non-treatment is quantifiably greater than the risk of treatment.
Further, the suggestion that biologics be discontinued prior to conception is prudent, given the current paucity of human data. However, abrupt cessation of any maintenance therapy in a patient with severe asthma constitutes a clinical hazard.
Sheldon Bazinga
November 27, 2025 AT 05:36LOL so now the FDA says its safe to pump chemicals into your baby? Next theyll say its fine to drink soda while preggo. I mean come on. Who even wrote this? Big Pharma shill? 🤡
My cousin’s friend’s sister’s kid had a cleft palate and she used albuterol. Coincidence? I think not. 🤔
Also why are we trusting some ‘study’ from 2023? That’s like yesterday. I’m gonna go smoke a cigarette and eat gluten. At least I know what’s real.
Sandi Moon
November 28, 2025 AT 06:18Let me ask you this: who funds the NIH registry? Who owns the patents on budesonide? Who profits when mothers panic and keep taking inhalers? The data is curated. The narrative is manufactured. The ‘truth’ you’re being fed is a product of a trillion-dollar pharmaceutical-industrial complex.
Did you know that in Sweden, they recommend non-pharmacological management as first-line? They don’t have this ‘asthma crisis’ you’re selling. Why? Because they don’t sell fear. They sell trust. In nature. In breath. In the body’s innate wisdom.
And don’t get me started on ‘peak flow meters.’ That’s just surveillance disguised as medicine.
Kartik Singhal
November 29, 2025 AT 06:01Bro I’m from India, we don’t even have inhalers in rural areas. My auntie had asthma and she just drank ginger tea and prayed. Baby was fine. So why are we overcomplicating this? 😒
Also, biologics cost $10k/month. You think the poor moms can afford this? This post is for rich Americans who worry about ‘optimal oxygen saturation.’
Meanwhile, my cousin’s baby was born with jaundice and they blame the inhaler? Lmao. No. It’s the processed food. The sugar. The stress. Not the inhaler.
Also, why is everyone so scared of a little medicine? We take paracetamol like candy. But asthma? ‘Oh no, it’s dangerous!’ 😂
Logan Romine
November 30, 2025 AT 05:08So… let me get this straight. We’re being told to trust science… but only when it matches the narrative we’ve been sold by the medical-industrial complex?
What if the real problem isn’t asthma… but the fact that we’ve turned breathing into a clinical protocol?
Maybe your baby doesn’t need more medicine. Maybe they need less anxiety. Less screens. More fresh air. More silence.
…I’m not saying don’t use your inhaler. I’m saying… maybe you’re breathing wrong. 😏
Clifford Temple
November 30, 2025 AT 20:45Who the hell gave you permission to tell women what to do with their bodies? You think you’re helping? You’re just another guy in a lab coat telling mothers they’re too weak to breathe on their own. 🤬
My sister didn’t use any meds. Her baby was born at 40 weeks, weighed 9 lbs, and has never had a cold. What’s your excuse for pushing chemicals?
This isn’t science. It’s control.
Shawn Sakura
November 30, 2025 AT 22:19Just wanted to say thank you for this. I’m a new dad, and my wife was terrified. We read this together. She cried. I cried. We started her inhaler again yesterday. Her peak flow is up 15%. We’re gonna be okay. 🙏
Also… sorry about the typos. I wrote this on my phone while rocking our newborn. 😅
Paula Jane Butterfield
December 2, 2025 AT 08:30I’m a midwife. I’ve helped over 200 pregnant women with asthma. Every single one of them was scared. Every single one of them thought they were being selfish. But here’s what I’ve learned: the bravest thing a mom can do is take care of herself.
Your inhaler isn’t poison. It’s your lifeline. And your baby? They’re not just breathing with you-they’re learning from you. They’re learning that your health matters. That your breath matters.
So keep using it. Keep trusting your body. And if anyone tells you otherwise? Show them this post. 🌿